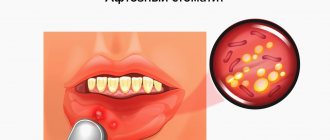
What does aphthous stomatitis look like?
Aphthae occur on the inside of the cheeks or lips, under the tongue, at the base of the gums, or on the soft palate.
https://img.medscapestatic.com/pi/meds/ckb/75/43075.jpg
They can be confused with manifestations of herpetic infection , but the latter usually appears at the red border of the lips, rarely in the oral cavity - usually on the gums or hard palate.
Aphthae first look like red bumps (papules), which then quickly turn into ulcers, surrounded by a red rim and covered with a gray-yellow coating (exudate). 1-2 days before the appearance of aphtha, there may be a local burning sensation of the mucous membrane.
Sometimes the child or family members notice what often triggers the appearance of aphthae. Journaling can help with this.
According to American data, about 20% of the population suffered from recurrent aphthous stomatitis at one time or another in their lives.
Most often children suffer and usually these are minor canker sores.
The peak incidence of aphthae is 1-19 years.
Symptoms and types of disease
Necrotizing ulcerative stomatitis has three types: acute, subacute, chronic. Depending on the severity, there are mild, moderate and severe forms.
Stomatitis occurs in three phases: initial, active and resolution stages. At the very beginning, the patient complains of slight malaise. Then the onset of gingivitis can be diagnosed: it is characterized by bleeding gums and the development of hyperemia. The mucous membrane of the mouth becomes covered with ulcers, covered with a yellowish and then gray-green coating on top. Tissues affected by necrosis adhere so tightly to the surface that they begin to bleed when trying to remove them.
In a mild form of the disease, the lesion is limited. Moderate severity is associated with loss of performance due to constant poor health - nausea, dizziness and high fever.
If there is no timely treatment, the disease spreads to the bone tissue and osteomyelitis occurs.
Types of aft.
Small aphthae is the most common type of aphthae (80-85%). Their size ranges from 1 to 10 mm. Ulcers can appear singly or several at a time (up to five).
Usually heal in 7-10 days.
Large aphthae (10-15%) - more than 10 mm in diameter, can even be up to 3 cm, deeper, take longer to heal (10-30 days).
They may leave scars behind. Very rare in children.
Herpetiform aphthae (5-10%) are small, from 1 to 3 mm, located in groups like herpetic vesicles. They heal quickly, within 10 days. They are not typical for children; they usually occur in the elderly.
The rest of the oral cavity looks normal - there is no inflammation of the gums, redness of the tonsils and pharynx, enlarged and painful cervical lymph nodes.
There is no fever or other general manifestations.
Aphthae in children is manifested primarily by refusal to eat and drink due to pain in the mouth.
The reasons for the recurrence of aphthae are not completely clear; the most popular theory is related to errors in the immune system.
Doctors most often do not find a specific cause of the failure; most likely it is a combination of several factors.
But doctors still have assumptions about some factors.
Diagnosis of stomatitis in children for treatment
As we said earlier, young men and young children under 3 years of age are most often affected by the disease. Diagnosing the disease is only possible in a clinical setting. When analyzing, they try to find symbiotic organisms. If their presence is detected, then a course of treatment is prescribed. It is especially important to timely diagnose the presence of infection in young children, since their bodies are still weak to resist infection.
If stomatitis turns into a sore throat, then it is necessary to take an analysis of a sample from the surface of the necrosis or a deeper layer, in case of a complicated form. It is worth noting that Vincent’s illness very often accompanies other dangerous diseases, including HIV, leukemia, syphilis, gingivitis, scorbuta and others. It is for this reason that the examination often includes procedures to screen out the above diseases. When stomatitis is detected in children, treatment is prescribed only after an accurate diagnosis.
What predisposes to recurrent oral aphthae?
Perhaps the microflora of the oral cavity, herpes group viruses, and maybe Helicobacter pylori, a microorganism that causes stomach and duodenal ulcers, play some role.
Also influence:
- injuries to the oral mucosa
- stress
- deficiency of vitamins B12, B1
- vitamin D deficiency
- zinc deficiency
- poor oral hygiene
- nitrates in drinking water
- Sodium lauryl sulfate is a very popular surfactant in the industry, which is often added to toothpastes for better cleaning and foaming effect.
- food allergies (eg, cow's milk protein) or food hypersensitivity (cinnamon, coffee, chocolate, cheese, figs, pineapple, citrus fruits, some spices)
- non-steroidal anti-inflammatory drugs
It is very important to understand: recurrent aphthae is an independent disease (most often this happens) or a manifestation of some systemic disease.
