Hypertrophy of pharyngeal lymphoid tissue
For hypertrophy of the palatine tonsils, physical methods, climatic and restorative treatment are used. If there is a sharp increase in the palatine tonsils and conservative therapy is unsuccessful, they are partially removed (tonsillotomy), in most cases simultaneously with the removal of the adenoids. The operation is performed on an outpatient basis under local anesthesia. After applying a tonsillotome to the part of the tonsil protruding from behind the arches, it is fixed with a fork and quickly removed. The postoperative regimen and prescriptions are the same as after adenotomy. The disadvantages of tonsillotomy include incomplete removal of the tonsil, especially when hyperplasia and inflammation of the tonsil are combined. The most common complications include bleeding, suppuration of the surgical wound, cervical lymphadenitis, and injury to the soft palate. Conservative treatment of adenoids is usually ineffective, and the physiotherapeutic procedures used in this case help to stimulate their growth. Timely removal of adenoids (adenotomy) eliminates the irritating effect of infected mucus from the nasopharynx on the tonsils, nasal breathing is restored, which often leads to shrinkage of the tonsils. Indications for adenotomy: frequent colds, severe disruption of nasal breathing, hypertrophy of the II and III degrees of adenoids (and if the ear is affected, also grade I adenoids, since it is necessary to free the mouth of the auditory tube), recurrent and chronic tracheobronchitis, pneumonia, bronchial asthma, recurrent and chronic diseases of the paranasal sinuses, hearing loss, secretory, recurrent and chronic otitis media, speech impairment, psychoneurological and reflex disorders (enuresis, epileptiform disorders). Contraindications to adenotomy: acute infectious diseases, their precursors or contact with patients with childhood infections. After a sore throat, an acute respiratory disease, surgery can be done after 1 month, after the flu - after 2 months, after a preventive vaccination - after 2-3 months, after chicken pox - after 3 months, after rubella, scarlet fever - after 4 months, after measles, whooping cough , mumps, infectious mononucleosis - after 6 months, after infectious hepatitis - after 1 year (after a blood test for bilirubin), after meningitis - after 2 years. Contraindications are also blood diseases (acute and chronic leukemia, hemorrhagic diathesis, immune hemopathy), carriage of toxigenic measles, non-bacteria diphtheria, acute diseases of the ENT organs or exacerbation of chronic diseases, acute diseases of internal organs or exacerbation of chronic diseases, decompensated conditions in diseases of the heart, kidneys , liver and lungs; dental caries, thymogaly, pharyngeal vascular abnormalities. Before the operation, children undergo examination, the minimum of which ensures the safety of the operation: general blood test, coagulation, bleeding time, tests to detect HIV, Australian antigen; Analysis of urine; dental sanitation, throat and nasal smear to identify toxigenic corynebacterium diphtheria bacilli; pediatrician's conclusion on the possibility of surgical intervention; lack of contact with infectious patients. The child is prescribed drugs that increase blood clotting. The operation is performed in a one-day hospital setting, under local anesthesia, using a ring-shaped knife - Beckmann's adenotom. Basket adenotome is also used. The adenotom is inserted into the nasopharynx strictly along the midline, then moved upward and anteriorly to the posterior edge of the nasal septum, and the upper edge of the instrument is pressed against the dome of the nasopharynx. In this case, the adenoid tissue enters the adenoid ring (Fig. 4.3, see color insert). The adenoid is quickly and sharply moved anteriorly and downward, cutting off the adenoids. In children, adenoid growths are often combined with hypertrophy of the palatine tonsils. In these cases, tonsillotomy and adenotomy are performed simultaneously. After 3 hours, if there is no bleeding after a follow-up examination, the child is discharged home with a recommendation of a home regimen, a gentle diet, and taking blood clotting agents and sulfonamide drugs. In recent years, endoscopic adenotomy under anesthesia has been introduced into practice, under conditions of suspended pharyngoscopy with visual control of an endoscope inserted into the posterior sections of the nasal cavity. With adenotomy, the following complications are possible: anaphylactic reaction to an anesthetic, bleeding. The severity of bleeding after adenotomy is assessed by the level of hemoglobin, hematocrit, blood pressure and pulse. If there is bleeding after adenotomy, a repeat adenotomy is performed to remove remnants of the adenoids, and general and local hemostatic measures are carried out. Complications also include suppuration of the surgical wound with the development of regional lymphadenitis, retropharyngeal, parapharyngeal abscess, mediastinitis, sepsis, asphyxia during aspiration of a removed adenoid, injury to the soft palate with the subsequent development of its paralysis and symptoms of dysphagia and dysphonia, injury to the root of the tongue, which is usually accompanied by severe bleeding, aspiration pneumonia.
