Author of the article:
Soldatova Lyudmila Nikolaevna
Candidate of Medical Sciences, Professor of the Department of Clinical Dentistry of the St. Petersburg Medical and Social Institute, Chief Physician of the Alfa-Dent Dental Clinic, St. Petersburg
Not only the health of teeth and gums, but also the functioning of the digestive, immune and other systems and organs depends on the state of the oral microflora. Let's figure out what this part of the body is, what affects the conditions of the oral cavity and how to quickly restore the normal functioning of the microflora.
What is the microflora of the oral cavity?
Surprisingly, approximately 160 species of microorganisms live in the mouth of a healthy person. You've probably heard that “the mouth is the dirtiest place in the body.” This statement is partly true: the oral cavity is one of the most populated parts of the human body.
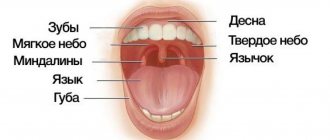
Microorganisms enter the oral cavity with food and water, as well as from the air. It is in the mouth that the most favorable conditions for the development of bacteria are observed. This part of the body always has uniform humidity and temperature (approximately 37 °C). The abundance of nutrients, sufficient oxygen content, the presence of folds in the oral cavity, interdental spaces and gum pockets, and slightly alkaline pH provoke the proliferation of various bacteria.
Microorganisms are unevenly distributed in the oral cavity. Their maximum number is observed on the surface of the teeth and on the back of the tongue. One gram of dental plaque contains approximately 300 billion microbes, and saliva contains approximately 900 million per 1 milliliter.
- 30-60% of the microflora are facultative and obligate anaerobic streptococci;
- part is occupied by Veillonella, coccobacteria, which ferment acetic, pyruvic and lactic acids to water and carbon dioxide. It is Veillonella that neutralizes acidic foods, so many dentists consider them as destroyers of cariogenic bacteria;
- Bacteria of the genera Propionibacterium, Corynebacterium and Eubacterium are also necessarily present in the mouth, which actively produce molecular oxygen, synthesize vitamin K and promote the development of obligate anaerobes. Some types of such bacteria provoke purulent inflammation.
- Lactobacilli are strict anaerobes. There are more than 10 types of similar bacteria in the mouth that form a biofilm in the cavity. The vital activity of these microorganisms creates a favorable environment for the development of normal microflora. Lactobacilli ferment carbohydrates to form lactic acid, lower the pH, and most importantly, prevent the development of pathogenic, putrefactive and gas-forming microflora.
- Rod-shaped lactobacilli in a certain amount are, like streptococci, producers of lactic acid.
- Bifidobacteria are necessary to ferment various carbohydrates, as well as produce B vitamins and antimicrobial substances that inhibit the growth of pathogenic microorganisms. Moreover, bifidobacteria are a bunch of epithelial cell receptors: they form a film that prevents the colonization of pathogenic bacteria.
It would take a very long time to list all the types of bacteria that populate the microflora of the oral cavity. It is important to understand that each person is unique, and to assess the “normality” of the microflora, you need to know the characteristics of a particular organism.
For example, in one case, a large number of lactobacilli in the oral cavity will preserve teeth, and in another, the formation of a large amount of lactic acid during their vital activity will retard the growth of other important microorganisms. The number of staphylococci, dysentery and typhoid bacilli decreases, carious processes become more active, and the microflora of the oral cavity will have to be restored.
Microbiota of the oral cavity and its connection with the occurrence of local and generalized infection
There is an opinion that the oral cavity is one of the dirtiest places in the entire human body. One can argue with this statement, but, according to scientists, saliva and oral fluid contain on average 109 microorganisms per 1 milliliter, and dental plaque contains 1011 per gram. According to the latest data, 688 species of different bacteria live in the mouth of a person who does not suffer from pathologies of the oral cavity [1].
Despite such a diversity of microbiota, with good hygiene and the absence of somatic diseases and mental disorders (such as diabetes, AIDS, constant stress and many others), we live in peace and harmony with the colonizers of the mucous membranes of our oral cavity. The presence of certain microorganisms in the oral cavity can serve as a diagnostic sign (for example, fungal diseases of the mucous membrane can be a sign of disorders of the T-cell immunity).
But, in addition to the mucous membranes, microorganisms also colonize the surface of the hard tissues of the tooth. As everyone knows, this leads to caries, and if you postpone a visit to the dentist and let the process take its course, it leads to complications such as pulpitis, periodontitis, and in the future to the formation of granulomas and cysts. Knowledge about the presence of certain representatives of the microcosm in the oral cavity, as well as about their physiological characteristics, allows us to find new ways to combat the pathologies that they can cause. The study of the oral microbiome has not lost its relevance today. Periodically, reports appear about the discovery of new representatives or the deciphering of the genomes of previously found bacteria. All this is necessary for a deeper understanding of the pathogenesis of diseases of the oral cavity, studying interbacterial interactions and improving the processes of treatment and recovery of patients, as well as the prevention of local and generalized complications.
