Tooth root removal can be very simple or very complex. It all depends on the patient’s condition, his teeth and jaw bones. If the bone has partially resolved, then only a first-year medical student will not be able to cope with the operation. It’s another matter if the root of the tooth is fractured as a result of mechanical damage, or if it is intact but located deep in the alveolus. Mechanical damage can be caused by trauma (strong impact), or improper previous treatment.
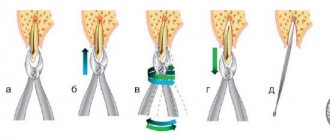
The operation to remove a tooth root from the upper jaw has its own specifics; procedures vary depending on the type of tooth (incisors, canines, chewing teeth). The surgeon uses various tools to remove the roots of teeth: S-shaped, bayonet-shaped forceps. The latter are especially actively used when removing tooth roots from the upper jaw. In some cases, before the actual removal of the tooth root, it is divided into parts (usually using a drill). Tooth root removal is different from the process of removing an entire tooth and is usually more labor intensive.
Some patients ignore surgery to remove the root of the tooth if the crown part is no longer there. Motivation varies - usually the patient expects that the remaining tooth will come out on its own over time. Indeed, tooth fragments tend to come out on their own, but the root is not a fragment. It is often observed that the patient comes with an already drawn-out root - then it is necessary to make an incision in the gum to gain access to it. The root of the tooth itself, if not removed in a timely manner, can provoke severe pain and inflammation. Remember: the tooth root does not dissolve!
Many Moscow clinics take on any, even the most complex cases. The experience and qualifications of doctors - specialists with extensive experience - will not allow them to complicate the operation themselves by causing mechanical damage to the tooth root or making mistakes when removing it. But they can correct other people's mistakes. Tooth root removal can be performed with forceps, elevators, or, when previous techniques have failed, by sawing.
Removing the root of a tooth in the upper and lower jaws has technological differences. For different teeth (canines, incisors, chewing teeth), forceps of different shapes (straight, S-shaped, bayonet-shaped) and elevators (working on the principle of a lever) are used. The procedure itself is performed under local or general anesthesia. The dentist will choose a method for removing the roots of the teeth, and anesthetic agents are selected in such a way as to eliminate the likelihood of side effects (individual intolerance, allergic reactions).
If the root of the tooth is already overgrown, you will have to open it by cutting into the gum. This operation is also performed under anesthesia. After surgery, stitches may be placed and special medications may be used to speed up gum healing. Doctors will remove the root of any tooth, regardless of why only the crown was removed. Painless, fast, high quality.
The main causes of pathology
There are a number of main reasons why a tooth can become overgrown with soft tissue. The most common reason is negligence towards periodontal tissues, refusal to visit the clinic after breaking off part of the crown. There are also quite often cases when a wisdom tooth that has not fully erupted is covered with gum on top. In the future, this figure eight can exert strong pressure on the entire dentition, which will lead to a gradual change in the bite and the appearance of serious orthodontic pathologies.
The patient may also encounter a similar situation when refusing to remove the root system of a broken tooth. As a result, a small piece of the top, as well as the root, remains under the gum, and over time they can begin to hurt and become inflamed.
It is important to note that a person’s bad habits, poor diet, consumption of junk food, chronic diseases and lack of oral hygiene can lead to teeth becoming more sensitive and brittle. As a result, the slightest pressure will be enough to cause part of the crown to break off.
When is tooth root removal required?
Dentists prefer to resort to such radical methods as rarely as possible and try to keep the dentition “alive.” Even if a small fragment remains, the possibility of prosthetics using the preserved base is first considered. In some cases, extraction cannot be done without.
Indications:
- The patient is diagnosed with periodontitis in the later stages, when the root part is severely loosened;
- serious injury (fracture);
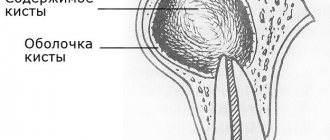
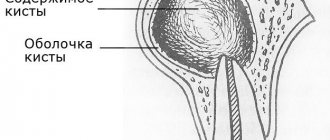
- a cystic neoplasm has been discovered that cannot be eliminated in isolation;
- a piece of the crown broke off, extending deep into the gum tissue;
- solid particles remained after poor-quality doctor intervention.
