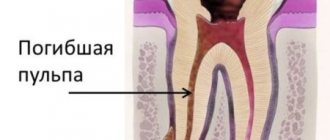
Gangrenous pulpitis is a putrefactive inflammation of the pulp in the crown and root parts of the tooth, which is accompanied by the death of its tissues. This form is considered one of the most dangerous and neglected, and its characteristic feature is the destruction of the pulp.
Gangrenous pulpitis of the tooth
is a late stage of chronic pulpitis, resulting from the lack of treatment for a disease such as caries. It is characterized by such unpleasant manifestations as darkening of the tooth, the development of halitosis (bad breath), and aching pain symptoms. Most often, this form of pulpitis affects the chewing teeth of the lower jaw.
Filling made of light-curing material for classes I and V - 2,000 rubles.
Filling made of light-curing material in classes II, III, IV - 3,000 rubles.
Placing a temporary filling - 400 rubles.
Resection of the root apex (frontal group) - 6,500 rubles.
Resection of the root apex (chewing group) - RUB 9,000.
Mechanical and medicinal treatment of canals for periodontitis (1 canal) - 1,100 rubles.
Closing perforations (MTA) - RUB 6,500.
At CELT you can get advice from a dental specialist.
- The cost of a dental consultation is 1,000
- The cost of an orthodontist consultation is 2,000
Make an appointment
Gangrenous pulpitis: etiology
Gangrenous pulpitis occurs due to the penetration of putrefactive anaerobic bacteria into the pulp. At the same time, the routes of penetration can be different:
- A carious cavity that requires treatment;
- Incorrectly carried out treatment, in which the affected tissues reached the nerve of the tooth (pulpitis develops under the filling);
- Violations of the technique of preparing a tooth for a crown;
- Deep periodontal pockets;
- Destruction of the tooth to soft tissues with severe abrasion;
- Periodontitis of the adjacent tooth;
- Various tooth injuries;
- Diseases of an infectious nature in which microorganisms are transferred to dental tissues through blood and lymph.
Another reason for the development is exacerbation of gangrenous pulpitis
, which was not cured and over time developed into a chronic form.
Causes
The key cause of the pathology is infection of the pulp chamber with putrefactive bacteria (anaerobic microflora). In most cases, it develops from the fibrous form of chronic pulpitis. Sometimes the disease occurs after acute diffuse pulpitis, which provokes necrosis of part of the pulp tissue.
Sources of infection:
- caries (pulp infection can occur when a tooth is opened for treatment);
- periodontitis of nearby teeth;
- sinusitis;
- osteomyelitis;
- mechanical trauma to the tooth, opening access to the pulp (for example, chipping off a piece of tooth or crown).
Symptoms
Symptoms of gangrenous pulpitis depend on the form in which it occurs:
- Acute gangrenous pulpitis is characterized by the presence of deep ulcers that cover the entire pulp. Due to the destruction of the septum between the carious cavity and the pulp, the infection penetrates inside. The acute form is characterized by severe pain that occurs for no reason or as a result of a reaction to irritants in the form of hot or cold food;
- Chronic gangrenous pulpitis is characterized by a dirty-gray tint of the upper layers of the pulp and the tooth itself, and the presence of a large carious cavity. There is no bleeding. There are practically no symptoms of pain, but sometimes aching pain may occur, especially when exposed to irritants. There is a putrid odor from the mouth.
The course of the disease depends on the following factors:
- pathogenicity of microorganisms;
- pulp resistance;
- the patient's general health status;
- periodontal condition;
- body resistance;
- the presence of concomitant pathologies.
This means that the process of development of the disease directly depends on how healthy the patient’s body is: the stronger it is, the more time it takes for bacteria to have a negative effect. Taking into account the above, we can conclude that the disease is especially severe in children, since the resistance of the child’s body is much lower than that of an adult. Clinic of gangrenous pulpitis
may vary depending on whether the tooth cavity is open or closed. So, with an open cavity, the following symptoms are observed:
| Symptoms of an open cavity | Symptoms with a closed cavity |
|
|
Pulpitis
4748 19 October
IMPORTANT!
The information in this section cannot be used for self-diagnosis and self-treatment.
In case of pain or other exacerbation of the disease, diagnostic tests should be prescribed only by the attending physician. To make a diagnosis and properly prescribe treatment, you should contact your doctor. Pulpitis: causes, symptoms, diagnosis and treatment methods.