As already mentioned, the human oral cavity normally contains a large number of different types of bacteria that do not live separately, but enter into various interactions, for example, forming biofilms. The entire microbiome of the oral cavity can be conditionally divided into two groups: permanent (species specific to a given biotope) and non-permanent microorganisms (immigrants from other host biotypes, for example, nasopharynx, intestines). A third type of microorganism may also be present—introduced microbiota from the environment.
Among the representatives of the normal microbiota, one can distinguish various types of actinomycetes (Actinomyces cardiffensis, A. dentalis, A. oris, A. odontolyticus, etc.), representatives of the genus Bacteroidetes (taxa 509, 505, 507, 511, etc.), Bifidobacterium (B. dentium, B. longum, B. breve, etc.), Campylobacter (C. gracilis, C. gingivalis, C. sputorum, etc.), Fusobacterium (F. periodonticum, F. gonidiaformans, F. hwasookii, etc.), Staphylococcus (S. warneri, S. epidermidis, etc.), Streptococcus (St. mutans, St. intermedius, St. lactarius, etc.) [1]. Despite its diversity, the species composition of the oral microbiota is quite constant, but the number of microbes of different species may fluctuate due to their species and changing environmental conditions. The quantitative composition of the microbiota can be influenced [2]:
- condition of the oral mucosa,
- physical conditions (temperature, pH, etc.),
- secretion of saliva and its composition,
- condition of hard dental tissues,
- food composition,
- hygienic condition of the oral cavity,
- absence of pathologies of the salivary glands, chewing and swallowing functions,
- natural resistance of the body.
Bacteria are retained on the surface of hard and soft tissues due to their morphological characteristics and certain intercellular interactions, which will be described below. Different types of bacteria have tropism for different tissues. For a further story about the formation of oral biofilms and the development of pathological processes, it is necessary to consider the main features of the predominant microorganisms.
This genus of bacteria is represented by immobile gram-positive cocci, located in “grape bunches” in the smear; are facultative anaerobes, chemoorganotrophs [5]. The most common representative of this genus in the oral cavity is Staphylococcus epidermidis, mainly located on the gums and in dental plaque. Breaks down food debris in the mouth and participates in the formation of dental plaque. Another common representative, Staphylococcus aureus, is the cause of the development of purulent bacterial infections, including generalized ones.
They are found in the oral cavity much more often than any other bacteria. Gram-positive spherical or ovoid cocci, chemoorganotrophs, facultative anaerobes [5]. Representatives of the genus that live in the oral cavity were identified as a separate group of oral streptococci. Like staphylococci, they break down food debris (mainly carbohydrates) to form hydrogen peroxide, as well as lactic acid, which plays a big role in the formation of dental plaque. Streptococcus mutans and S. sangius live mainly on the hard tissues of teeth and are found only after damage to the enamel, S. salivarius - mainly on the surface of the tongue.
Gram-negative anaerobic non-spore-forming cocci, chemoorganotrophs [5]. During their life activity, they decompose lactate, pyruvate and acetate into carbon dioxide and hydrogen, which increases the pH of the environment and has a positive effect on the formation of dental plaque (mainly Veillonella parvula) and the growth of other microorganisms. In addition, they are able to oxidize food debris to various organic acids, which promotes demineralization processes and the formation of microcavities.
Disturbance of oral microflora: causes
Oral dysbiosis can be caused by a variety of diseases and problems. Violation of opportunistic microflora of the oral cavity most often causes problems such as:
- Diseases of the gastrointestinal tract. Malfunctions of the digestive organs lead to a slowdown in metabolic processes in the body. The absorption of vitamins and nutrients deteriorates, the balance of the intestinal bacterial environment is disrupted, which provokes problems in other organs and systems.
- Decreased immunity. If the body's resistance deteriorates, the oral cavity automatically becomes more vulnerable to pathogenic microflora.
- Chronic diseases. Often, small caries or stomatitis, if left untreated, can spread from the source of inflammation to the entire oral cavity.
- Bad habits, such as systematic drinking of alcohol and smoking, inevitably affect the quality of the salivary glands. Prolonged drying out or too much moisture in the oral cavity has a detrimental effect on the composition of the microflora.
