Causes
Vascular occlusions are associated with a state of vascular insufficiency. The occlusion process occurs:
- as a result of injuries, if the artery is compressed.
- due to the fact that the lumen is blocked by a thrombus or embolus.
The formation of blood clots is promoted by a chronic disease - vascular atherosclerosis. As atheromatous plaques grow and increase in diameter, they interfere with normal blood flow. Atherosclerotic plaque leads to blood clotting and blood clot formation. Occlusion is caused by separated plaque fragments that move freely along the vascular bed. In addition, as a result of atherosclerosis, the walls of blood vessels lose their elasticity, become thinner and stratify under blood pressure, which causes the formation of aneurysms. Thrombosis or embolism is likely to occur in the area of the vessel where the dilatation has appeared.
The effect of occlusion on the healing of periodontal lesions
As a result of traumatic occlusion (short-acting factor) or orthodontic treatment (long-acting factor), mechanical stress begins to develop in the periodontal ligament and adjacent areas, which in itself triggers a biochemical reaction from the structures of the dentofacial apparatus. This reaction consists of a whole cascade of biological and chemical stages, the totality of which determines the complex nature of the adaptive properties of the organism.
When pressure is formed in a specific area of the periodontal ligament, compression of the gingival fluid is observed, the alveolar bone bends slightly, and the lumen of the blood vessels in this area is partially or completely blocked, depending on the intensity of the applied force. Even with momentary disturbances in the blood supply to periodontal tissues, oxygen pressure in the blood decreases, which leads to the release of the first markers of inflammation - prostaglandins and cytokines. Hypoxia and the associated disruption of the activity of individual cells, in turn, provokes the development of a process such as aseptic inflammation, mediated by molecules that are associated with the pattern of destruction of body proteins. Essentially, these molecules are endogenous factors that are normally secreted intracellularly, and thus avoid contact with the immune system under normal conditions. However, when cell activity is disrupted, these molecules are released into the intercellular space, triggering the development of inflammation with the participation of prostaglandins, cyclooxygenase-1 and 2 (COX-1, COX-2).
If such mechanisms have the opportunity to develop over several hours, metabolic disorders begin to progress, which are associated with the release of secondary inflammatory markers such as cyclic adenosine monophosphate and tumor necrosis factor alpha (TNF), the latter including the activator of the nuclear transcription factor receptor [ NF-κB] (RANK)/NF-κB receptor ligand (RANKL) and osteoprotegerin (OPG) molecule. These factors stimulate the process of bone tissue remodeling and resorption.
Ultimately, all these biochemical reactions directly affect the work of dental surgeons. During the inflammatory reaction associated with the action of traumatic occlusion, migration of leukocytes (neutrophils and macrophages) is observed in the area of critical action on the periodontal ligament. And if we take into account that this situation can also be observed after certain periodontal interventions, then the risk of developing occlusal trauma among periodontal patients should be clinically completely minimized in order to exclude the possibility of developing secondary iatrogenic complications. This article will examine aspects of the influence of occlusal forces of varying intensity on the structure of periodontal tissues and analyze their potential impact on wound healing after certain periodontal procedures.
Side effects of traumatic occlusion on clinical treatment results
Due to the above-described biological mechanisms of inflammation, occlusal trauma can negatively affect the healing process of periodontal wounds after iatrogenic interventions in the structure of periodontal tissues. That is why signs of tooth mobility and traumatic occlusion should be diagnosed and corrected at the planning stages of future treatment, and not during postoperative monitoring.