The latter option is rare, but the doctor should always keep in mind the possibility of this situation.
What is stomatitis?
Stomatitis, which means “mouth” in ancient Greek, is the most common name for a group of diseases of the oral mucosa. The disease should not be confused with glossitis (damage to the tongue), cheilitis (damage to the lips) and palatinitis (damage to the palate). Stomatitis is not contagious, but almost every person has directly or indirectly encountered one or another type of the disease. Once you have been ill, the chance of recurrence of the disease is very high.
Correctly diagnosing stomatitis is difficult. The doctor often assesses the situation only visually - in medicine there are no special tests for this disease. The difficulty of diagnosing stomatitis also lies in the fact that it can be a symptom of more serious diseases.
What systemic diseases can manifest as aphthae?
- Reiter's syndrome
- Behçet's disease
- AIDS
- cyclic neutropenia
- PFAPA syndrome
The gastroenterologist is especially interested in the connection between recurrent ulcers and specialized systemic diseases.
Celiac disease is found in 5% , and for a long time canker sores may be the only manifestation of a reaction to gluten.
Let me remind you that the estimated prevalence of celiac disease in the general population is about 1%.
Enamel defects and aphthous stomatitis in celiac and healthy subjects: Systematic review and meta-analysis of controlled studies
Other important conditions that manifest as canker sores are inflammatory bowel diseases: Crohn's disease and ulcerative colitis.
Extraintestinal Manifestations of Pediatric Inflammatory Bowel Disease: Prevalence, Presentation, and Anti-TNF Treatment
Possible complications
If stomatitis in the mouth is left untreated, it will certainly lead to negative consequences, from gum inflammation to tooth loss. That is why it is extremely important when treating stomatitis to strictly adhere to the recommendations given by your dentist. The list of major potential complications includes the following diseases.
- Chronic stomatitis.
Statistically, this is the most common complication. An untreated inflammatory process becomes chronic and recurrent, which means that an infectious focus will always be present in the body. - Appearance of scars.
A symptom such as bleeding gums can be a manifestation of many diseases, but with stomatitis, due to constant non-healing cracks in the oral cavity, scar tissue forms, which in the future may not allow the patient to open his mouth wide. - Laryngitis.
If the infection spreads up the respiratory tract, the patient's voice becomes hoarse and a cough appears. - Vision problems.
With advanced herpetic stomatitis, the target of damage becomes not only the gums, but also the mucous membranes of other organs. Most often, these are the eyes and genitals. - Loss of teeth.
The most dangerous complication of stomatitis. The main threat is the fact that the destructive process can last for many years and may not be noticeable to the patient at first. First, periodontal disease will develop - serious damage to periodontal tissue. And only then, as a consequence, the teeth will gradually become looser until they fall out.
What can help in finding the cause of aphthae?
A conversation sometimes helps to find out whether relatives have important diseases with a family predisposition - celiac disease, Crohn's disease, lupus erythematosus.
During the examination, the doctor can evaluate the general manifestations of the disease (not typical with ordinary recurrent aphthous stomatitis) and check for the presence of ulcers outside the oral cavity.
The simplest laboratory examination is carried out - this is most often enough.
A general blood test may show anemia due to deficiency of iron, folic acid, and vitamin B12.
The level of neutrophils is also assessed - their decrease may be a sign of the rare systemic disease cyclic neutropenia
A high ESR may be a sign of Crohn's disease and ulcerative colitis.
Serum iron levels may be reduced in up to 20% of recurrent canker sores.
Treatment methods for stomatitis
In order to successfully get rid of the disease, it is best to perform sanitation of the oral cavity. After eliminating the pain, doctors can begin to remove ulcers and unwanted deposits. In practice, a course of antibiotics is most often prescribed. So, an adult should drink about 4-5 tablets a day; for a child this norm is reduced to one. Also effective methods of treating the disease include:
- antiseptic substances
- it is recommended to rinse your mouth with them at least 4 times a day; - trichopolum
- for optimal treatment, it is enough to take half a gram per day; - antihistamine therapy
- this method helps to suppress microbial sensitization; - in the vitamin complex
- to maintain the tone of the body, as well as strengthen it, it is recommended to consume vitamin C at least one and a half grams per day; - keratoplastic ointment
- it is used to lyse infectious plaque.
Treatment of aphthous stomatitis.
There is no radical and quick treatment.
The main task of the doctor is to fight the pain caused by aphthae. This is especially important for young children, who may refuse to eat or drink due to pain and become easily dehydrated.