- Poor nutrition and lack of vitamins worsens the quality of saliva and makes the microflora of the oral cavity more vulnerable.
- Taking antibiotics and certain medications, such as hormones;
- Wearing dentures.
Why do bacteria and germs cause oral diseases?
Even stable microflora of the oral cavity cannot be called completely safe. Thus, any damage to the mucous membrane or tooth enamel and subsequent inflammation contribute to the development of pathogenic processes. Even normal microflora can become unfriendly with weakened immunity.
The most dangerous are “alien bacteria”. They reproduce as a result of disruption of the normal functioning of the ecosystem. This phenomenon is common in periodontitis, caries, stomatitis, gingivitis and other diseases. The uncontrolled spread of bacteria, fungi and microbes leads to the release of toxins and the development of the inflammatory process. Often such microorganisms demonstrate a tendency to constant relapses, especially if therapy is not accompanied by restoration of the microflora.
Stages of dysbiosis
Depending on the degree of development of the disease, dentists distinguish four stages of dysbiosis:
- Latent. The first, latent stage is characterized by subtle changes in the number of microorganisms of one strain. The patient feels well and does not experience any symptoms of inflammation.
- Subcompensated. The number of lactobacilli decreases, the disease has a blurred picture. The patient may feel discomfort in the oral cavity, but does not always understand that this is dysbacteriosis.
- Pathogenic. Lactobacilli are observed in minimal quantities in the oral cavity. The oral cavity begins to be populated by a facultative pathogenic environment.
- Decompensated. In addition to severe inflammation in the mouth, uncontrolled growth of yeast-like fungi occurs. The functioning of the salivary glands is disrupted, and an unpleasant taste and burning sensation occurs in the mouth.
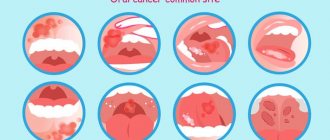
Advanced forms of dysbiosis are characterized by symptoms such as:
- inflammation of the gums and mucous membranes;
- plaque on the teeth and surface of the tongue;
- bleeding gums;
- ulcers and blisters on mucous membranes;
- increased body temperature;
- swelling and soreness of the tongue;
- dry skin, sticking in the corners of the mouth.
Methods for restoring oral microflora
Treatment of dysbacteriosis depends, first of all, on the nature of the pathogen, which is determined on the basis of dental examination.
Unfortunately, making a diagnosis of dysbacteriosis is often difficult, since at the initial stage the disease does not manifest itself in any way. At the slightest suspicion of a disease, the dentist refers the patient to a smear from the surface of the mucous membranes, blood and urine tests.
Depending on the diagnosed cause of dysbiosis, the dentist may prescribe the following methods of treating the disease:
- Sanitation of the oral cavity. The doctor removes tartar and fills all teeth affected by caries, and, if possible, treats the gums and mucous membranes.
- Treating the oral cavity with antiseptics to eliminate pathogenic microorganisms.
- Taking immunostimulants to strengthen the body and activate its defenses.
- A course of probiotics to restore the balance of beneficial bacteria in the oral cavity.
- Taking vitamin complexes for general strengthening of the body with vitamin deficiency. Properly prescribed vitamins promote cell regeneration and strengthen bone tissue.
In rare cases, antifungal agents and antibiotics are prescribed.
As a rule, the duration of treatment for dysbiosis is 2-4 weeks and depends on the patient’s health status, the number of foci of inflammation and existing complications of the disease.
A reliable assistant in the fight against dysbiosis will be the probiotic complex ASEPTA PARODONTAL*, a source of lactobacilli to restore the microflora of the oral cavity. This unique complex with patented strains of lactobacilli and vitamin D has the ability to effectively restore oral microflora. The complex normalizes the bacterial flora in the oral cavity, eliminates bad breath and prevents the formation of biofilms of pathogenic microorganisms.
To improve the effectiveness of the prescribed therapy, dentists recommend giving up bad habits (at least for the duration of treatment), reviewing the diet, paying attention to plant foods, and be sure to take care of the oral cavity after each meal.
Nine types of bacteria in the mouth
The human mouth is home to many microorganisms. It is not surprising that the oral microbiome ranks second in terms of the number and diversity of bacteria in the body, second only to the intestines, because inside there are different types of tissues and surfaces that come into contact with objects of the outside world.
Scientists count more than 700 known species of bacteria, as well as a variety of fungi, viruses and protozoa, inside the mouth. Many of the presented microorganisms are considered opportunistic flora, others – pathogenic. Let's look at nine types of microorganisms that have adverse effects inside the oral cavity.
