Corrective osteotomies of the knee joint are used
- as an independent method of treating degenerative-dystrophic pathologies of large joints, for some infectious diseases of bones and congenital pathologies;
- as part of one of the stages of complex treatment of arthrosis of various etiologies, at the final stage of which the joint is replaced with an endoprosthesis.
What is corrective osteotomy of the knee joint?
This is a surgical intervention in which, through surgical manipulation of the tibia or femur, the effect of shifting the circular axis of load distribution on the lower limb and giving it a more physiological position is achieved.
The operation corrective osteotomy found its rebirth in the early 2000s; until that time, knee arthroplasty . Recently, the point of view has triumphed that while the patient is relatively young (up to 60 years), the regenerative features of his body are relatively great, and irreversible changes have not yet occurred in the knee itself, leading to its almost complete immobility and wear of the working surfaces over a large area, corrective osteotomy will allow a person to preserve his own joint with a minimal amount of surgical access. At the same time, in the postoperative period, complete restoration of knee function is possible while maintaining all types of physical activity and without reducing ability to work.
Possible complications
Some complications arise already during osteotomy, others during the rehabilitation period.
- Incorrect fusion of bones. Occurs due to improper fixation of bone tissue fragments during surgery. With such a complication, repeated intervention is necessary.
- Non-union of bones. It may occur due to severe concomitant pathologies, smoking, impaired blood supply to the operated area, or osteoporosis. For treatment, a repeat operation is performed and special rehabilitation is prescribed.
- Compartment syndrome. Occurs if, during surgical manipulation, the muscles were strongly compressed by a tourniquet. For treatment, certain drugs are prescribed; if the case is severe, a fasciotomy is performed.
- Improper functioning of the joints located next to the surgical field. This complication is typical for the absence or violation of rehabilitation rules. Exercise therapy is prescribed.
- Infections. They can be introduced during surgery or due to improper wound care. An antibiotic is prescribed for treatment; in severe cases, revision surgery will be required.
- Nerve damage is a surgeon’s mistake or a peculiarity in the location of the patient’s nerve endings. The function of a damaged nerve cannot be restored.
- Thromboembolism. Occurs when anticoagulants are prescribed incorrectly, getting out of bed late, or the inability to wear compression stockings. To eliminate this complication, high doses of antiplatelet agents and anticoagulants are needed.
What types of damage are treated?
With gonarthrosis, there is an uneven distribution of load on the articular surfaces. Most often there are two types of such distribution:
- varus deformity of the limbs (legs - “wheel”) is the most common type of pathology in which the internal surfaces of the joint are affected;
- valgus knees (X-shaped) - when the outer surfaces of the joints are worn out.
The operation is performed only if the articular surfaces are damaged unevenly, on only one side of the knee. In the case of total damage (as in rheumatoid arthritis), the intervention in question is completely useless and absolutely contraindicated.
Contraindications for osteotomy
Osteotomy is an operation. Like any intervention, it has contraindications. According to ISAKOS (International Society of Arthroscopy, Knee Surgery and Orthopedic Sports Medicine), bone correction cannot be performed with the following diagnoses:
- Rheumatoid arthritis;
- Osteoporosis;
- BMI more than 40;
- Impaired blood flow in the lower extremities;
- Extra-articular deformities;
- Previous infection;
- Reduced bone regeneration ability;
- Operations on the meniscus;
- Limitation of flexion more than 25 degrees;
- Some types of arthrosis.
In other situations, surgery can be performed, because for many, corrective osteotomy remains the last chance to return to motor activity, beautiful legs and a full life.
The essence of the operation and the result
The main goal of the intervention is to distribute pressure and friction evenly across the knee joint, reducing this impact on the most affected areas by loading those that are more preserved and functional.
As a result, the axis of the load on the limb is shifted, giving it a more physiological position, and, as a result, a more balanced distribution of the load (and let us remember, when walking it is about four body weights on one knee, when running - about eight), and reducing pressure on the “sick” area of the joint surface.
What are the dangers of malocclusion?
- Violation of dental contacts makes it difficult to chew food and provokes the development of diseases of the gastrointestinal tract.
- Severe malocclusions so limit the possibilities of normal nutrition that they are a reason for deferment from the army.
- Changing the angles of inclination of the teeth affects the distribution of the load during chewing, leads to overload of the periodontium, the development of gum inflammation and, ultimately, earlier tooth loss.
- Teeth crowding, combined with misalignment, affects the natural cleaning of teeth, further leading to the development of gum disease and an increased likelihood of tooth enamel destruction. If tooth loss has already occurred, then violations of the jaw relationships can create difficulties in prosthetics.