Definition _
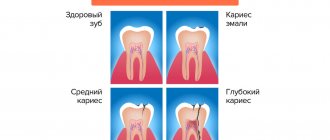
The term “pulpitis” refers to the inflammatory process in the pulp of the tooth. The pulp is a complex connective tissue structure rich in nerve fibers and blood vessels. According to statistics, among dental diseases, pulpitis ranks second after caries, of which it is a complication.
Causes of pulpitis
The most common reason for the formation of pulpitis is advanced caries. As dentin is destroyed, the carious cavity increases; the pathogenic microorganisms present in it (streptococci, staphylococci, diplococci, enterococci, gram-positive rods, etc.) penetrate through the dentinal tubules into the pulp chamber and trigger the pathological process.
Another cause of pulpitis is sinusitis, periodontal disease, periodontitis of the nearest tooth, osteomyelitis, sepsis, when the infection enters the pulp in a retrograde manner with blood and lymph flow through the apical opening of the root.
It is impossible not to mention such a reason as a medical error - we are talking about an insufficiently carefully sealed tooth canal during the treatment of deep caries, as a result of which an infectious process begins to develop under the filling.
In rare cases, the inflammatory process in the pulp becomes a consequence of tooth trauma, deep cracks and chips of the enamel.
Classification of the disease
There are several classifications of pulpitis. In Russia, the classification proposed by the Moscow Medical Dental Institute (1989) is more often used.
Acute pulpitis:
- focal,
- diffuse.
Chronic pulpitis:
- fibrous,
- hypertrophic,
- gangrenous.
Exacerbation of chronic pulpitis:
- fibrous pulpitis,
- gangrenous pulpitis.
In addition, pulpitis is distinguished by the condition of the pulp:
- intact non-inflamed pulp,
- atrophic pulp,
- reversible pulpitis,
- irreversible pulpitis,
- pulp necrosis.
Symptoms of pulpitis
Acute focal pulpitis is manifested by sharp paroxysmal pain: at first it is insignificant, but as the inflammatory process progresses it becomes unbearable.
Often the pain is especially bothersome at night.
In advanced cases (with diffuse pulpitis), the pain radiates to neighboring teeth, and sometimes the patient cannot even determine exactly where it hurts. In the case of focal pulpitis, the affected tooth may react to cold and hot food, and the pain subsides for quite a long time. With diffuse pulpitis, hot food increases the pain, and cold food brings relief for a while.
Chronic fibrous pulpitis reminds itself of itself with aching pain, and there is a reaction to hot and solid foods. Upon examination, the enamel of a diseased tooth may be darker and dull compared to others.
Hypertrophic pulpitis is characterized by the presence of pain, as well as bleeding of the gums when eating solid foods. Patients complain of bad breath (halitosis), which occurs as a result of poor oral hygiene due to bleeding gums.
Gangrenous pulpitis is characterized by a change in the color of the affected tooth to gray, the presence of a putrid odor from the mouth, a reaction to hot and cold food, and aching pain. The gums near the tooth may be swollen and hyperemic, and the regional lymph nodes are enlarged.
Chronic pulpitis in the acute stage is diagnosed in cases where exacerbations take a severe form: the patient experiences very severe pain after a long period of “calm”. Thus, this form of the disease often combines the symptoms of acute and chronic pulpitis.
Diagnosis of pulpitis
Diagnostic measures begin with collecting an anamnesis, during which the doctor determines the presence or absence of complaints of unmotivated pain, pain from exposure to various irritants.
In the absence of obvious pain, it is clarified whether the patient experiences discomfort in the area of the affected tooth (tingling, feeling of heaviness, fullness).
During a visual examination, the doctor performs palpation, percussion, determines tooth mobility, examines periodontal tissue, pays attention to swelling and hyperemia of the gums, and palpates regional lymph nodes.
For accurate diagnosis, the following studies are used:
- radiography - to assess the degree of destruction of tooth tissue and the size of the carious cavity;
- thermal test - to determine the reaction of a diseased tooth to thermal stimuli;
- electroodontodiagnostics - to determine the sensitivity of the nerve when an electric current is passed through it.
Which doctors should I contact
? Dental diseases are treated by dental therapists.
Treatment of pulpitis
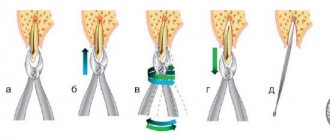
There are two ways to treat pulpitis: conservative and surgical.