For this purpose, local painkillers and drugs are used that form protective films on the aphthae.
The second goal is to speed up healing.
The most popular drugs for healing are anti-inflammatory corticosteroids for aphthae, in rare, especially severe situations - even orally for a short course (prednisolone tablets).
The third task is to avoid or at least reduce the frequency of recurrent aphthae.
For some people, regular intake of vitamins (especially B12), zinc, and iron helps.
Avoiding oral hygiene products containing lauryl sulfate may be helpful.
Together with your dental hygienist, you can consider ways to improve your oral hygiene.
A gluten-free diet will help with celiac disease.
The most common diseases of teeth and gums
- Caries.
This is a common problem that affects almost every person at different ages. At the first stage of development, spots appear on the enamel, and as a result of development, hard tissues are destroyed;
- Gingivitis.
An inflammatory process that causes swelling and tenderness of the soft tissues. If treatment is not treated in a timely manner, the problem worsens and becomes chronic;
- Periodontitis.
A popular problem in which the initial stage is asymptomatic. Pain and discomfort appears after damage to bone and soft tissue;
- Periodontal disease
is expressed in periodontal damage, which can lead to tooth loss. Therefore, it is important to start treatment in a timely manner.
Conclusions:
Aphthae in the mouth recur at some point in life in almost 20% of all people, most often in the second decade of life.
It is difficult to establish a clear and unambiguous reason.
If recurrent aphthae occurs, the pediatrician, physician, or dentist should consider the possibility that rare aphthae are a manifestation of a serious systemic disease.
In such situations, the gastroenterologist must exclude celiac disease, Crohn's disease and ulcerative colitis.
5, total, today
Types of ulcerative stomatitis
Necrotizing ulcerative stomatitis can be acute or chronic. The acute phase usually lasts ten to fifteen days. Proper treatment during this period accelerates the healing process and prevents relapses. The pain goes away, the damaged areas are cleared of dead tissue, granulation and healing of the ulcers occurs. However, with self-medication at home or a complete lack of therapy in an already healed area, Vincent's stomatitis can resume and become chronic.
In this case, the disease progresses slowly, with mild symptoms, and virtually no pain. The main complaints are related to bleeding gums, increased salivation and putrid breath. Also, with chronic ulcerative-necrotic stomatitis, areas with congestive swelling, redness, ulceration and necrosis of the gums in the interdental spaces are visible on the mucous membrane. At an advanced stage, probing the gum edge reveals exposed gum bone. In addition, in adults, complications of necrotizing ulcerative stomatitis such as inflammation of the middle ear, chronic runny nose, inflammation of the genital tract, gastroenteritis, etc. are possible.
Ulcerative-necrotizing stomatitis
Necrotizing ulcerative stomatitis is an infectious disease. Its causative agents are Vincent's spirochete and spindle-shaped rod. It can affect only the gums, cover the entire mucous membrane of the mouth, and spread to the tonsils.
Degree of damage
The diagnosis is made depending on the degree of damage to the mucous membrane:
- Vincent's gingivitis or gingivostomatitis (only the gums are affected).
- Stomatitis (gums and other areas of the oral cavity are affected).
- Vincent's tonsillitis (the pathological process spreads to the oral mucosa and involves the palatine tonsils).
Causes
The main reason for the development of the disease is improper oral hygiene. The causative agents of the disease are present in the oral microflora of all healthy people. If hygiene rules are not followed, their number increases, resulting in the development of a pathological process.
The rapid development of ulcerative necrotic stomatitis can also be provoked by a general weakening of the body’s immunity and resistance. For this reason, the disease often accompanies colds.
Other reasons that can cause the development of stomatitis include:
- Hypothermia.
- Overwork.
- Severe stress.
- Exhaustion as a result of insufficient nutrition (for example, with strict diets).
The risk of developing stomatitis increases with the presence of injuries to the mucous membrane. The risk group includes patients whose mucous membranes are constantly injured, for example, by tooth fragments, poorly placed fillings, dentures, etc. Often stomatitis occurs during the eruption of wisdom teeth, since the gums are severely injured during the process.
Despite the abundance of reasons that can lead to the development of necrotizing ulcerative stomatitis, careless hygiene and poor dental care remain the most common provoking factors. The likelihood of developing the disease increases if:
- Plaques and tartar.
- Inflammatory processes in periodontal canals.
- Chips and cracks, etc.
Depending on the nature of the disease, acute, subacute and chronic stomatitis are distinguished. The disease can occur in varying degrees of severity.