Adenoid hypertrophy
Adenoid hypertrophy (adenoid vegetations/growths, hypertrophy of the nasopharyngeal/pharyngeal tonsil) is a persistent enlargement of the nasopharyngeal tonsil. It can occur either alone or in combination with hypertrophy of the palatine tonsils.
The nasopharyngeal tonsil (adenoids) is a collection of lymphoepithelial tissue in the upper part of the nasopharynx. The result of its increase is called adenoid hypertrophy, and with inflammation the process is called adenoiditis. In combination with the palatine, tubal and lingual tonsils, they form the Pirogov-Waldeyer ring, located at the entrance to the upper respiratory tract and digestive tract and acting as a local immune barrier.
Adenoid hypertrophy is most often observed between the ages of 2 and 6 years, but can also occur at a later age.
There are several classifications of adenoids according to the degree of enlargement. The most popular division is based on the doctor’s subjective assessment of the size of the tonsil during examination:
- I degree – the lumen of the choanae is blocked by 1/3
- II degree – the lumen of the choanae is blocked by 1/3–2/3
- III degree – the choanae are completely closed by adenoids.
However, just assessing the size of the tonsil is not enough; a careful history taking is an important criterion.
Causes
Hypertrophy of grade I-II adenoids at the age of 2 to 6 years is often a physiological process that is associated with the fact that the child begins to actively contact the outside world and the amygdala is subjected to constant antigenic stimulation.
Severe (or pathological) hypertrophy, which leads to the symptoms described below, can occur due to an infectious or non-infectious cause. The infectious diseases include the following:
- viral (adenovirus, Coxsackie virus, cytomegalovirus, Epstein-Barr virus, herpes simplex virus, parainfluenza virus, rhinovirus, etc.)
- bacterial (Streptococcus, Haemophilus influenzae, Moraxella catarrhalis, Staphylococcus aureus, Neisseria, Mycoplasma pneumoniae, Fusobacterium, Peptostreptococcus, Prevotella, etc.)
Non-infectious causes include gastroesophageal reflux, allergies, and prolonged exposure to cigarette smoke.
Symptoms
Symptoms of hypertrophy occur due to an increase in the size of the tonsil and/or the presence of chronic inflammatory changes in it (chronic adenoiditis). Although these processes are often related (prolonged inflammation leads to hypertrophy), it must be borne in mind that this does not always happen. For example, with adenoid vegetations of the 1st degree, there may be pronounced signs of chronic inflammation, and with vegetations of the 3rd degree there may be no clinical manifestations at all. With physiological hypertrophy, the process occurs without any symptoms or with minor manifestations.
With severe hypertrophy, the child has difficulty breathing through his nose, and therefore he breathes through his mouth, snores during sleep, sometimes with pauses in breathing (obstructive sleep apnea syndrome). Impaired ventilation of the nasal cavity leads to mucous discharge and frequent rhinosinusitis. Characterized by sneezing and bad breath. Large adenoids put pressure on the soft palate, phonation and articulation are impaired in children, children have a nasal sound. If the adenoids block the auditory tubes, this can manifest as recurrent acute otitis media, hearing loss associated with the accumulation of fluid in the middle ear (exudative otitis media). Over time, due to oxygen starvation, the child becomes lethargic, apathetic, and irritable. Memory deterioration, decreased attention, and learning difficulties occur. Sleeping with your mouth open for a long time leads to disruption of the development of the facial skeleton. The hard palate becomes high and narrow, the lower jaw becomes narrow and elongated, the bite is disturbed, which may require orthodontic treatment in the future. An experienced otolaryngologist will immediately recognize the typical “adenoid” appearance of a child.