Conservative treatment is indicated in the early stages of acute pulpitis. The doctor completely cleans out the carious cavity, puts an antibiotic in it and closes it with a temporary filling. After a few days, when the medicine takes effect and the infectious process is stopped, the temporary filling is replaced with a permanent one. Conservative treatment allows you to keep the tooth alive (do not remove the nerve).
Surgical treatment (depulpation of tooth canals) is carried out in 85% of cases. The doctor cleans out the carious cavity, removes the dental nerve, fills the root canals with filling material and restores the tooth crown.
If the tooth cannot be restored, it is removed.
In case of pulpitis, all manipulations with the affected tooth are carried out under anesthesia.
Complications
In the absence of timely treatment, pulp inflammation and tooth destruction progress, as a result, surrounding tissues are involved in the process, and complications such as periodontitis, gumboil, osteomyelitis, phlegmon, abscess, and cysts develop.
In rare cases, complications can be systemic in nature - sepsis, myocarditis, brain abscess.
Prevention of pulpitis
The most reliable prevention of pulpitis is oral hygiene and timely treatment of caries.
Sources:
- Clinical recommendations (treatment protocols) for the diagnosis of “dental pulp disease”. Dental Association of Russia. – 2018.
- .
- Khafizov R.G., Khafizova F.A., Azizova D.A., Shaikhutdinova D.I. Modern etiological, diagnostic and therapeutic aspects of pulpitis // Uch.-method. allowance. KFU Institute of Fundamental Medicine and Biology. - Kazan. – 2015. – 74 p.
IMPORTANT!
The information in this section cannot be used for self-diagnosis and self-treatment. In case of pain or other exacerbation of the disease, diagnostic tests should be prescribed only by the attending physician. To make a diagnosis and properly prescribe treatment, you should contact your doctor.
Gangrenous pulpitis in children
Children are much less susceptible to this disease... However, if it occurs, its treatment requires considerable effort. Most often, young patients suffer from chronic pulpitis due to the fact that they cannot correctly explain the essence of the problem and the nature of the pain. This leads to the disease becoming chronic. According to dentists, gangrenous pulpitis in childhood develops as a result of fibrous and purulent forms of pulpitis, occurring in a chronic or acute form, respectively. Necrosis of the tooth nerve begins as a result of the penetration of anaerobic microflora into it, while pain symptoms are determined by the peculiarities of the baby’s nervous system. During the examination, the dentist identifies large carious cavities and dead pulp tissue. Painful symptoms occur when probing the canal openings. For treatment, it is most often necessary to use a devital method of removing the nerve of the tooth.
What might you encounter after treatment?
Some patients report discomfort after filling. It is important to distinguish whether this pain is correct (post-filling) or one that requires immediate consultation with a doctor.
Mild pain is almost normal after pulpitis treatment. This is due to the fact that a serious intervention was performed, especially if inflammatory and pathological processes had previously occurred. Temporary pain occurs during the first couple of days and occurs when chewing. There is no need to go to the dentist, wait a while, the pain will go away.
The pain is sharp, intensifying and occurring throughout the week may indicate the continuation of the inflammatory process. Swelling of the gums indicates the same thing. In this case, you need to visit your dentist.
Diagnosis of the disease
Treatment of gangrenous pulpitis is prescribed only after the dentist makes the correct diagnosis. It is very important to be able to distinguish this disease from:
- deep caries;
- chronic fibrous pulpitis;
- apical periodontitis.
A visual examination of the oral cavity by a dentist reveals the following:
- deep carious cavity with softened dentin;
- open dental cavity;
- grayish coating on the upper layers of the pulp;
- change in the color of the tooth crown.
Probing the pulp can be painful, in contrast to percussion, in which there are practically no pain symptoms.
In addition to a visual examination, the doctor will prescribe:
- X-ray diagnostics;
- electroodontodiagnostics.
Diagnostics
The dentist detects visual symptoms during a routine examination and makes a preliminary diagnosis. During palpation and percussion, the patient usually does not feel anything, but deep probing of the pulp is accompanied by painful sensations.
To clarify the diagnosis, three main methods are used:
- Thermal diagnostics. The disease causes a painful reaction with a slow fading of pain to irritation with high temperature.
- Electroodontodiagnosis - shows reduced electrical excitability of the pulp (60-90 µA).
- Radiography. The image demonstrates pathological changes in the periapical tissues - an expanded periodontal fissure, foci of destruction localized near the root apex.