How is a tooth root removed in dentistry in children? Is this necessary? Milk units normally fall out on their own. They are indicated to be pulled out in cases of deep carious lesions, fractures, loosening and subgingival caries.
What happens if you leave
Some people can walk for several years with their teeth completely destroyed. This is very harmful, because the remaining root part rots and is a source of foul odor from the mouth. In addition, this is a hotbed of numerous infections, because the roots accumulate pathogenic microorganisms and food particles. Dense plaque and tartar form on the fragments. As a result, soft tissues become inflamed.
The body will constantly fight the source of the problem; the immune system will direct a significant part of its resources to the fight. Sooner or later, a severe inflammatory process develops; in the most severe cases, the maxillary sinuses become infected, osteomyelitis develops, and fractures and other injuries are possible.
Patients mistakenly believe that over time the root will come out on its own, so dental intervention is not necessary. The root part does not fall out, over time it will become overgrown, and the doctor will have to cut the gum for high-quality extraction. In this case, the rehabilitation period may be delayed.
Consequences
If the root and part of the tooth are left inside the gum tissue, some complications may occur. Inflammation in the pulp chamber can begin as a result of dirt and infection; this process is accompanied by severe pain, the appearance of purulent discharge, rotting, etc. To avoid sepsis, surgical removal of the root and nerve endings is recommended.
Another dangerous disease is periodontitis. In the absence of timely treatment, the unit can become very loose; it is surrounded by voids where germs, food particles, and infection can get in. In this case, the root moves away from the coronal part quite quickly and it becomes almost impossible to save it. If the problem is not corrected in time, there is a high risk of damage to other organs and even blood poisoning. The latter threatens with very serious complications and is dangerous to human health.
Another common occurrence is when a previously filled tooth breaks and particles of the composite get into the hole. These particles can react with tissues, which leads to the development of inflammation. In this case, not only the root of our broken tooth can become inflamed, but also nearby units. If inflammation is left unattended by a specialist for a long period of time, a cyst may appear.
How long does it take for gums to heal after tooth extraction - timing
How long it takes for the gums to heal after tooth extraction depends on many factors: the degree of trauma of the removal, whether sutures were applied, the possible addition of infectious inflammation of the socket, and the age of the patient. Healing of the hole after tooth extraction can be divided into partial and complete.
Partial epithelization of the wound occurs on average in 12 days (Fig. 5), but complete epithelization of the surface of the clot is observed in 20 to 25 days (Fig. 6). However, if inflammation of the socket occurs or after a complex tooth extraction, which is usually accompanied by major bone trauma, the healing time may increase by several days.
Reasons for slow healing –
- significant trauma to the bone and gums during removal (both due to the doctor’s indifference and as a result of sawing out the bone around the tooth with a drill during difficult removal),
- when a clot falls out of the socket (empty socket),
- development of alveolitis of the socket,
- the doctor left fragments or inactive fragments of bone tissue in the socket,
- if sharp bone fragments protrude through the mucous membrane,
- if the gum mucosa around the hole is very mobile, and the doctor did not apply stitches,
- antibiotics were not prescribed after a complex removal,
- patient's age.
What to do
Of course, you shouldn’t sit and wait for the pain and discomfort in the area of a tooth overgrown with gums to go away on its own. It is best to immediately contact a specialized dental clinic for medical advice. Only he will be able to conduct a comprehensive examination of the oral cavity, prescribe the necessary tests, conduct an X-ray examination and prescribe the correct treatment.
As a rule, a broken tooth that is overgrown with soft tissue is carefully removed. This requires making an incision in the gum. If the tooth is healthy, then after opening the hole the doctor can install an artificial root and prosthesis into it.