Reinhardt et al used finite element analysis to determine which zone, depending on the point of application of force on the periodontal ligament, would experience the earliest inflammatory lesions. For this purpose, the authors carefully studied the specifics of the functioning of the central incisors of the upper jaw. It was interesting that during the study it was possible to establish that the level of alveolar bone reduction turned out to be little dependent on the value of stress in the area of the periodontal ligament until the moment when bone loss had already reached 6 mm. It was also noted that the stress value on the periodontal ligament with the same applied force in the conditions of loss of 4-6 mm of supporting bone tissue almost doubles, thus, the effect of occlusal trauma, in fact, begins to progress. This fact is extremely important for taking into account when carrying out manipulations of directed tissue regeneration, because if the concentration of acting forces is applied to the area of intervention, then the risk of losing the graft and membrane used increases almost immediately several times. Harrel and Nunn discussed in more detail the effect of occlusal adjustments on periodontal tissue. Their study involved 89 people with periodontal pathologies and recorded occlusal parameters. 30 patients were given no treatment, 18 were treated with root surface cleaning and polishing, and 41 were treated surgically for existing pathology. Scientists were able to establish that patients with adjacent existing occlusal problems and deep periodontal pockets are characterized by a worse treatment prognosis and an increase in the level of mobility of individual teeth when comparing the same parameters with a group of patients who did not have any adjacent occlusal disorders. Thus, the authors were able to establish that the presence of uncontrolled occlusal changes in itself is a risk factor for the potential development of periodontal diseases. The researchers also found that teeth that received occlusal adjustments, or that did not have any primary occlusal problems, showed a lower risk of deterioration in their initial condition compared to those teeth that did not undergo proper occlusal adaptation.
The authors were able to establish that teeth with occlusal deviations, the treatment of which was not carried out during complex rehabilitation, were characterized by a more progressive increase in the depth of periodontal pockets with each year of observation. Thus, occlusal trauma clearly affects not only the parameter of tooth mobility, but also the depth of periodontal pockets, compromising the general periodontal status of the patient.
Palcanis also confirmed the presence of changes in the periodontal ligament under the influence of occlusal trauma in a canine animal model. After resection of the coronal part of the teeth, the author introduced a special cannula into the area of the periodontal ligament through the space of the pulp chamber. In this way, it was possible to increase the pressure in the periodontal ligament in isolation, without resorting to more complex options for simulating excessive compression on periodontal tissue. In addition, this approach allowed the author to accurately measure the pressure that was exerted on the periodontal ligament. Biancu, Ericsson, and Lindhe conducted studies to determine how trauma influences existing periodontal destruction by determining how pressure can trigger progressive loss of periodontal attachment. The study was conducted on one-year-old Beagle dogs. Eight dogs had an orthodontic elastic installed, which caused loosening of the tooth crown. The position of the elastic to create the loosening movement was changed from the lingual to the vestibular side and vice versa twice a week for 3 months. At the end of the study, the level of plaque accumulation was also monitored. The results of histological studies demonstrated that the most coronal part of the periodontal ligament showed signs of excessive mobility, a decrease in the amount of collagen in the ligament space and an increase in the number of vessels and inflammatory cells (leukocytes). Interestingly, in the area of the adjacent bone there was also an increase in the number of osteoclasts, and the number of collagen fibers that connected the cementum structures of the tooth with the alveolar socket, on the contrary, was reduced.
Thus, it can be assumed that qualitative changes in the structure of the periodontium are associated with the action of excessive forces that exceed all biological and physiological norms and which provoke the development of tooth mobility.
Elimination of this effect will reduce the risk of developing damage to surrounding tissues and will promote normal healing of the therapeutic wound in the periodontal structure. Brazilian scientists studied the effect of occlusal trauma on the periodontal ligament by deliberately over-biting mice by placing excessively high amalgam or composite fillings. The results of histological analysis showed signs of traumatic damage to the ligament (disorganization of the structure, irregularity of the pattern of the alveolar bone), and the severity of these was greater in the area of teeth restored using amalgam than in the area of teeth restored using composite materials.
Signs of periodontal trauma resulting from occlusal interaction
Trauma due to occlusal interaction (TFO) is a pathological disorder in the structure of periodontal tissues caused by the action of the masticatory muscles. Similar disturbances are observed in cases of parafunctional activity, as a result of iatrogenic interventions, in various forms of malocclusion, as well as during tooth migration. Stillman defined periodontal trauma due to occlusal interaction as “a condition in which damage to the tissues that provide support to a tooth develops as a result of close contact between opposing teeth.” Causes of occlusal-associated injury may include premature contact, parafunction (such as bruxism), and changes in tooth position over time. In addition, the American Academy of Periodontology Glossary of Terms identifies two separate concepts: primary and secondary occlusal trauma. With primary occlusal trauma, teeth with healthy surrounding periodontal tissues are damaged as a result of the action of excessively high occlusal forces. With secondary occlusal trauma, teeth are exposed to normal occlusal forces, but the condition of their periodontium is already compromised, which is why the action of even physiologically acceptable occlusal stresses provokes progressive periodontal damage.