Reviews about our doctors
I would like to express my gratitude to the dentist Elena Nikolaevna Kiseleva and her assistant Svetlana - they are real specialists and at the same time sensitive, not burnt out by years of practice.
Thanks to them, I have been coming back here for many years. Thanks to the management for such doctors! Read full review Svetlana Nikolaevna
13.08.2021
I am very grateful to Evgeniy Borisovich Antiukhin for removing my three eights. Especially considering that the lower tooth was not the simplest (it was located in an embrace with a nerve). The removal took place in 2 stages, one tooth under local anesthesia, two under general anesthesia. I had no idea that wisdom teeth could be... Read full review
Sofia
28.12.2020
How is pulp necrosis treated?
The standard recovery course begins with root canal treatment. Further treatment is divided into several stages:
- Clean the root canals.
- Removal of dead pulp residues and rinsing with an antiseptic with sodium hypochlorite.
- Pathogenic bacteria are poisoned with a composition containing calcium hydroxide. In the oral cavity, in the affected areas, a highly alkaline environment is created, which destroys microorganisms.
- After two weeks, at a follow-up visit, all canals are washed with an antiseptic again and then sealed.
To prevent relapse of the disease, dentists recommend regularly seeing a doctor to monitor the condition of the treated teeth and pulp areas. Timely sanitation of foci of infection and replacement of old fillings with a broken marginal seal will preserve the health of the oral cavity for many years.
Treatment of gangrenous pulpitis
Unfortunately, treatment of acute and chronic gangrenous pulpitis
It is carried out only by surgical techniques. They involve removing the nerve of the tooth, since the process of its damage is irreversible. The procedure is performed under local anesthesia and requires complete removal of the pulp from the root and crown parts of the tooth. In order for it to proceed correctly, it is necessary to exclude bleeding. To do this, the dentist performs cauterization of the vessels. Once the pulp has been removed, one of two solutions is used:
- the canals are cleaned and sealed, and a permanent filling is applied;
- obturation is performed using calcium hydroxide and temporary filling.
Since the disease is often accompanied by severe destruction of the crown part of the tooth, it may require the installation of an artificial crown to restore it.
Diagnosis of chronic pulpitis
The disease most often occurs as a complication of caries, when bacteria enter the pulp and cause an inflammatory process in it. However, the penetration of microorganisms is possible with dental injuries, gum disease (through periodontal pockets), as well as with sinusitis and osteomyelitis (much less often). Diagnosis of chronic pulpitis is carried out using a number of techniques that make it possible to accurately determine the form and stage of the disease.
- Visual inspection.
With the help of a dental probe and a mirror, you can almost always notice damage to the teeth and the development of the disease (the exception is chronic pulpitis under a filling). - Radiography.
The most common way to diagnose most dental diseases. - EDI (electroodontodiagnosis).
Use of electrical current to assess the viability of pulpal nerve endings. - Thermometry.
Exposure of the pulp to temperatures to assess its condition.
Treatment prognosis and disease prevention
Dentists at the CELT clinic give favorable prognoses for treatment that was carried out efficiently and on time. In any case, they take all measures to save the tooth.
In order to avoid this disease and keep the tooth healthy, it is necessary to undergo preventive examinations at the dentist every six months and not try to endure toothache. The earlier the disease is detected, the easier and faster it can be cured. Prevention measures also include maintaining oral hygiene. The dental department of the CELT clinic offers services for the treatment of the most complex cases of gangrenous pulpitis. Contact us and be healthy!
Make an appointment through the application or by calling +7 +7 We work every day:
- Monday—Friday: 8.00—20.00
- Saturday: 8.00–18.00
- Sunday is a day off
The nearest metro and MCC stations to the clinic:
- Highway of Enthusiasts or Perovo
- Partisan
- Enthusiast Highway
Driving directions
Common causes of pulp death
Let us highlight the main factors for the occurrence of pulp necrosis:
- Chemical - in the treatment of caries with alcohol, phenol. Diagnosed by the gray color of the hard tissues of the tooth and on x-rays;
- Bacterial - with mixed microflora with streptococci, staphylococci, clostridia, fusobacteria.
- Thermal – after a burn when processing a tooth with tips without water cooling.
- Mechanical - the result of a new or non-healing old wound, as well as pathological abrasion of teeth (biting fabric, fishing line, biting seeds, etc.)