If it is not possible to save the tooth, then a procedure is performed to extract its root system. To do this, the specialist uses a special tool called an elevator, with which he cuts the top of the unit and gradually brings it to the surface. Such manipulations are carried out under local anesthesia and do not take much time. After extraction of a diseased tooth, a medicinal drug can be applied to the wound, which promotes faster healing. The stitches are removed after a few weeks.
What does white plaque mean after tooth extraction?
Some patients notice that their gums turn white after tooth extraction. In the normal course of events, a whitish coating is nothing more than an “effusion” of fibrin from the blood, and indicates the beginning of epithelization of the wound. White plaque after tooth extraction usually appears on the surface of a blood clot (Fig. 8), as well as on the surface of a severely injured mucous membrane.
White plaque on the gum after tooth extraction -
In this case, the gum surrounding the socket has a pale pink color, when pressing on the gum there should be no purulent discharge (as in the video below), there should be no unpleasant odor from the socket, constant aching pain or pain when responding to cold and hot water (24stoma.ru) .
What can happen if you refuse the help of a specialist?
If the tooth root remains under the layer of gum tissue, decay can spread to neighboring units. In this case, treatment will be longer and more expensive. The main symptoms of this problem are a strong odor from the mouth and periodic pain that radiates to the head. Harmful microorganisms will begin to accumulate under the gums, which can lead to the development of caries.
In 99% of cases, the patient has a small sac with purulent filling at the apex of the root. After some time, it inevitably turns into a painful swelling called gumboil. The only correct solution when gums grow on a tooth is to quickly contact an experienced dentist. It will not only eliminate inflammation, but will also be able to save the destroyed unit.
previous post
What happens if you swallow toothpaste?
next entry
Who to contact
The NovaDent dental network in Moscow and the Moscow region offers the services of experienced, reputable doctors. Removal of the roots of the teeth of the lower and upper jaw is carried out under sterile conditions, in compliance with all rules of procedure and hygiene. Sign up for a free consultation and we will select the optimal treatment plan for you at an affordable price.
Expert of the article you are reading: Kuzmenko Viktor Valerievich Orthopedist, surgeon, leading specialist of the NovaDent network
17 years
Clinical experience
Krasnogorsk
Moscow region, Krasnogorsk, Podmoskovny Boulevard, 5
+7
Free consultation with this specialist
Final provisions
When a doctor diagnoses pericoronitis, it means that the gums around the erupting teeth - permanent or baby - have become inflamed, and the tooth is probably not growing properly. The abnormality creates a pocket called a hood between the new tooth and the soft tissue. The cavity quickly fills with a substrate consisting of plaque and bacteria, and decay begins. The main symptom is pain at the site of the growing tooth; in addition, other signs are present.
Pericoronitis is treated by removing the inflamed soft tissue (hood), or extracting the tooth (in extreme cases). Home methods, rinses, lotions will not help, they can only do harm if you rely on them completely and do not visit the hospital.
Treatment of pericoronitis can be quick - in the early stages, and long and painful - in advanced stages. A person can prevent the development of pathology while complying with hygiene standards. And it is worth remembering that modern dentistry is a very rapidly developing branch of medicine. Trust the professionals to help you maintain your health.
Treatment of pericoronitis of the wisdom tooth in the lower jaw
Mistakes and complications in the treatment of dental pulpitis
Cervical caries on the front teeth: causes and treatment
Restoration of tooth enamel, price, drugs
Root canal treatment for chronic periodontitis
Dental treatment without pain in Moscow
Repeated endodontic treatment of tooth canals for pulp inflammation
Prevention of pericoronitis
Therapy for a disease, especially one that is advanced or susceptible to relapse, can be time-consuming and expensive, and the patient constantly lives with pain. It is easier to prevent such problems by following the rules of oral care:
- Try to visit the dentist at least once a year, or better yet, once every six months. The disease is well recognized at an early stage and is easily treated.
- Practice daily oral hygiene. Clean plaque from your teeth and tongue, and don’t be shy to look at your own teeth in the mirror.
- Don't experiment with toothbrushes and toothpastes if your teeth tend to hurt frequently. Let your doctor recommend the care products.