Combined occlusal trauma is a pathology in which excessive occlusal loads act on a tooth whose periodontal condition is already problematic. Based on this, traumatic occlusion can be defined as occlusion that provokes damage to the ligamentous apparatus of the tooth.
Clinical signs of periodontal damage caused by occlusal loads manifest differently in different individuals. Jin and Cao conducted a study in which the authors tried to relate the effect of traumatic occlusion with the severity of periodontitis pathology. For this purpose, the researchers conducted an analysis among 32 patients with moderate to severe forms of periodontal disease at the Beijing Medical University. All teeth that showed increased periodontal probing depth and loss of supporting bone tissue were studied in isolation from teeth that, despite inherent occlusal changes, demonstrated functional stability.
As a result of the study, the authors proposed the use of two indicators - the occlusal-associated injury index and the adaptability index. High rates of the occlusal-associated trauma index characterized the expansion of the periodontal ligament area, increased functional mobility of the teeth, as well as a higher risk of progression of periodontal pockets and loss of periodontal attachment. With high values of the adaptability index, teeth were characterized by the presence of abrasion facets and a relatively lower level of loss of surrounding bone tissue, as well as a very slow decrease in the level of periodontal attachment.
No occlusion
As already described above, mechanical load directly initiates the progression of the bone remodeling process, however, occlusal hypofunction on the other hand (for example, due to the loss of antagonist teeth) provokes the development of initial signs of osteoporosis. The mechanisms themselves that implement the process of bone loss are still not fully understood.
A recent study by Xu et al found that lack of occlusal interaction not only leads to bone loss, but also to architectural changes in the structure of the bone itself. In addition, it turned out that these processes correlate with the activity of sclerostin, a molecule that is secreted by osteocytes and whose action is an antagonist of the Wnt/ß-catenin signaling pathway. By binding to the LRP5/6 receptor, sclerostin inhibits the formation of bone tissue by osteoblast cells. Subsequently, the same molecule induces the promotion of the process of osteoclastogenesis and the expression of RANKL, which are involved in bone tissue resorption. To gain a broader understanding of the mechanisms of bone loss in hypo-occlusion, further studies that focus on the biological and mechanical aspects of bone remodeling are needed.
Phases of periodontal wound healing
Healing of a periodontal wound is an integral stage in the process of rehabilitation of patients after iatrogenic interventions in the periodontal structure. However, this process also involves the implementation of a number of specific stages, the description of which will be given below.
Hemostasis and inflammation phase
The goal of the body's implementation of the hemostasis and inflammation phase in the area of the periodontal wound is to eliminate all possible bacteria and antigens from the intervention area and to achieve primary coagulation in the area of interest. During hemostasis, fibrinogen in the exudate structure triggers the blood clotting mechanism and forms a fibrin mesh. It is thanks to the latter that the bleeding stops. Throughout the entire 24 hours after the intervention, the entire mechanism of the inflammatory response is actively implemented, which includes both cellular and vascular components. The release of histamine and serotonin in the area of intervention causes vasodilation and allows phagocytes to freely migrate into the wound site.
Directed migration of neutrophils occurs due to chemokines, a cascade of complement factors and those peptides that are released during blood clotting. After entering the wound, neutrophils release reactive oxygen fractions, due to which the wound is cleansed. In addition, neutrophils provide the release of proteases that lyse bacterial cells, while the removal of other plaque occurs due to phagocytes. Neutrophils also form so-called neutrophil extracellular traps, which subsequently go through the processes of nuclear and membrane disintegration, chromatin decondensation, cytoplasmic dissolution and diffusion with cytoplasmic proteins. During the implementation of this phenomenon, ruptures of the plasma membrane and the release of chromatin fibers (which are formed from DNA), histones, and 20 other different proteins, including elastase, myeloperoxidase, cathepsin G, proteinase 3, high mobility group of proteins B1, and LL37.18, also occur. The formation of an extracellular neutrophil network also leads to the activation of immune cells, which strengthen the biological barrier in the wound area and provide protection against possible penetration of microbial antigens. Ultimately, the phase of degradation of pro-inflammatory mediators is reached, which makes it possible to reduce the overall volume of inflammation and also ensures the prevention of the development of its chronic form.