Stages of treatment
Most of the operations, the main task of which is to heal the inflamed pulp, can be divided into a list of conditional stages:
- Excision of dental tissue.
- Extraction of the neurovascular bundle itself.
- Channel cleaning.
- Filling.
The question of how pulpitis is treated in 2 visits with the removal of teeth and nerves can clearly be answered by any more or less qualified dental specialist. However, not everyone, even experienced doctors, had to deal with the most severe forms of this disease. It is not difficult to guess that the key to the success of the entire therapy as a whole is a visit to a specialized specialist who knows how to handle modern equipment and the advanced range of today’s pharmacological drugs. Such professionals, of course, include dental staff.
Pulp anatomy
In the depths of the tooth, under the dentin layer, there is a pulp, which consists of soft, loose, fibrous connective tissue, dotted with blood and lymphatic vessels, as well as nerve endings running from the jaw along the root canal through the apical foramen.
Pulp (lat. pulpis dentis) is the “heart” of the tooth, reliably protected by powerful dental walls of bone tissue from the effects of external factors, nourishing the tooth with minerals, ensuring its growth, restoration, and vitality. It is important to note that the pulp is not only a space of soft tissue (pulp chamber), but also the dental canal connected to it. The pulp chamber is a loose, amorphous colloidal system containing loose, fibrous connective tissue, as well as a large number of elastin and collagen fibers. The cellular composition of this system contains histocyotes, mast cells, macrophages, as well as fibroblasts that produce collagen and provide intercellular communication. The surface layers of the fibrous structure of the pulp contain odontoblasts - cells with long processes located in the dentinal canals. These processes make dentin sensitive to any irritants. Stellate cells are located a little deeper, and the central layer contains collagen and nerve fibers and blood vessels. If an inflammatory process begins in the pulp, then leukocytes appear in the structure, lymphocytes and plasma cells are activated.
In addition to providing the tooth with nutrition, the pulp performs several other important functions. Plastic, responsible for the delivery of “building” proteins, is ensured by the activity of odontoblasts involved in the formation of dentin: before the eruption of the primary tooth, after eruption - the secondary one. The protective function of the pulp is carried out thanks to macrophages, lymphocytes and fibroblasts. Macrophages “recycle” dead cells and, together with lymphocytes, are responsible for immune reactions, and fibroblasts produce and maintain the necessary balance of the intercellular substance of the pulp, which is responsible for metabolic processes in it. In general, the protective function of the pulp is to create a barrier for the penetration of pathogenic bacteria that have entered through the dentin further, along the root canal into the periodontium, and then to the soft tissues surrounding the tooth. In addition, the protective function includes the regeneration of the so-called replacement (tertiary) dentin: when caries occurs, this dentin prevents its spread deep into the tooth. The trophic function of the pulp, which affects the metabolism and nutrition of the tooth, supporting the vital activity of tooth enamel, is ensured by the activity of a developed vascular system, characterized by thin vessel walls, high blood flow speed and, accordingly, higher pressure than in other organs. The sensory function of the pulp is carried out due to the activity of a large number of nerve fibers, which, like a fan, diverge from the apical foramen to the periphery of the pulp.
Very often the pulp is called the “dental nerve” because its sensitivity to any irritants is so high that inflammation, as a response to a bacterial, viral, or infectious attack, occurs almost immediately. Such inflammation in medical terminology is called pulpitis.
Diagnosis of traumatic pulpitis
This type of disease, like other types of pulpitis, requires immediate treatment before complications begin. The dentist will conduct a diagnosis, including:
- examination in the dental chair;
- x-ray or computed tomography;
- electroodontodiagnostics.
Electroodontometry analyzes the condition of the pulp using alternating current - diseased and healthy teeth react to it differently. This study is performed instead of an x-ray or as an addition to it. Accurate diagnosis of traumatic pulpitis helps the dentist create an optimal treatment plan.
It will not be superfluous to know what symptoms manifest the clinic of traumatic pulpitis. A damaged tooth reacts sharply to hot/cold food, even cold air causes discomfort, and any touch to it is very painful. If the pulp was injured during dental treatment, the patient feels a sharp pain. Trauma to a wisdom tooth is accompanied by a sharp putrid odor that hygiene products cannot cope with.