- Consider purchasing a waterpik. Talk to your doctor and listen to professional advice on choosing a device.
- If any type of inflammation develops in the oral cavity, go to the clinic. Not a single folk recipe will help get rid of pericoronitis and other dental diseases, and time for quick help can be missed.
Hyperplasia
What is the main reason for tooth overgrowth with gums? In most cases, this is associated with the development of a phenomenon such as hyperplasia, that is, excessive proliferation of tissue cells. Otherwise, this process may be called hypertrophy. Unfortunately, this process is not entirely harmless, but appears against the background of the development of a focus of inflammation.
Another reason for hyperplasia is a malfunction of the endocrine system, that is, a hormonal imbalance, as well as a disruption of metabolic processes in the body. In this case, the gums can begin to grow uncontrollably, greatly increase in volume and bleed at the slightest touch. The last stage of pathology is complete overlap of the gum crown part of the tooth.
Children can also experience a similar phenomenon; this usually occurs during teething, as well as during the change from milk units to molars. Sometimes we are not talking about hyperplasia, but about banal inflammation of the tissue at the site of the appearance of a new tooth. However, an accurate diagnosis must be made by a dentist.
Tooth root removal under anesthesia
In most situations, local anesthesia is used. However, in cases where we are talking about the extraction of “eights”, or in cases of intolerance to the components of the drugs, or a pathological fear of dental treatment, general anesthesia is resorted to. Throughout the entire procedure, the person sleeps, so he does not feel pain or psychological discomfort.
Despite the tangible advantages, this technique has a significant drawback. Its use can lead to serious problems with the heart, brain and other internal organs and systems. Some patients have difficulty recovering from anesthesia and experience nausea, headaches and other symptoms.
In modern dentistry, a more gentle method is used - sedation. The person relaxes, but is conscious and can interact with doctors. There is no stress or pain.
The gum former fell out: what to do?
It is also possible that the former becomes unscrewed and falls out of the implant. This may occur due to a loose fit of the element to the titanium root. This happens when the surgeon secured the implant too deep into the bone, and bone tissue grew on it, making it impossible to secure the former tightly. To correct this deficiency, you need to visit a doctor. When the gum former has already fallen out, the first thing you should do is carefully screw it into place and make an appointment with the dentist. Without a plug for a long time, the hole may become overgrown.
Excision of the hood
This is the most commonly used technique in eliminating the consequences of pericoronitis. Intervention, especially in the early stages, is minimal, and rehabilitation is never long or painful. Operation stages:
- An injection of an anesthetic is given;
- The dentist uses a scalpel to remove the gingival hood;
- The resulting wound is disinfected with disinfectants.
The doctor will continue to provide therapeutic support to the patient for a number of weeks. A person will make special healing baths for the oral cavity at home based on a water-salt solution, and then come to the clinic for follow-up examinations. In some cases, antibiotics are prescribed if the doctor notices bad activity of pathogenic bacteria on the teeth. It happens that the hood recurs and returns again, covering the problematic tooth. In this case, there is no other choice but to remove the source of trouble.
How to restore a damaged tooth?
If the root is preserved, it is possible to carry out tooth restoration, which is the restoration of its previous shape using artificial materials. The tissue of such a tooth will not be alive, but it looks natural and has high strength characteristics. Modern materials used to restore damaged teeth include veneers and composite filling materials that have a natural tint that does not make the artificial tooth stand out from the background of the previous ones.
Removal steps
Before you pull out the root of a tooth, you need to prepare for this. The procedure is carried out in several successive steps. All of them are mandatory and, subject to medical recommendations, as well as general rules, guarantee a good result and quick recovery.
Preparing for removal
At the preparatory stage it is necessary:
- It is good to examine the oral cavity, especially near the pathological area. A panoramic photograph should be taken, the condition of the periodontal soft tissues should be assessed, and the presence of an inflammatory process should be confirmed or refuted.
- Develop a therapeutic regimen together with your doctor.
- Select pain relief methods and specific medications, taking into account contraindications and individual characteristics of the body.
- Prepare the necessary equipment.
