- home
- Useful articles
- Oral abscess: causes, symptoms, treatment
The development of an abscess in the oral cavity is associated with infection entering the pulp and its further spread throughout its entire structure. An inflammatory process begins, leading to tissue swelling and accumulation of purulent deposits. If the infection is not stopped and timely treatment is not started, then it will penetrate through the dental canals into other organs of the body, causing various diseases.
What is it and why does it happen
This disease is a local acute inflammatory process in the oral cavity, which is characterized by the accumulation of pus in the tissues of the gums, teeth or palate. Lack of timely and correct treatment can lead to a transition to a chronic form or cause such serious complications as the appearance of phlegmon or sepsis.
The causes of this disease are the presence of problems with the gums (gingivitis), with the roots of the teeth and adjacent tissues (periodontitis), with the enamel and hard surface (caries), as well as various mechanical injuries, infection, and chronic diseases. People suffering from diabetes and immune diseases are at increased risk of becoming acquainted with this unpleasant disease.
If your tooth is cracked, the roots are exposed, deep cavities appear, do not wait for an abscess to develop - be sure to visit the doctor at our dental clinic in Lyublino, because untreated caries is the main reason for the development of the inflammatory process.
In our clinic you can get a free dental consultation!
Causes of PTA
The disease rarely occurs independently and is often a complication of purulent tonsillitis or chronic tonsillitis. It develops when pathogenic flora penetrates the tissues of the palatine tonsils. The inflammatory process is provoked by:
- bacterial lesions against the background of Staphylococcus aureus, streptococci, Escherichia coli, Haemophilus influenzae, Klebsiella. A throat abscess occurs when a sore throat worsens. In some cases, the disease can develop without a previous infection of the pharynx with blockage of the salivary glands. Often paratonsillitis or paratonsillar abscess is preceded by acute tonsillopharyngitis;
- dental diseases. These include periostitis of the alveolar processes, gingivitis, caries, etc. They often cause peritonsillar abscess in children;
- injuries. The disease occurs through contact. Violation of the mucous membrane provokes infection of the area.
Our doctors
18 years of experience
Baghdasaryan
Armen Evgenievich
Chief physician, dentist-orthopedist-therapist
Graduated from VSMA named after. N.N. Burdenko. Internship on the basis of MGMSU named after. A.E. Evdokimov in “General Dentistry”.
Clinical residency at the Moscow State Medical University named after. A.E. Evdokimov in “Orthopedics”.
More about the doctor...
5 years experience
Sadina
Ekaterina Vladislavovna
Dental therapist, surgeon
Penza State University Medical Institute, specialty “Dentistry”.
In 2016, she underwent professional retraining in the specialty “Therapeutic Dentistry” at the Moscow State Medical and Dental University named after A.I. Evdokimov.
More about the doctor...
8 years of experience
Arzumanov
Andranik Arkadievich
Dentist-orthodontist
Graduated from Moscow State Medical University. Internship - Moscow State Medical University at the Department of Orthodontics and Children's Prosthetics.
Residency at Moscow State Medical University at the Department of Orthodontics and Children's Prosthetics. Member of the Professional Society of Orthodontists of Russia since 2010.
More about the doctor...
Symptoms
The main symptoms of this disease are:
- An increase in acute, throbbing or aching toothache, intensifying with food intake;
- Experiencing a bitter taste or unpleasant odor in the mouth;
- Feeling of general weakness, headache, apathy, insomnia, lack of appetite;
- Increased tooth sensitivity;
- The gums become inflamed, there is swelling, redness, a small compaction or swelling filled with pus is formed;
- There is an enlargement of the cervical lymph nodes;
- As the infection develops, nausea appears and body temperature rises;
- Facial asymmetry may appear, the size of one cheek, lower or upper lip may increase.
It is important to know that an abscess that begins on one tooth, if left untreated, can spread to the next. If the outer shell cannot withstand and ruptures, the pus comes out, it becomes easier and the pain goes away, but there is a risk of purulent masses getting into healthy tissues and teeth, and the sad story repeating. Ignoring purulent seals in the oral cavity can lead to such dire consequences: tooth loss, death of jaw tissue, development of respiratory diseases (pneumonia, sore throat) and vision. This is also fraught with paralysis of the facial nerves, and the entire body is exposed to acute intoxication.
