Dental periodontitis is an inflammation of an infectious nature that occurs at the membrane of the tooth root and affects the tissues of the oral cavity located next to it. Periodontitis is difficult to confuse with other dental diseases, because it has a clear symptom – severe and constantly increasing pain, which cannot be relieved by taking tablets from the pharmacy.
Treatment of periodontitis must be carried out urgently, because you risk not only losing a tooth, but also acquiring complications that are dangerous to the overall health of the body! How periodontitis occurs, what signs will help to identify the disease in a timely manner, how periodontitis is treated in dentistry, at what prices the service is offered in Moscow - we will talk about this in detail in this article.
Indications for treatment of periodontitis
There are two main ways to treat periodontitis: conservative and surgical. Each of them has its own indications and contraindications.
According to modern dental standards, a doctor should give preference to conservative methods. They are indicated for both acute and chronic periodontitis, including the appearance of cysts and granulomas, loose teeth, and increasing inflammation.
However, orthograde treatment cannot be used in all cases. Indications for surgical intervention are:
- obstruction of the tooth root canals;
- the presence of a stump tab or pin that cannot be removed without damaging the roots;
- multiple perihilar cysts or cysts growing into the maxillary sinus;
- wide affected area (over 10 millimeters);
- perforation of the tooth cavity or root wall;
- ineffectiveness of conservative treatment methods.
Important!
When we talk about periodontitis, we often mean apical (also known as periapical or apical) periodontitis - that is, inflammation at the apex of the tooth root. The cause of this disease is endodontic problems. Another type of periodontitis, marginal, affects the gums in the cervical area of the tooth, but it already belongs to the field of periodontology. This material is devoted to the treatment of apical periodontitis only.
Causes of periodontitis
The etiology of periodontitis in most cases is associated with advanced forms of caries. When the pulp is damaged, the inflammation spreads to the root of the tooth and then spreads through the canal to the periodontium. In addition, the causes of the disease can be:
- tooth trauma - fracture or crack of the root, bruise, chipped crown with subsequent penetration of infection into the pulp;
- violation of the root canal treatment technique with tissue injury with sharp instruments;
- violation of the root canal filling technique with filling material extending beyond the root apex;
It is important for the dentist to find out the cause of periodontal inflammation in order to select the optimal treatment regimen for the tooth and prevent relapse.
Treatment methods for dental periodontitis
| Conservative treatment | Surgery |
Therapeutic:
Physiotherapeutic:
Conservative treatment of periodontitis is accompanied by the use of antibiotics. | Surgical treatment:
|
Important!
The probability of successful conservative treatment of periodontitis is 70 - 90%
Why is chronic periodontitis dangerous?
The anatomical structure of the teeth ensures in most cases the free outflow of serous and purulent masses from the source of inflammation. As a result, the patient may not be aware of the presence of chronic periodontal inflammation for a long time. All this time it is actively developing, exposing tissues to destruction. Sometimes this leads to the fact that it is no longer possible to save the tooth.
In addition to tooth loss, chronic periodontitis leads to the formation of skin or gingival fistulas and various types of granulomas, which require long-term (several months) complex and expensive treatment.
Granulomatous formations pose an additional danger. They can, under the influence of such unfavorable factors as stress or hypothermia, lead to the development of serious inflammatory processes, including sepsis.
Chronic periodontal inflammation can also accelerate the progression of diseases such as nephritis, arthritis and rheumatism, and provoke other health problems.
Stages of periodontitis treatment
The number of visits to the clinic for the treatment of periodontitis depends on the stage of the disease (acute periodontitis, chronic, chronic in the acute stage) and the chosen technique. Often, therapy is carried out in several stages and requires at least 2 - 3 visits to the attending physician, since it is not recommended to install a permanent filling until the inflammation is completely removed.
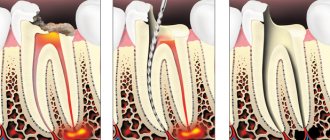
- Preparation for treatment: diagnosis using an x-ray, anesthesia injection.
- Drilling a tooth to access canals, removing a nerve, or removing an old filling.
- If necessary, expand channels.
- Antiseptic treatment of canals, application of medications, physiotherapeutic procedures.
- Installation of a temporary filling.
- Removal of the temporary filling, antiseptic treatment of the canals (this stage is repeated until the source of inflammation is completely eliminated; sometimes this may take several months).