- Perform hygienic treatment of the oral cavity, remove plaque and stone.
- Rinse your mouth with an antiseptic solution. Chlorhexidine is most often used for this.
- Do not neglect anesthesia.
- If necessary, cut the gum.
Proper preparation is a guarantee of a successful procedure. In this way, possible complications can be minimized as much as possible.
Tools
Dentists, before pulling out, remove the root of the molar tooth from the gum, select special devices, without which high-quality extraction is impossible. The doctor comes to the aid of:
- Forceps. They capture the visible part protruding above the surface of the gums. The periodontium is first separated from the root system, and the mucous membranes are peeled off from the boundaries of the alveoli. Dental units from the upper jaw are pulled out with a tool with wide bayonet-shaped blades, and from the lower jaw - with wedge-shaped models.
- Elevator. It is used as a lever, first inserted into the cavity between the walls of the hole and the root body. Used when the root part is deep, when forceps are powerless.
- Drill. Using a bur, the outer alveolar wall is removed, and the remains are removed with forceps.
Extraction methods
There are several methods that dentists resort to:
- Amputation. Indicated if surgical intervention on the upper jaw is necessary. The visible periodontal layer is mechanically separated, the drill trims the root system, which is then removed with forceps. The empty hole is filled with a special composition.
- Hemisection. Most often used on mandibular molars. The doctor takes out the diseased root and the coronal part that is adjacent to it. After this, filling is performed.
- Cystectomy. Indicated for cystic neoplasms. First, the upper section is opened, the cyst is excised, and the resulting void is filled with medical composition.
Regardless of the method chosen, local anesthesia is used. The patient will not feel pain or other discomfort.
Further processing of the alveoli
This is a mandatory step after extraction of a dental unit. The hole must be thoroughly washed with an antiseptic solution, then anti-inflammatory drugs are placed in it for the purpose of prevention or for treatment if inflammation does appear. In this case, the wound will heal much faster.
Features of tooth root extraction in different jaws
When removing fragments from the upper and lower dentition, there are some differences in the instruments used and the manipulations performed. From above, molars, canines and incisors are removed with bayonet-shaped forceps and C-shaped pliers. The dentist performs rotational movements and pulls out the tooth. When difficulties arise, a drill or elevator is used.
With the lower jaw everything is much simpler. Typically, curved dental forceps are sufficient. The exception is when “eights” are removed.
Is it possible to put a crown on a decayed tooth?
An important condition must be met here - the root should not have any damage. If the tooth is destroyed below the gum level, you will most likely have to contact a surgeon. The crown is permanent, and the tooth underneath must remain healthy. If there is injury, the root of the tooth may begin to rot, causing infection and severe pain.
If the area above the gum is intact, the doctor determines whether the damaged tooth can be restored. If the answer is positive, he will do everything possible to save the tooth, because the natural root tissue is much stronger. A good dentist always strives to save the root, and modern medicine offers effective methods for restoring even severely damaged teeth.
Diagnosis of pericoronitis
Pain in the teeth, the main symptom of pericoronitis, does not directly indicate the disease. This symptom is considered common to dozens of other dental diseases. Only a doctor can make a diagnosis in person.
When examining a patient, the dentist will ask about the nature of the pain, its frequency and duration. This will be followed by a mandatory examination of the oral cavity, perhaps the doctor will use instruments: somewhere he will knock on the teeth, somewhere he will apply a little pressure. If the picture seen remains unclear to the specialist, he will send the person for an x-ray. However, in the vast majority of cases, the doctor immediately determines pericoronitis in the patient, and additional research is carried out when the disease is adjacent to other dental pathologies.
Treatment of acute pericoronitis
Treatment of the disease is usually carried out in two ways: removing the hood or removing the tooth. Adherents of unconventional methods of treatment and grandmother's recipes should be reminded that not a single dental disease can be cured using traditional methods. The use of decoctions, tinctures and other methods can only alleviate the symptoms, but without consulting a specialist, it is very easy to let the disease progress until a serious health situation develops. Therefore, going to the clinic is mandatory.