If the process of formation and development of the extracellular neutrophil network somehow develops differently than described above, this can lead to chronic inflammation of the periodontal wound and its long-term non-healing. An increased risk of changes in the structure of the inflammatory mechanism is observed in various chronic and autoimmune diseases such as rheumatoid arthritis, systemic lupus and chronic diabetic ulcers. Macrophages are also a critical immunological regulator involved in wound cleansing and inflammation. M1 macrophages of different subtypes ensure the implementation of the stage of direct inflammation, while macrophages of the M2 phenotype are classified as an anti-inflammatory cell phenotype that is involved in the resolution of inflammation and healing of periodontal wounds. Classically, M1 macrophages respond to microbial stimuli (lipopolysaccharides) or cytokines (TNF and granulocyte macrophage colony-stimulating factor [GM-CSF]), while other cytokines (i.e., interleukin [IL]-4, IL-13, IL -33) are associated with the polarization and differentiation of alveolar macrophages into M2 phenotype cells.
Migration phase
The migratory phase involves the movement of epithelial cells and fibroblasts from the edges of the wound towards each other, which results in the closure of the wound surface. Cell migration is a major component in the process of replacing lost tissue and is controlled by cell-cell interactions and local factors.
Proliferative phase
The proliferative phase occurs together with and after the migratory phase (from day 3). At this stage, granulation tissue is formed, which consists of capillary and lymphatic vessels that have grown into the wound area. Collagen is synthesized by fibroblasts, which strengthens the healing area for 14 days. At the end of this period, the density of the vascular component decreases, and signs of edema practically disappear.
Remodeling phase
This phase is characterized by the maturation of cellular connective tissue and thickening of the epithelial layer, which leads to the formation of a scar. In this case, the cellular granulation tissue changes and becomes an acellular mass over a period of several months to 2 years.
The effect of occlusion on periodontal wound healing
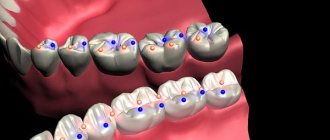
The wound healing process involves a number of stages, including the inflammatory response, its resolution, and structural remodeling with the maturation of periodontal tissue in the affected area. Wound treatment must address multiple stages, including inflammatory response and resolution, as well as remodeling and maturation of the final structure. When healing a wound in the area of the periodontal ligament, it is necessary to take into account the fact of the influence of occlusal trauma from both biological and physiological perspectives, since the factor of traumatic occlusion can provoke not only the development of undesirable changes, but also inhibition of the process of progressive growth of bone tissue. Occlusal trauma can also cause disorientation of fibers in the structure of the periodontal ligament, a decrease in the number of fibers, an increase in the volume of cellular infiltrate, a shift in bone remodeling towards osteoclastogenesis, vein thrombosis, and even necrosis of the periodontal ligament, which has previously been described in the literature. Further progression of the traumatic occlusion factor negatively affects the repair of the periodontal ligament and its adequate blood supply. All of the above negative effects are becoming increasingly important in cases of periodontal healing after dental implantation as part of targeted tissue regeneration, or even in cases of dental trauma. Thus, compression of the periodontal ligament provokes its inflammatory expansion, and, consequently, a decrease in the number of retaining collagen fibers. Photo 1 illustrates the effect of occlusion on wound healing parameters.
Photo 1. Cascade of reactions during wound healing. The negative effect of occlusal trauma on the periodontium includes compression of the periodontal ligament, thrombosis, the formation of an inflammatory infiltrate, osteoclastogenesis and possible loss of the graft used for augmentation. Lymphocytic infiltration and bone resorption may also occur, requiring more invasive periodontal interventions.
Compression of bone tissue leads to an increase in the level of functional mobility of teeth with the surrounding formation of an inflammatory infiltrate. Occlusion of the lumen of blood vessels directly leads to the loss of periodontal attachment and the level of surrounding bone tissue, and a shift of the system towards osteoclastogenesis begins to develop. Aseptic inflammation of periodontal tissue is manifested by the formation of tooth abrasion facets and progressive necrosis of the periodontal ligament under significant prolonged occlusal load. Remodeling of bone tissue under the influence of uncontrolled occlusal forces, although characterized by adaptive thickening of the hard bone plate, is also fraught with vein thrombosis in the bone structure.