- Malocclusion leads to a change in the trajectory of jaw movement during chewing: the temporomandibular joints are overloaded, and dysfunction of the temporomandibular joints develops.
- Some types of malocclusion are anatomical prerequisites for narrowing the airways, for the appearance of snoring and such a serious condition as sleep apnea.
Advantages of the method
- Relatively low invasiveness of the intervention. Surgical access is achieved by making an incision of only about one centimeter;
- follows from the previous one. This manipulation does not always require anesthesia, and in the vast majority of cases it is performed using regional, spinal or epidural (less often) anesthesia;
- as a result of the manipulation, the patient is discharged from the clinic with his knee completely preserved, and, subject to a number of conditions, a complete restoration of its functions is possible;
- the duration of the operation is about one and a half hours, it is well studied, with many years of experience;
- length of hospital stay is about three days;
- the time to return to the full range of activity of the limb is about two months.
Which is preferable: knee replacement or corrective osteotomy?
This question can be encountered in discussions both among patients and in the professional community. Although, objectively, the question of choosing between these manipulations can only be decided if there are contraindications to surgery using the corrective osteotomy method .
In all other circumstances, there are usually two options:
- corrective osteotomy of bones cannot have an alternative in the form of endoprosthetics, since it is aimed at solving completely different problems and is prescribed for other indications;
corrective osteotomy cannot be replaced with prosthetics, since it is only a stage in the strategy of therapeutic measures, the final of which will be knee replacement.
Rehabilitation stage
Severe swelling is something all patients should prepare for after an osteotomy. Swelling will persist for up to 3 weeks. Throughout this period, the person walks with rubber bands that prevent the mouth from opening too wide. For nutrition, soft, semi-liquid and warm food with sufficient calories is recommended. Chewing hard foods is prohibited.
After 4 weeks, the patient turns to the orthodontist, who completes the work on the dentition.
Contact only trusted dental clinics; osteotomy is a rather complex type of operation, so it should only be performed by experienced surgeons with good experience.
Indications for surgery
- age – up to 60 years. At a young age, tissue regeneration, and therefore rehabilitation, occurs faster and more reliably. In old age, the operation of choice is complete joint replacement with an endoprosthesis;
- no signs of obesity. Excess weight will negate all the positive effects of the operation very quickly, and the relief will be short-lived. A vicious circle is started: excess body weight, as a result, increased load on the knee, resulting in a recurrent course of arthrosis;
- rachitic changes in bone tissue. Provides both a reduction in wear on the surfaces of the knee joints and the correction of cosmetic defects;
- deforming arthrosis, gonarthrosis. Together with other recommendations, this is the main and main indication;
- improperly consolidated fractures of the lower extremities and shortening of one of the lower extremities - the principle is the same. Redistribution of the load followed by automatic alignment of the limbs;
- osteomyelitis. When treating this pathology, the infected area of the bone is excised and replaced with an autoimplant. Thus, the focus of the purulent process is removed, and due to autoimplantation of bone tissue, regeneration processes are accelerated.
The purpose of corrective osteotomy of the knee joint
There may be several ultimate goals set by an orthopedist when prescribing surgical treatment, and they depend on the strategic objective:
- can be used as a long-term complex therapy for arthrosis - as an intermediate link in a chain of sequential changes in treatment tactics, from conservative and physical treatment to radical joint replacement;
- used as an independent and main method of treatment for incorrectly consolidated fractures, to eliminate congenital and acquired cosmetic defects of the lower extremities, in the presence of ankylosis and false joints.
Restoring support function
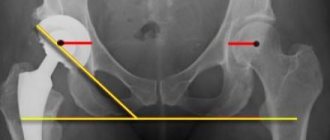
Surgeries aimed at creating a weight-bearing, painless joint are mainly used for coxa vara/valga, neoarthrosis of the femoral neck, chronic cervical fractures, congenital dislocations, and osteoarthrosis. The problem of restoring a supporting function convenient for walking and standing is often solved by changing the axis of the femoral neck. The altered neck-shaft angle changes the fulcrum of the head, which was initially pathological, by several millimeters (up to 15 mm). This approach favors not only the restoration of weight-bearing ability, but also decompression of the joint and reduction of pain symptoms. The cutting of the femur is carried out in the most appropriate way, which is selected on the basis of individual radiological data.
How is the operation performed?
The meaning of the surgical intervention is that an incision is made on the bone on the side of the greatest damage to the joint, a hole of the required shape. After this, the required amount of one’s own bone or cartilaginous substance is placed into this hole, due to which the limb is, as it were, retracted to the side, deviated along the axis of the body in the direction opposite to the pathological process.