Symptoms
At the initial stages of the disease, both specific (bleeding, burning, dry mouth) and general symptoms (weakness, fever, joint pain) occur. Often the patient considers them to be signs of other pathologies and does not associate them with the inflammatory process in the mouth. The duration of this stage differs depending on the severity of the disease. The disease can progress quickly and the condition worsens in just a few hours. In a chronic course, the first stage can last several days.
As the pathological process develops, the general condition worsens, and the following symptoms appear:
- Sharp pain in the mouth.
- Difficulty moving the tongue.
- Increased salivation.
- The appearance of putrid odor from the mouth.
Gradually, lesions develop on the gums. Subsequently, they spread to other areas of the mucosa. The gums swell and turn red. Severe pain and bleeding occurs. It becomes almost impossible to eat. As the disease progresses, the gums become covered with gray necrotic tissue.
General health depends on the severity of the disease. In a mild form, the patient’s general condition remains normal, the ability to work remains, and the person can lead a normal life. A severe course is always accompanied by a strong increase in temperature. The ulcers are deep and can reach tendons and bones. In this form, stomatitis can lead to another serious disease - osteomyelitis.
If you have a problem similar to that described in this article, be sure to contact our specialists. Don't diagnose yourself!
Why you should call us now:
- We will answer all your questions in 3 minutes
- Free consultation
- The average work experience of doctors is 12 years
- Convenient location of clinics
Single contact phone number: +7
Make an appointment
Treatment
If signs of stomatitis appear, you should immediately consult a doctor. During diagnosis, the doctor examines necrotic ulcers, determines the depth and extent of the lesion. After this, treatment is prescribed.
During treatment, it is important to ensure thorough sanitation of the oral cavity. The disease must be treated comprehensively:
- Rinse with antiseptic solutions.
- Taking antihistamines.
- Taking general strengthening medications and vitamin C.
- Ointments and applications for the treatment of necrotic ulcers.
- Removal of necrotic tissue and dental plaque.
Surgical intervention is indicated in cases where the development of stomatitis was provoked by the eruption of wisdom teeth. If treatment is started correctly and in a timely manner, the entire process takes 6 days. If the patient does not receive the necessary treatment in time, complications, gangrenous processes, and irreversible changes in the bones and periodontium begin to develop.
If you have a problem similar to that described in this article, be sure to contact our specialists. Don't diagnose yourself!
Why you should call us now:
- We will answer all your questions in 3 minutes
- Free consultation
- The average work experience of doctors is 12 years
- Convenient location of clinics
Single contact phone number: +7
Make an appointment
Sources:
- Personal experience as a periodontist;
- Diseases of the teeth and oral cavity; GEOTAR-Media - Moscow, 2012;
- Diseases of the oral mucosa; Phoenix - Moscow, 2007;
- Clinical manifestations of infectious diseases in the oral cavity in patients with HIV infection; Publishing house of the Russian Peoples' Friendship University - Moscow, 2013;
- Therapeutic dentistry. Diseases of the oral mucosa. In 3 parts. Part 3; GEOTAR-Media - Moscow, 2013;
- Therapeutic dentistry. Diseases of the lacrimal membranes of the oral cavity. In 3 parts. Part 3: GEOTAR-Media Moscow, 2013;
- Banchenko G.V., Rabinovich I.M. Syphilis and its manifestations and oral cavity. Clinic, diagnosis, treatment; Medical Information Agency - Moscow, 2008;
- Bark K., Burgorf V., Hede N. Diseases of the mucous membrane of the oral cavity and lips. Knika. Diagnosis and treatment. Atlas and guide; Medical literature Moscow, 2011;
- Brad W. Neville - Oral and Maxillofacial Pathology (2016).
Stomatitis and treatment at home
Treatment of stomatitis at home primarily involves the use of various herbal decoctions and infusions with antiseptic, anti-inflammatory and immunostimulating effects. For example, even doctors recommend rinsing with calendula - it has a strong antimicrobial and anti-inflammatory effect and promotes healing. Chamomile is an excellent antiseptic - it is one of the most popular remedies that is widely used in folk and official medicine.
Stomatitis is treated using folk remedies not only for rinsing, but also for oral administration. For example, rosehip decoction is a real storehouse of vitamins and other substances necessary for the human body. It improves immunity, prevents the development of inflammatory processes, and also helps destroy harmful bacteria. Despite the miraculous power of herbs, it should be remembered that candida and herpetic stomatitis will not be eliminated by such folk treatment, since fungi and viruses are not affected by antiseptic, anti-inflammatory and immune-modifying agents.