Thus, in order to prevent all potential negative consequences, periodontal patients should be carefully assessed for occlusal relationships after performing any surgical and regenerative manipulation of periodontal tissues. Bone loss caused by traumatic occlusion in the absence of bacterially induced inflammation is reversible. The situation is similar with traumatic damage to the periodontal ligament as a result of inadequate occlusal load - if the provoking factor is eliminated, the ligament recovers on its own.
Thus, dentists should pay due attention to the fact of diagnosing traumatic occlusion in all dental patients, and especially in those who have undergone guided tissue regeneration procedures. After all, the harmonious state of the occlusal relationship is also a factor in successfully achieving tissue regeneration around previously affected teeth, or in the area of installed implants.
Clinical applications and conclusions
Based on the available data, the authors can summarize that traumatic occlusion can provoke the development of a detrimental inflammatory effect similar to chronic wounds, which may ultimately negatively affect periodontal tissue regeneration. Additionally, chronic wound inflammation caused by occlusal loading may be exacerbated in the context of other autoimmune disorders or chronic inflammatory conditions (eg, diabetes). In such cases, it is necessary to take all available measures to neutralize such negative consequences. It is also necessary to remember that the wound healing process consists of four phases - hemostasis, cell migration, proliferation and remodeling, which must be balanced with each other and provide a natural mechanism for cleaning and restoring damaged periodontal tissues.
In order to ensure the regeneration of periodontal tissues in conditions of traumatic occlusion, it is necessary to exclude the influence of all identified occlusal inconsistencies (both axial and non-axial), which provoke an increase in the level of biological mobility of teeth in the periodontal structure. All working and non-working occlusal contacts should be checked and adjusted before administering anesthesia so that the doctor is confident that the occlusal correction was made under conditions of normal proprioceptive sensitivity of the patient. In addition, it is important to provide a detailed periodontal diagnosis in the area of potentially problematic teeth, as well as monitoring changes in occlusal guides in the long term after the end of the immediate rehabilitation of the dental patient.
Authors: Ann M. Decker, DMD Hom-Lay Wang, DDS, MSD, PhD
Occlusion of cardiac vessels
A dangerous condition is considered to be acute occlusion of the coronary arteries, which supply blood to the heart muscle. This occurs as a result of atherosclerosis of the coronary arteries and coronary heart disease. If, during the chronic course of the disease, a person experiences angina pectoris, then the acute form is fraught with a heart attack and even death of the patient. Typical signs of cardiac vascular occlusion are chest pain that lasts more than 10 minutes and does not go away with rest or after taking nitroglycerin. In this case, the concept of acute coronary syndrome is used: a patient with such symptoms should be immediately hospitalized.
The danger lies in the fact that a person initially ignores the symptoms of coronary artery disease or simply does not feel them without taking any measures. Vascular occlusion is characterized by suddenness and unexpectedness, so at the first signs of developing coronary artery disease, consult a doctor immediately.
Facial anatomy
The key to understanding the reasons for the development of complications after filler injections is knowledge of the structural features of the face.
Main 5 structural layers:
- Skin (it consists of epidermis and dermis).
- Subcutaneous fat deposits.
- Facial muscles, SMAS.
- Blood vessels.
- Skull bones.
With any contour plastic surgery, there can be either a standard number of dangerous zones or an increased number - if, for example, surgical interventions were previously performed in the facial area. At the appointment, the cosmetologist asks the patient in detail about diseases and operations previously undergone - this allows him to assess the risks as accurately as possible and reduce the likelihood of adverse reactions to a minimum.
Peripheral vascular occlusion
Large arteries of the extremities, more often the lower ones, are susceptible to vascular occlusion. Occlusions are an unpleasant consequence of vascular diseases of the legs. At the same time, the threat of an acute occlusive process in this area is dangerous due to the development of tissue necrosis, which leads to amputation of the affected limb. Characteristic signs of thromboangiitis obliterans, atherosclerosis of leg vessels and other common pathologies are:
- pain in the legs that does not go away with rest;
- pallor of the skin of the extremities;
- coldness in the legs;
- tingling sensation, numbness in the limb;
- impairment of motor functions of the limb.