- Installation of a permanent filling, control x-ray.
In parallel, the patient is prescribed antibacterial and anti-inflammatory therapy, as well as home rinses with disinfectant solutions.
Recommendations after treatment
After conservative or surgical treatment, you should not eat food for 2-3 hours due to the effects of anesthesia. Pain may be experienced for 7 days after surgery. It is recommended to rinse your mouth with antiseptics and a decoction of medicinal herbs. For severe pain, it is recommended to take painkillers. If pain persists and severe swelling is observed, contact your doctor immediately.
At the same time, the crown of the tooth changes its color, the presence of a carious cavity and tooth mobility are noted. Dentists at the CELT clinic successfully treat even the most advanced and severe forms of chronic periodontitis!
Make an appointment through the application or by calling +7 +7 We work every day:
- Monday—Friday: 8.00—20.00
- Saturday: 8.00–18.00
- Sunday is a day off
The nearest metro and MCC stations to the clinic:
- Highway of Enthusiasts or Perovo
- Partisan
- Enthusiast Highway
Driving directions
Features of the treatment of periodontitis with fistula
Odontogenic fistula is one of the complications of periodontitis, mainly granulating. It consists of holes in the mucous membrane, which are formed due to the proliferation of granulations and destruction of the tissues surrounding the tooth. In severe cases, a fistula can appear not only in the gum, but also in the cheek, and even on the skin of the face. Purulent contents are released through the hole, which appears due to the inflammatory process in the periodontium.
On the one hand, the formation of a fistula facilitates the course of the disease, since inflammatory products are eliminated through it (which means that the patient most likely will not suffer from severe pain). On the other hand, non-intervention over time can lead to tooth loss.
You can get rid of a fistula only by eliminating its cause - damage to periodontal tissue. Treatment follows a standard scheme: mechanical treatment of the canals, disinfection and thorough filling. Due to the outflow of pus through the fistulous tract, treatment is most often successful and takes less time. After creating suitable conditions, the fistula goes away on its own, but in severe cases, surgical removal of overgrown granulations may be necessary.
How does the acute phase of chronic periodontitis manifest?
When exacerbated, chronic periodontitis of the tooth expresses itself with the same symptoms as the acute form of the disease. That is, there is a strong, aching pain, swelling of the gums and swelling of the cheek. Typically, chronic periodontitis enters the acute phase when the immune system is weakened, the flu, ARVI, or simply severe hypothermia are present. If, during an exacerbation of the chronic form, a fistula appears in the gum area, pus will flow from the area of inflammation and the pain in the tooth will gradually subside.
But this does not mean that periodontitis has gone away on its own; the inflammatory process will continue to develop and will manifest itself again under favorable external factors, which we discussed just above. Based on the type of periodontitis, a treatment regimen is selected. The price of the service depends on the regimen chosen for treating the disease. We will tell you below about all the stages of treatment of dental periodontitis in different forms and prices for procedures. But no matter in what form periodontitis develops, its treatment always begins with diagnosis.
Diagnosis of periodontitis involves examination of the oral cavity, x-rays, and examination of patient complaints. All this together helps to accurately diagnose the form of periodontitis and prescribe adequate and effective treatment.
Treatment of chronic forms of periodontitis
There are three types of chronic periodontitis: fibrous, granulating and granulomatous.
- In fibrous periodontitis, the tissues surrounding the apex of the tooth are replaced by fibrous tissue. The patient usually does not feel pain, and the disease can only be determined by an x-ray.
- Granulating periodontitis is characterized by the growth of granulation tissue: the process of bone resorption (resorption) starts, fistulous tracts are formed, through which inflammatory products are separated. As the granulations expand, the patient begins to experience periodic aching pain.
- Granulomatous periodontitis is accompanied by the appearance of a granuloma - a neoplasm at the root apex. It is a chamber of connective tissue filled with granulations. If the disease is not treated, the growth of granuloma can even lead to a jaw fracture.
Treatment of chronic periodontitis is often carried out using conservative treatment methods. According to modern standards, doctors, as a rule, do not carry out separate treatment for granulomas, cysts and fistula tracts: if the canals are disinfected and properly sealed, the neoplasms will disappear on their own. In advanced cases, surgical intervention is permissible.