Osteotomy with metal structure
Next, the area of the bone where the incision was made with the bone autoimplant placed there is fixed with a titanium plate using screws . Then the access is sutured, and the limb is immobilized using a splint or splint. There is no need to apply plaster.
Types of surgical techniques
- by type of access - open and closed. There are situations when open access, despite being more invasive (when the bone surface is exposed and the incision width is 10–12 centimeters), is preferable. The need for this type of intervention is due to the increased risk of damage to nerves and blood vessels during surgery;
- by level of implementation of interventions. Depending on the location of the pathological process and the goal, excision is performed on the femur or tibia. On the latter, in turn, high and low tibial osteotomies are performed;
- according to the method of excision of bone tissue - wedge-shaped, transverse, straight, oblique, spherical;
- by the nature of the correction - opening, closing.
Knee osteotomy: visual representation of the procedure.
What types of osteotomy are there?
For osteotomy, manual (osteotomes, hand saws, etc.), mechanical (saws, cutters, etc.) and ultrasonic instruments are used. The main purpose of their use is to obtain a thin incision (1–2 mm thick), which will allow the bone tissue to be shifted in the desired direction. To solve this problem, the plastic surgeon chooses an approach (intranasal or percutaneous) and one of three main types of osteotomy:
- Medial.
- Lateral.
- Transverse.
A good plastic surgeon after an osteotomy always takes into account the reduction of free space in the internal structures of the nose for air flow through the nose. To preserve nasal breathing function after bone osteotomy, the nasal dorsum is reconstructed using cartilage tissue from the nasal septum area.
Rehabilitation
Rehabilitation measures after corrective osteotomy of the knee joint using plates with angular stability usually last no more than four weeks. There are often cases when the period of rehabilitation measures can increase significantly. This is due to the individual characteristics of the patient, but the largest share in such cases is due to ignoring the recommendations of the attending physician and non-compliance with the conditions and timing of the postoperative period. If you strictly follow the rehabilitation plan, the chance of developing complications or delaying the healing process is minimal.
The patient begins to perform the first sets of physical therapy exercises while still in the hospital (the inpatient treatment phase takes from three days to a week). In the postoperative period after corrective osteotomy of the knee joint, rehabilitation measures are aimed primarily at restoring blood circulation and maintaining full trophism of the limb. At this time, exercises for bending and extending the leg at the knee, massages of the feet and hips, symptomatic, restorative, antibacterial therapy and anticoagulants, cold on the leg are indicated. The patient walks on crutches (about three months); putting weight on the operated limb is absolutely contraindicated.
The main role in rehabilitation belongs to physical therapy. The load on the joint should be gradually increased. The number of exercise therapy exercises and their duration increase; at later stages, exercise classes on an exercise bike and swimming are prescribed. During the recovery period, physiotherapeutic procedures are required.
The entire period of rehabilitation and full restoration of performance takes from six months to a year.
Among the methods of surgical expansion of the atrophied alveolar ridge (AC), a special place is occupied by intercortical osteotomy, based on the vestibular movement of the outer cortical plate in the edentulous area [1, 4, 5, 11, 15, 16].
Its advantages in achieving long-term results of dental implantation are presented in a number of publications [2, 3, 8, 10], etc. However, it is reported that it is problematic to ensure the primary stability of a dental implant (DI) and the optimal thickness of the soft tissue covering it, or the so-called biological the width of the adjacent gum, which is understood as the zone of connective tissue and epithelial attachments to the coronal part of the bone crest [9, 13, 14]. There are also conflicting opinions about the structure of the cut-out flap, which promotes better blood supply to the osteotomized fragment in the postoperative period [14, 17], and the rationality of simultaneous elimination of soft tissue deficiency [6, 7, 12].
This report presents the main surgical stages of the AMCO alveolar intercortical osteotomy technique, patient selection criteria and some aspects of the prevention of postoperative complications.
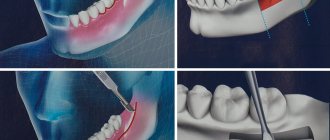
Surgical intervention begins with cutting out a combined (full-thickness in the caudal part, split-thickness in the cranial part) flap on the outer side of the corrected area of the AH, where dental implantation is planned; then, through an intercortical osteotomy, vestibular movement of the outer bone wall is performed to increase the width of the ridge.
Dissection and detachment of soft tissues
Rice. 1. An incision along the ridge and skeletonization of the vestibular surface of the coronal part of the alveolar process.