Prevention of paratonsillitis
The following simple preventive measures will help prevent the development of peritonsillar abscess:
- strengthening the immune system;
- healthy lifestyle;
- timely treatment of acute and chronic diseases of the ENT organs (sinusitis, adenoids, pharyngitis, tonsillitis, etc.), caries;
- rejection of bad habits.
In the presence of recurrent abscesses, elective tonsillectomy is recommended.
Opening a peritonsillar abscess at the GMS clinic is a simple and safe surgical procedure that is performed in an outpatient or inpatient setting. Recovery takes 10-14 days, after which you will return to your normal life. You can make an appointment with an otolaryngologist at GMS Hospital by phone or using an online application.
What types are there
Depending on the location of the source of inflammation in the oral cavity, abscesses can be localized to:
- Gums One of the most common types, it forms around the inflamed soft tissues of a certain tooth, without proper treatment it becomes chronic. During an exacerbation, bad breath appears, accompanied by the discharge of pus and general weakness;
- Palate Usually occurs with periodontitis located in the teeth of the upper jaw, quickly spreads to other tissues, and can cause the development of osteomyelitis (bone necrosis);
- Cheeks A very dangerous type of inflammation, if left untreated there is a risk of inflammation spreading to the skin of the face. It affects the inside, and it is possible that the outside of the cheek can also be affected. A possible reason for the appearance is infection in the smallest wounds when biting the mucous membrane with teeth.
- Floor of the mouth Placed under the tongue, characterized by severe pain when eating or talking. An abscess that spontaneously opens can further spread the infection through the throat to other organs of the body;
- On the tongue, the surface thickens and swells. There is redness, it hurts to eat, talk and even just breathe. This type of inflammation causes a feeling of suffocation and lack of air, and therefore requires urgent hospitalization.
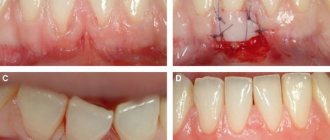
Treatment
To get a complete picture of the disease, dentists use modern diagnostic methods, on the basis of which they select the optimal solution to this problem. These include radiography, ultrasound, sampling of purulent mass and their analysis, visual examination of the condition of the pharynx (pharyngoscopy). Based on the results obtained and studying the history of the disease, appropriate therapy will be prescribed.
Before visiting a doctor, you can alleviate your condition a little by taking painkillers and warm antiseptic solutions, but you should not put off visiting the dentist for long, because the process develops very quickly and does not go away on its own.
Treatment of an oral abscess is usually carried out using two methods:
- Surgical intervention Allows you to avoid most of the complications that may arise from an unauthorized breakthrough of a purulent sac. The operation is performed under local anesthesia by a dental surgeon, with the help of special instruments the abscess is opened, the wound is cleaned and drainage is placed, after the operation antibiotics, antihistamines, vitamins and immunomodulators are prescribed;
- Medication Medications (Fluocinonide gel, Chlorhexidine solution, Ibuprofen) are prescribed only in the initial stage; timely consultation with a doctor and timely prescribed medications help avoid surgical intervention.
When the pus comes out, relief comes: there is no more pain, the temperature returns to normal, and the swelling disappears. The course of treatment ends with the necessary physical procedures: electropharesis with the addition of an antiseptic on the gums, UHF heating, and the procedure for silvering teeth affected by caries. Until the wound in the mouth completely heals, the patient must abandon hard vegetables and fruits in favor of soft cereals and liquid soups.
Treatment of peritonsillar abscess
In case of a complicated course, children (especially young children) are indicated for hospitalization and treatment in a hospital setting.
The main treatment method for PTA is systemic antibacterial therapy. In severe cases, severe intoxication, difficulty swallowing, nausea, antibacterial therapy is prescribed parenterally (bypassing the gastrointestinal tract) with subsequent transfer to oral forms of drugs - until the completion of the 14-day course of treatment. Courses of antibiotic therapy for less than 10 days increase the likelihood of disease relapse.