Periodontitis - symptoms and treatment
Acute apical periodontitis
After periodontal damage for one of the above reasons, a short-term intense tissue response occurs.
This process is accompanied by clinical symptoms of acute periodontitis.[7] The tissue response is usually limited to the periodontal ligament. It leads to typical neurovascular inflammatory reactions, which are manifested by hyperemia (overflow of blood), vascular congestion, swelling of the periodontal ligament and extravasation (leakage into the tissue) of neutrophils. Since the integrity of the bone, cementum and dentin has not yet been compromised, periapical changes at this stage are not detected by X-ray examination.
If the inflammation was caused by non-infectious irritants, the lesion may disappear, and the structure of the apical periodontium is restored.[13][14]
When infection occurs, neutrophils not only fight microorganisms, but also release leukotrienes and prostaglandins. The former attract more neutrophils and macrophages to the affected area, and the latter activate osteoclasts - cells involved in the destruction of bone tissue. Thus, after a few days, the bone surrounding the periodontium can be resorbed (dissolved), then in the area of the root apex, an expansion of the periodontal fissure is detected radiographically.[15]
Neutrophils die at the site of inflammation and release enzymes from their granules that cause the destruction of extracellular matrices and cells. This “splitting” of tissue prevents infection from spreading to other parts of the body and provides space for protective cells to penetrate.
During the acute phase, macrophages also appear in the periodontium. They produce proinflammatory and chemotactic (allergic) cytokines. These molecules enhance the local vascular response, bone destruction and extracellular matrix degradation, and may also cause hepatocytes to increase the production of acute phase proteins.
Acute primary periodontitis has several possible outcomes:
- spontaneous healing;
- further strengthening and spreading into the bone (alveolar abscess);
- exit to the outside (formation of fistulas or sinus tract);
- chronization of the process.[19]
Chronic periodontitis
The prolonged presence of microbial stimuli results in a shift towards macrophages, lymphocytes (T cells) and plasma cells, which are encapsulated in collagenous connective tissue.
Pro-inflammatory cytokines (immune system cells) are powerful stimulators of lymphocytes. Activated T cells produce a variety of cytokines that reduce the production of proinflammatory cytokines, leading to suppression of bone destruction. In contrast, T cell-derived cytokines may simultaneously enhance the production of connective tissue growth factors, which has stimulatory and proliferative effects on fibroblasts and the microvasculature.
The possibility of suppressing the destructive process explains the absence or delayed bone resorption and restoration of collagen connective tissue during the chronic phase of the disease. Consequently, chronic lesions may remain asymptomatic for a long time without significant changes on radiographs.[21]
The balance that exists in the periodontium can be disrupted by one or more factors, for example, microorganisms “located” inside the root canal. They progress into the periodontium and the lesion spontaneously becomes acute with the reappearance of symptoms.
As a result, during these acute episodes, microorganisms may be found in the surrounding periodontal bone, with a rapid increase in radiographic appearance. This radiographic pattern is due to apical bone destruction that occurs rapidly during the acute phases and is relatively inactive during the chronic period. Consequently, the progression of the disease is not continuous, but occurs in intermittent bursts after periods of “stability.”
Cytological studies show that about 45% of all chronic periodontitis are epithelialized. When epithelial cells begin to proliferate, they may do so in all directions randomly, forming an irregular epithelial mass that contains vascular and infiltrated connective tissue. In some lesions, the epithelium may grow into the entrance of the root canal, forming a filling-like seal at the apical foramen.
Features of the treatment of periodontitis in the acute stage
Exacerbation of periodontitis goes through two phases: intoxication and exudation (appearance of discharge). As the disease progresses, the patient first experiences aching and episodic pain, and then constant throbbing and tearing pain, so treatment cannot be delayed.
Acute periodontitis can be serous or purulent. In the second case, purulent exudate accumulates in the apical part of the tooth root, and the main task for the doctor is to remove it. Sometimes this is enough to clean the tooth cavity and treat the canals, but in severe cases it may be necessary to cut the periosteum for drainage.
Surgery
If the granuloma is large and cannot be removed therapeutically, it becomes necessary to resect the upper part of the root. To do this, the canal is filled with materials that quickly harden but do not dissolve. It is allowed to use the material in excess, since the doctor will remove it later. During the operation, high-quality anesthesia will be required. The dentist cuts the gum and widens the area of the jaw where the granuloma is present. At the site of destruction, the bone and part of the root are cut out and the granulation is scraped out. Instead, an antibacterial substance is compacted and the wound is sutured. It is recommended to install drainage for a day.