If these symptoms appear, it is recommended to immediately examine and treat the vessels of the extremities: the slightest delay can result in the development of gangrene. In the early stages of the development of the disease, treatment of obliterating atherosclerosis of the lower extremities and other pathologies of sclerotic origin is carried out using conservative methods, whereas in an advanced form it is difficult to fight the disease.
Occlusive processes occur in the arteries of the kidneys, resulting in the development of renovascular hypertension and kidney dysfunction. The aorta is also affected, since it is the largest vessel. Read about the consequences of aortic atherosclerosis by clicking on the link.
Possible complications: how they manifest themselves and what to do
Any change in skin tone immediately after administration of the drug may indicate vascular ischemia. Symptoms of arterial and venous occlusion are complete discoloration of the epidermis or its darkening to a bluish-gray tint, reticular erythema, ecchymosis, severe headaches. The main thing in this case is to start blood flow processes in the affected area. Ways to do this (done by a doctor!):
- applying a compress (it should be warm);
- massage aimed at dilating blood vessels and uniformly dispersing the drug;
- the use of stimulant drugs to dilate external blood vessels;
- taking aspirin;
- hyaluronidase injections (if problems are caused by hyaluronic acid preparations);
- corticosteroid injections (anti-inflammatory/immunomodulatory drugs);
- taking systemic antibiotics;
- antiviral therapy (indicated when there is a threat of necrosis in the perioral zone).
Hyperbaric oxygen therapy and a course of laser procedures may be prescribed several months after the injection of filler and the development of occlusion. Although this complication is very rare, it is worth knowing about. To avoid damage to the vessels of the retina, fillers are not injected into the area of the glabella and the upper part of the nasolabial folds.
Occlusion of blood vessels supplying blood to the brain
Occlusive processes in the arteries supplying the brain are fraught with dangerous consequences. Impairment of cerebral blood supply is fraught with the development of a stroke or ischemic cerebral infarction, and this often ends in the patient’s death, paralysis or dementia. A common cause of this is carotid artery occlusion. It is accompanied by loss of consciousness, nausea and vomiting, impaired coordination, speech and vision, weakness and numbness of the limbs. A harbinger of strokes are transient (cerebral) ischemic attacks, which we described in detail earlier.
Forecast
Carotid atherosclerosis carries a significant risk of ischemic stroke. With asymptomatic narrowing of the internal carotid artery of more than 70%, the risk of ischemic stroke exceeds 5% per year. If the patient has had episodes of cerebrovascular accidents, then this risk is already 25% per year.
The risk of ischemic stroke in asymptomatic atherosclerotic plaques with a narrowing of less than 70% does not exceed that in patients without atherosclerosis.
After adequate restoration of blood circulation in the carotid arteries, the risk of ischemic stroke is reduced by more than 3 times.
Upcoming events
2021-09-01BASIC COURSE ON DENTAL IMPLANTATION WITH DR. FRIEDMAN FOR STUDENTS AND RESIDENTS (Annual course)
2022-02-05International Implantology Congress
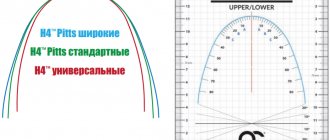
Rice. 7.The force vector is oriented in the orthograde (natural, physiological) direction along the axis of the implants. It should be noted that the central fossa (Fossa) of the lower molar is additionally shifted in the lingual direction, i.e., lingualized.
Front overlays
In orthodontic treatment, frontal overlays are also used, divided into two groups: single and multi-unit.
Types of single front overlays:
- oral – installed on the distal surface of the tooth;
- medial – used when there is slight mobility of the supporting canines;
- shoulder pads – stabilize the prosthesis, used for splinting mobile teeth;
- double-arm rest - used when defects are included in order to replace clasps, installed on the distal side of the fangs.
Multi-link linings come in narrow, medium and widened types. They provide support and stabilization of the prosthesis, but do not fix it. They are used for Kennedy dentition defects on the lower front teeth.