A linear horizontal incision is made:
— within the keratinized attached gum;
- along the apex or palatal cranial edge of the ridge, in the space between 2 adjacent teeth or supposed vertical cuts (in the absence of teeth);
- with dissection of the periosteum, i.e. to the bone;
— in the form of intrasulcular and marginal incisions in the area of the gingival papillae of adjacent teeth, while the gingival edge of the tooth neck remains intact.
An important condition when dissecting tissue is, if possible, preventing the lines of bone cutting and suturing the edges of the wound from coinciding in order to reduce the likelihood of developing postoperative complications in the form of divergence of its edges and infection.
Peeling of the combined flap begins with skeletonization of the apex of the bone AG approximately 3-4 mm from the vestibular (crossing the mucogingival border) and palatal sides, including in the projection of adjacent teeth. In fact, at this stage of the operation, the coronal part of the vestibular flap is cut out, including the periosteum (Fig. 2).
Rice. 2. Formation of a combined flap; in the coronary part the flap includes the mucoperiosteal layer, and in the apical part it includes a split layer.
Next, the periosteum is dissected along the entire length of the flap (Fig. 3), penetrating with the tip of a scalpel into the wound 1-2 mm parallel to the surface of the bone (to prevent perforation of the usually thin mucous membrane in this area - SO) with the intersection of the existing muscle attachments. Further detachment of the flap is performed: a) acutely; b) on top of the periosteum, i.e. in the submucosal layer; c) to the projection of the upper fornix of the vestibule of the oral cavity, holding the scalpel parallel to the surface of the movable S.O. Thus, the large or apical part of the combination flap, approximately 6-7 mm wide, is split, since the periosteum is not peeled off. This allows you to preserve the blood supply to the bone and increase the mobility of the relocated flap, while avoiding additional vertical loosening incisions, which has a beneficial effect on the trophism of local soft tissues.
Rice. 3. Mobilization of the flap by linear incision of the periosteum.
In those clinical observations when, in order to improve the long-term functional and aesthetic results of AMCO, it is necessary to increase the volume of the attached gum (if its thickness is less than 2 mm) and (or) eliminate recession in teeth adjacent to the implantation zone, the so-called bilaminar technique according to G. Zucchelli is used (2013), the essence of which is the coronal movement of the vestibular flap in combination with a free connective tissue graft (CTT).
When expanding the edentulous narrow AG in the frontal part of the upper jaw (MF), it is necessary to take into account that the contour of the outer surface of its ridge usually has a concave shape, which is unfavorable for achieving aesthetic results of dental implantation. Recreation of the convex shape of the outer contour of the ridge is achieved as follows: immediately after a horizontal cut to a depth of 8-10 mm, a wedge-shaped chisel is installed into the resulting intraosseous lumen and expanded to 2 mm, then in the projection of the planned dental implantation a drill with a diameter of 2.0 mm is used to form osteotomy hole, which is gradually enlarged in the bucco-lingual direction using a special set of expanders1. By successively using expanders of increasingly larger diameters, they compact the spongy substance, move and “straighten” the outer bone wall, the thickness of which, as has been repeatedly noted, should be at least 2 mm. Next, vertical cuts are made through intraosseous access in a manner similar to that described. In addition, a feature of surgical intervention in the anterior part of the HF is the location of the DI neck deeper than the cemento-enamel junction by 3 mm, which corresponds to the biological width. The latter, as is known, is composed of 3 anatomical structures of the gum: the gingival sulcus, zones of epithelial and connective tissue attachments.
Intercortical osteotomy
carried out using 2 cuts, starting with a horizontal one in the middle of the apex of the bone AG (Fig. 4); then 1 vertical cut is made from its medial and lateral ends. The splitting of the ridge within the made cuts is carried out by vestibular movement of the outer cortical plate according to the type of subperiosteal fracture at its base.
Rice.
4. Horizontal cut in the middle of the apex of the AG using a piezo scalpel. The success of horizontal cutting is ensured by the following technical techniques: a) minimize bone loss during splitting using thin instruments (piezo scalpel, diamond disk, cutters, sharp chisel, etc.); b) crest osteotomy is performed to the cancellous bone and somewhat in the outer direction, maintaining the thickness of the vestibular bone plate (VBPL) within 2.0-2.5 mm; c) all bone cuts are made at a distance of at least 2 mm from the roots of adjacent teeth.