Streptococcus mutans (streptococcus mutans)
The most well-known type of bacteria in the oral cavity, as it is considered the main cause of tooth decay. These bacteria begin to have a detrimental effect on teeth only if they manage to form colonies on the surface of the enamel, gradually destroying it.
Treponema denticola (Treponema denticola)
A type of gram-negative spirochete bacteria that plays a role in the development of periodontitis. They colonize periodontal pockets, causing inflammation. In the active stage of periodontitis, these bacteria are found in large quantities in periodontal tissues.
Trichomonas tenax (Trichomonas tenax, oral trichomonas)
The parasitic organism, often found in the mouths of people who do not practice good oral hygiene, is associated with periodontal infections. It is believed to feed on other microorganisms, but its secretions damage human tissue.
Entamoeba gingivalis (oral amoeba)
The first protozoan species discovered in the human microbiome. Some authors classify oral amoebae as opportunistic microflora. Others cite the results of studies proving the influence of oral amoebas on periodontal inflammation. They are localized in periodontal pockets, at the very base of the tooth. Found in 95% of patients with active periodontitis. Interestingly, these microorganisms are extremely rare in the oral cavity of patients with healthy gums.
Candida (candida)
Candida is a genus of yeast, the most common type of fungus in the human mouth and intestines. Considered an opportunistic pathogen, the most common type is Candida albicans. However, under certain conditions it can cause diseases such as aphthous stomatitis and even invasive candidiasis.
Actinomyces israelii (Wolff-Israel actinomycetes)
A species of rod-shaped bacteria from the actinomycetes family. Found in the oral cavity of healthy people. However, they can contribute to the development of caries, and are also considered the main cause of actinomycosis.
Campylobacter concisus (Campylobacter consisus)
A type of campylobacter that inhabits the oral cavity. Unlike most previously described microorganisms, Campylobacter is found in various organs and can cause severe disease. For example, this species can be found in the intestines, causing inflammatory diseases of the intestines and lower gastrointestinal tract.
Veillonella parvula (veillonella parvula)
Often found in the microbiome of healthy people, it has a negative effect on the development of caries and periodontitis. It poses a great danger to the cardiovascular system, since the activity of the bacteria Veillionella parvula has been found to be associated with hypertension and endocarditis.
Fusobacterium nucleatum (Plauta's bacillus)
An opportunistic microorganism, which, nevertheless, contributes to the formation of periodontal plaque. Studies have found a connection between Plaut's bacillus and premature birth, as well as colon cancer.
Possible complications of dysbiosis
It is important for each patient to closely monitor the state of the oral microflora. Lack of treatment for dysbiosis can lead to such unpleasant diseases as:
- pathological halitosis – bad breath caused by an imbalance of the oral microflora;
- caries – destruction of hard tooth tissues;
- pulpitis - inflammation of the pulp - the internal tissues of the tooth;
- periodontitis – inflammation of the tooth root membrane and adjacent tissues;
- gingivitis – inflammation of the oral mucosa;
- stomatitis – damage to the oral mucosa;
- periodontitis is a deep lesion of the periodontal tissue.
In addition, the close relationship between the state of the oral microflora and the state of the cardiovascular system has been scientifically proven. In 2008, it was proven in the USA that periodontal disease, as a source of chronic inflammation, is an independent risk factor for coronary heart disease (CHD).
So, now you know the role of normal oral microflora in the human body. Treat yourself carefully, and your healthy body will delight you every day.
What bacteria inhabit the oral cavity?
The permanent microflora of the mouth consists of 30 strains of microorganisms that are responsible for the most important functions. These strains include: streptococci, veillonella and diphtheroids.
Almost 300 species of microorganisms constantly reside in the oral cavity. Among them there are pathogenic - harmful. Suitable habitats for parasites are braces and plates, carious cavities, crowns, gum pockets, and the back of the tongue. Some teeth have a soft but thick layer of yellow plaque, which over time turns into dark tartar - this is the focus of harmful microorganisms.
Bacteria and microbes form a unique environment that is maintained in the normal state of the body and is capable of self-regulation. In the normal state of the oral microflora, beneficial bacteria outperform pathogenic bacteria.
Systematic hygienic teeth cleaning at the dentist is an essential attribute of a healthy and beautiful smile.
Every time we accept another patient for caries treatment, we are convinced that the price of professional hygiene is disproportionate to the consequences and costs that will have to be borne if it is not done.
It has been proven that even correct, scrupulous and constant home care is ineffective. 90% of adults brush their teeth ineffectively.
Teeth cleaning at Unit using modern technologies: Air Flow and ultrasound gives the maximum effect in maintaining a healthy balance of microflora and local immunity.
Sign up for professional cleaning