After prescribing systemic antibiotic therapy, dynamic observation for 24 hours is recommended. It is acceptable in patients with suspected paratonsillitis, without obvious signs of PTA, without signs of airway obstruction, sepsis, severe spasm of the masticatory muscles, or other signs of a complicated course of the disease. And also in children under 7 years of age with small abscesses and rare episodes of acute tonsillopharyngitis in history.
Studies have shown that systemic antibiotic therapy is effective even without draining the abscess. According to available data, 50% of children responded to systemic antibiotic therapy and did not require abscess drainage or tonsillectomy.
Systemic antibacterial therapy should include antibiotics active against GABHS, Staphylococcus aureus and respiratory anaerobes. For PTA, amoxicillin-clavulanate, ampicillin-sulbactam, and clindamycin are most often prescribed. If there is no or severe response, vancomycin or linezolid is added to treatment to ensure optimal coverage of potentially resistant Gram-positive cocci.
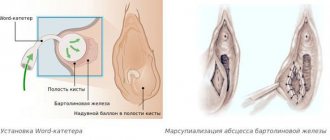
There are 3 methods of PTA drainage:
- PTA puncture - purulent discharge is removed through an aspiration needle;
- drainage of the PTA through the incision;
- tonsillectomy.
Draining an abscess never precludes the use of systemic antibiotic therapy.
All 3 methods of abscess drainage are comparable in effectiveness. The choice of procedure depends on the patient's condition, severity of the disease, presence of complications, age and the patient's ability to cooperate with the doctor.
For patients without spasm of the masticatory muscles or a history of recurrent acute tonsillopharyngitis, puncture drainage of the PTA or drainage of the abscess through an incision is recommended, which can be performed on an outpatient basis under local anesthesia.
Tonsillectomy is preferred in the following cases:
- presence of previous episodes of PTA or recurrent tonsillopharyngitis;
- significant upper airway obstruction or other complications;
- ineffective abscess drainage;
- presence of other indications for tonsillectomy (for example, obstruction of the upper respiratory tract and snoring due to the large size of the tonsils).
Randomized trials comparing puncture RTA drainage with incisional RTA drainage have shown comparable abscess resolution in more than 90% of cases.
Data on the benefits of systemic hormonal therapy (glucocorticoids) in the treatment of PTA are conflicting. Some studies show that the use of glucocorticoids (dexamethasone) can reduce the duration of symptoms of the disease, as well as reduce pain after drainage of the PTA. Other studies have reported no clear benefits of glucocorticoids in adults or children. Because the number of patients in these studies was small (ranging from 40 to 250 cases), further study of the effectiveness of routine use of glucocorticoids in the treatment of PTA is necessary.
Relapses of PTA occur in 10-15% of cases, more often in patients with a history of recurrent acute tonsillitis.
A risk factor for PTA is smoking.
Prevention
In general, the effectiveness of treatment depends on at what stage of the disease the patient sought medical help and his general health. It is very important to follow all doctor’s orders and treatment procedures immediately after they are prescribed. A timely surgical operation and the absence of complications after it are a guarantee of healing the abscess within one to two weeks.
Preventive measures to prevent this disease are very simple:
- Maintain hygiene, which includes high-quality and proper care of teeth and gums (brushing teeth and tongue at least twice a day, cleaning interdental spaces with dental floss after meals, regular use of mouth rinses);
- Treat carious teeth and other oral diseases in a timely manner;
- Protect the jaws and oral mucosa from injury;
- Have a complete diet, including vitamins and vital microelements.
Simple tips, the implementation of which depends only on your desire, will help in the future to avoid serious consequences caused by an abscess. And remember: oral health directly affects the beauty and charm of your smile.
Diagnostics of PTA
When contacting the medical otorhinolaryngology department, a detailed medical history will be collected. You will be asked questions regarding your health status. To clarify the clinical picture and choose the right treatment tactics, the ENT doctor will perform an examination, conduct a pharyngoscopy - an optical examination of the pharynx and tonsils, analyze your complaints, and refer you for laboratory tests.
culture for aerobic and anaerobic bacteria, if carried out
To clarify the diagnosis, imaging studies may be prescribed:
- Ultrasound;
- radiography;
- CT scan.