Vertical loosening dissections of the compact layer of bone (Fig. 5) are performed: a) with a piezo instrument or a fissure carbide bur installed intraosseously, followed by advancement to the vestibular side; b) perpendicular to the horizontal cut, starting from the top of the ridge (from its medial and lateral ends, respectively) for approximately 8-10 mm; c) at a distance of at least 2 mm from the projection of the periodontal ligament of the tooth adjacent to the intervention zone; d) being careful not to injure the proper periosteum.
Rice. 5. Vertical cuts were made in the compact layer of bone.
The osteotomy is completed with a thin pointed chisel, which, through a horizontal dissection of the bone, is installed into the resulting gap between the outer and inner cortical plates to the depth of the vertical cuts (Fig. 6). In this intraosseous position, the chisel is tilted vestibularly from the basal part of the ridge, and at the base of the osteotomized bone fragment it is broken (a “greenstick” fracture) on the periosteal pedicle and moved. To control the displacement of the fragment, the index finger is placed on the outer surface of the VCP. The palatal bone plate must remain intact.
Rice. 6. A thin chisel is inserted into the cut to carry out the final stage of the osteotomy.
At this stage, the resulting wound defect is assessed to determine the advisability of immediate or delayed implantation according to the standard protocol. Depending on the stability of the displaced VCP on the periosteal pedicle, implantation can be carried out in 1 or 2 stages. It is very important that after the splitting is completed, the minimum thickness of the bone walls is at least 2 mm; otherwise, it is recommended to use delayed D.I. setting. In a two-stage protocol, the intraosseous space is first filled with osteoplastic material (OPM) and implantation is performed in a delayed period after bone regeneration has been achieved. The use of OPM also makes it possible to prevent the return of split cortical plates to their original position. Small gaps (1 to 3 mm wide) are often restored without additional bone grafting. When performing dental implantation, the resulting intraosseous space is additionally filled with autologous bone chips obtained using burs or a scraper. To improve graft stabilization, a barrier membrane is used.
Formation of the bone bed and installation of DI
After completion of the intercortical osteotomy at the level of the base of the AH, guide holes are prepared using cutters with a diameter of no more than 2-2.5 mm of the corresponding implant system, which are installed during the same surgical intervention, provided that sufficient primary stability of the externally retracted VCP is achieved (Fig. 7). In this case, it is necessary to minimize its trauma by: a) preserving cancellous bone on it; b) palatal position of the osteotomy hole (taking into account the dentoalveolar arch and occlusion); c) carefully screwing it into the formed DI bed (Fig. 8).
Rice. 7. The vestibular bone wall is retracted using an expander.
Rice. 8. The bone expander is screwed into the prepared implant bed.
In the lateral section of the HF, a prerequisite for successful primary stability of the DI is its immersion by 2/3 of its length into the bone tissue and 0.5-1 mm below the free coronal edge of the ridge. For the same purpose, a movable VCP can be additionally attached to the palatal bone wall using microscrews. To prevent ingrowth of surrounding tissues, a plug is installed in the internal threaded channel of the DI (Fig. 9).
Rice. 9. Installation of intraosseous DI.
When deciding to carry out delayed implantation, the surgically created gap between the cortical plates must be filled with osteoinductive and (or) osteoconductive material (Fig. 10), which is left for 4-6 months. A mixture of autogenous bone chips obtained from nearby areas using a bone scraper and xenogeneic material (Bio GEN, Gen Os, Easy Graft, etc.) is used as OPM. If necessary, provide coverage of the OPM with a barrier membrane, which is installed under the inner surface of the detached mucoperiosteal flap so that it covers the entire outer surface of the introduced material.
Rice. 10. The bone deficiency is filled with bone replacement material, and a bioresorbable barrier membrane is laid.
Suturing the edges of the surgical wound
Rice. 11. Suturing the wound.
After completion of the regenerative intervention or installation of the DI, the cut out flap is moved caudally and, without tension, fixed with separate interrupted and horizontal mattress sutures (5/0 or 6/0 diameter) to the original attachment site. At the same time, the existing removable or bridge prosthesis is relined to prevent contact with the surgical wound.
Patients with removable dentures are not recommended to use them until the sutures are removed (i.e., within 10-14 days after surgery). Subsequently, the removable dentures are repositioned so that they do not place excessive pressure on the implantation area.
It should be understood that in some cases, AMCO is the most realistic treatment option that allows for optimal results. Deep knowledge of the topic of anatomical bone and soft tissue structures, analysis of these and clinical and radiological data before the upcoming surgical intervention can reduce the risk of unforeseen technical problems associated with it and unwanted side effects in the postoperative period.
The South Korean Split help kit contains 5 expanders with a diameter of 2.5 to 4.5 mm, which makes it possible to install a DI of the optimal size.