There are acute and chronic inflammation of the mucous membrane of the nasopharyngeal tonsil:
- Acute adenoiditis is an acute inflammation caused by a viral or bacterial infection. It manifests itself as a cold: fever, difficulty in nasal breathing, serous or purulent discharge from the nose. The duration of the disease varies and does not exceed one month. In the presence of adenoid hypertrophy, phenomena characteristic of hypertrophy are added to the listed manifestations.
- Chronic adenoiditis is a chronic polyetiological disease, which is based on the disruption of local immune processes and the formation of stable microbial biofilms. It manifests itself as difficulty in nasal breathing, serous or purulent discharge from the nose, mucus running down the throat and coughing. The causes of the disease are the same as those of hypertrophy. There is no consensus on the duration of adenoiditis at which it can be considered chronic. According to various sources, at least 12 weeks must pass from the onset of the disease. This condition can occur independently and over time lead to adenoid hypertrophy.
Diagnostics
The gold standard for diagnosis in global practice and the standard of our hospital is an endoscopic examination of the nasal cavity. We carry out this study with a thin flexible fiberscope under local anesthesia.
Lateral x-rays are a common way to assess hypertrophy but can be misleading. For example, an X-ray may show a picture of grade III adenoids due to enlargement of the tubal tonsils (they are located on the sides of the nasopharyngeal tonsil), due to swelling of the mucous membrane or accumulation of thick mucus. This method is used only if endoscopy of the nasopharynx is impossible.
It is important to carry out differential diagnosis with diseases that may have similar clinical manifestations (juvenile angiofibroma, choanal atresia, polyposis, enlargement of the posterior ends of the inferior turbinates, hypertrophy of the tubal tonsils).
Treatment
Physiological hypertrophy without any manifestations or with minimal symptoms does not require treatment, but endoscopic examination is necessary for differential diagnosis.
Treatment may be conservative. It includes eliminating factors that can cause hypertrophy: allergies, gastroesophageal reflux, passive smoking. Accordingly, in some cases a multidisciplinary approach of an otolaryngologist, allergist, gastroenterologist and pediatrician is necessary. A positive effect can be had by changing the climate to a more favorable one, for example, sea climate. Topical corticosteroids have been used as an adjunctive treatment in children over the age of three, with some studies showing some benefit, but overall evidence on the effectiveness of these drugs is mixed. In acute and exacerbation of chronic adenoiditis in the case of a bacterial infection, treatment is carried out with antibiotics. Irrigation of the nasopharynx with saline solution is also used in treatment. The use of various oils, mucolytics, local antibacterial drugs, silver solutions, herbal remedies, and physiotherapy currently do not have a high-quality evidence base.
In some cases, surgical treatment cannot be avoided. Not every child needs surgery and it requires specific indications. When determining them, doctors at Ilyinskaya Hospital follow the principles of evidence-based medicine, relying on global experience. Indications include failure of conservative treatment, recurrent infections, acute otitis media and sinusitis, and an “adenoid” face. Parents should understand that long-term refusal to undergo surgery if indicated, or an attempt to “wait out” or “outgrow” adenoid hypertrophy can lead to complications, the treatment of which in the future will require a lot of time and can negatively affect the development of the child. According to the recommendations of the American Academy of Otolaryngology and Head and Neck Surgery, adenotomy should be performed in the following cases:
- In children under 4 years of age with symptoms of difficulty in nasal breathing, signs of chronic adenoiditis, as well as exudative otitis media
- In children 4 years of age and older with exudative otitis media
- If you have confirmed obstructive sleep apnea (periodic sudden decrease or cessation of breathing during sleep)
In the presence of pathology of the palatine tonsils, surgery for their resection/removal is often performed simultaneously (adenotonsillotomy/adenotonsillectomy), and in case of exudative otitis media, shunting is performed at the same time.
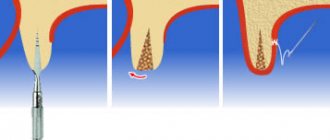
Adenotomy has undergone significant changes over time. Previously, this operation was performed under local anesthesia using a special knife (adenotome) under the control of a small mirror, and sometimes blindly. During the operation, the child experienced stress, and the surgeon may not have fully performed the operation. Nowadays, this approach is practically not used, but it is preserved in some clinics.