Symptoms of pulpitis
The first symptom indicating pulp inflammation is an attack of pain. Suddenly there is an acute toothache. Most often, sweet or cold food (drink) becomes a direct irritant. The symptom lasts no more than 1-3 days. This indicates the acute phase of pulpitis. If there is no treatment at this stage, the inflammation will deepen and irreversible changes in the pulp will occur. Then the toothache will become constant, mainly, it will appear in the evening when changing position from vertical to horizontal. Warm food or chewing food will become an irritating factor. Continued lack of therapy will result in irreversible loss of pulp viability. The carious defect will become very deep and extensive. This stage of change may initially be asymptomatic. As a result, the only treatment method will be endodontic treatment, that is, root canal treatment. Sometimes pulpitis can also present with general symptoms such as weakness, fever or headaches.
How much does it cost to treat traumatic pulpitis in Moscow clinics?
The cost of therapy depends on the degree of damage - the larger the chip, the more expensive. In Moscow clinics, prices for pulpitis treatment start from 6,000 rubles for a single-canal tooth and reach 12,000 rubles. The price tag is also affected by which tooth the problem arose with. On the chewing one, you can limit yourself to only treatment, and the anterior one, as a rule, also has to be restored. This increases costs by at least 3,500 rubles. Treatment methods for traumatic pulpitis also differ in cost: conservative methods require more time and effort from the dentist, which means they are more expensive. The surgical option to remove the pulp will be cheaper.
Age restrictions
Pulpitis can occur in anyone at any age. The conservative method of treating this disease has no age restrictions. When choosing a surgical method in patients over 45 years of age, it is necessary to take into account the condition of periodontal tissues.
Treatment of pulpitis in children with baby teeth has its own characteristics. Thus, the inflammatory process in baby teeth arises and spreads rapidly and does not always depend on the depth of carious lesions and visible tissues affected by caries. In this case, it is extremely important to stop the spread of infection to the periodontal tissue, since the rudiments of molar teeth are formed in this tissue. However, removal of teeth affected by pulpitis is used only in rare cases, since the absence of each dental unit has a negative impact on the formation of the bite. In the treatment of pulpitis of baby teeth, filling pastes are used that do not affect the rudiments of the molars, but are absorbed along with the “milk” roots when teeth change begins. Anesthesia must be carried out taking into account possible allergic reactions.
Complications of pulpitis
Unfortunately, patients very often ignore toothache that occurs during acute pulpitis (when necrosis has not yet occurred or necrotic lesions are small). This is a big mistake. Consulting a dentist at this stage and carrying out the correct treatment can not only save the tooth, but also prevent dangerous complications.
The consequences of pulpitis can be:
- Flux,
- Periodontitis,
- Destruction of tissue around the tooth root,
- Abscess formation,
- Pulp gangrene (necrosis),
- Degradation of the bones adjacent to the tooth root
- Periodontal tissue infections,
- Formation of fistulas and cysts,
- Tooth loss,
- The development of systemic diseases caused by bacteria entering the bloodstream: myocarditis, sepsis, brain abscess, glomerulonephritis and rheumatic diseases.
Why may pain persist after treatment?
- Pain may occur if the tooth has retained its sensitivity, and during the treatment the pulp tissues were accidentally damaged or burned.
- Pain can also be caused by irritation of the mucous tissue around the apex of the tooth root, caused by strong antiseptics used to wash the canals.
- It can also appear due to minor trauma to the tissue of the apex of the tooth root, which the dentist may inadvertently inflict with an instrument during the treatment process.
According to statistics, those who have undergone treatment for gangrenous pulpitis experience re-inflammation of the tissue and pulp surrounding the tooth.
How to recognize the beginning of a repeated inflammatory process in time? You need to pay attention to the following signs:
- two or three days after treatment there is no improvement in the condition, and the pain remains intense;
- painkillers do not help and relieve pain only for a short time;
- there is a slight increase in temperature;
- There is swelling and redness on the gum, pain when pressed.
What might these signs indicate? First of all, due to poor quality dental treatment. Perhaps, during the treatment process, the pulp doctor did not notice and did not remove the area of the pulp damaged by bacteria, and perhaps did not completely seal the dental canal. Also among the possible causes of pain are a burn of periodontal tissue or an inflammatory process under a filling.
Therefore, it is very important, in order to prevent the recurrence of the disease, after filling the canals, take a picture to make sure that everything is done correctly and all the canals are filled without voids.
If the pain persists after three days, does not lose its intensity and causes inconvenience, you should consult a dentist. Most likely, you will need to re-treat gangrenous pulpitis, and this time not with conservative methods, but with complete removal of the pulp.