There are situations when the entire tooth needs to be removed. Reasons include obstruction of the root canals, lack of treatment effect, closely located mandibular canal, etc. After removal, the inflamed area goes away on its own. But there are cases when it is necessary to make an incision, disconnect the periosteum and install drainage. This manipulation is carried out when there is an accumulation of pus that did not come out during tooth extraction.
Treatment of periodontitis at home
Periodontitis cannot be cured at home, since the disease is caused by bacteria that colonize the dental canals. The only way to get rid of them is to carry out antiseptic treatment and sealing of the canals, and this can only be done by a doctor, but by waiting for a visit to the clinic, you can alleviate the symptoms and reduce pain.
Disinfectants that do not irritate the mucous membranes can be used for rinsing 4 - 5 times a day. Doctors also recommend rinsing with a solution of salt and soda, including after treatment, to relieve swelling and reduce inflammation. Non-steroidal anti-inflammatory drugs are suitable for pain relief. All this will help relieve symptoms, but is not a cure.
You may experience pain after periodontitis treatment. Normally, they last 3–5 days and gradually fade away. If the pain does not subside or returns with renewed vigor, re-therapy is necessary.
Anti-inflammatory drugs
In the treatment of periodontitis, drugs from the group of non-steroidal anti-inflammatory drugs are used, which quickly act on the site of the disease, eliminate pain, and relieve inflammation.
The most commonly used anti-inflammatory tablets for periodontitis are:
- Analgin
- Paracetamol
- Nimesulide
- Diclofenac
- Tempalgin
Nonsteroidal anti-inflammatory drugs often have a negative effect on the mucous membrane of the digestive system, so they should be used with caution by people with stomach diseases.
Periodontitis: how does the disease appear and how does it develop?
Periodontitis is a term dentists use to refer to an inflammatory process that affects the tissues that surround the tooth and help keep it in the socket. The causes of periodontitis may vary in etiology (origin) and the disease is classified into subtypes. Correct diagnosis of the subtype of periodontitis is of fundamental importance: on its basis, the specialist will select the most effective treatment methods. Below we will get acquainted in detail with the forms of the disease, and also consider in detail their characteristic symptoms.
Infectious periodontitis
Dentists have to treat the infectious form of periodontitis in 90% of cases. The disease appears due to infection entering the root canals of the tooth and usually against the background of caries or pulpitis, the timely treatment of which was ignored. Infection in the canal cavities can also occur due to errors in endodontic treatment. The inflammatory process begins to actively develop from the moment pathogenic microflora enters the cavity of the dental canal. As inflammation spreads, not only soft but also hard tissues are destroyed; a granuloma can form, and if left untreated, a cyst.
IMPORTANT: The process of cyst formation can be asymptomatic, but the formation can grow to significant and dangerous sizes and lead to various types of pathologies, including deformation of the jaw joint.
Temporary filling
During a second visit to a dentist-therapist during the course of treatment of chronic periodontitis, the area of manipulation is examined. The specialist will also clarify whether the patient has any complaints of pain, swelling in the gum area or other discomfort. If such negative phenomena are not observed, temporary filling of the dental canals is performed.
For this purpose, the temporary filling is initially removed, as well as the antiseptic placed in the tooth canals. The canal openings are thoroughly washed with an antiseptic and then filled with a special type of composite material used for temporary filling. This composite contains calcium hydroxide, a substance that destroys pathogenic microflora and also catalyzes the process of bone tissue regeneration in the area of the upper zone of the tooth root. Temporary filling of canal cavities is done for a fairly long period - from two to three months. The dentist then places a temporary filling in the crown of the tooth.
How does this pathology manifest itself?
Acute periodontitis is characterized by:
- sharp pain when biting on a tooth;
- feeling as if it has shifted;
- swelling of the soft tissues of the gums;
- increase in body temperature.
In the chronic form of dental periodontitis, the following symptoms are characteristic:
- wave-like appearance and disappearance of pain;
- increased tooth sensitivity when biting;
- periodic formation of a fistulous tract in the gum tissue with the appearance of purulent discharge.