Why does my mouth start to burn?
In the ICD, burning mouth syndrome is called glossodynia. This can be an independent diagnosis or a symptom that accompanies another disease. Researchers have not found a single reason why your mouth suddenly feels scalded.
After many tests, the diagnosis is often given the word “primary” or “idiopathic”. This means that the cause of the burning pain in the mouth could not be found. There is a hypothesis that the basis of the disease is damage to sensory and pain receptors.
Among the causes of secondary glossodynia are:
- gastroesophageal reflux, also known as GERD;
- allergies to food, mouthwash, or denture material;
- hormonal changes due to hypothyroidism, diabetes, or menopause;
- dry mouth as a result of radiation therapy or due to “breakage” of the salivary glands;
- high blood pressure medications such as enalapril, perindopril and others;
- lack of iron, zinc and B vitamins;
- excessive cleaning of the tongue, especially with abrasive pastes;
- fungal infections of the mouth.
Introduction
Burning mouth syndrome (BMS) is considered ambiguous in terms of pathogenesis and one of the most difficult to treat interdisciplinary pathologies.
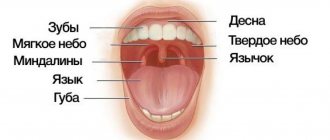
SHR is represented by a clinical triad of symptoms: burning of the tongue, dry mouth and changes in taste in the absence of visible damage to the oral mucosa. Patients describe their unpleasant sensations as burning, tingling, tingling, itching, numbness, and crawling. In approximately half of the patients, the burning sensation is combined with pain in the tongue of aching or pressing nature of varying intensity. Symptoms are usually bilateral and localized in the anterior 2/3 and lateral surfaces of the tongue, on the lips, gums, and inner surface of the cheek. But the most common localization of burning is the tip of the tongue. More than 70% of patients experience taste disturbances, a sensation of bitter and/or metallic taste. Up to 2/3 of patients complain of dry mouth. A patient with the above complaints can seek advice from a doctor of any specialty. The rare diagnosis of SGR is due to both low
prevalence and lack of awareness of doctors about this syndrome. According to international studies, the diagnostic search sometimes lasts up to 7 years [1].
OHR is defined as a chronic disorder characterized by a burning sensation and dysesthesia in the oral cavity, recurrent daily for more than two hours a day for more than three months and without any clinically obvious lesions or damaging causes [2]. Other names for SGR are found in the literature: glossodynia, oral dysesthesia, glossopyrosis, stomatopyrosis and stomatodynia.
SHR is more common in older people (the average age of onset is about 60 years) and is quite rare in patients under 40 years of age [3]. The prevalence of SGR, according to international studies, ranges from 0.6% to 15% [4, 5]. This disorder is diagnosed predominantly in peri- and postmenopausal women, with a female to male ratio of 7:1 [6].
According to the third edition of the International Classification of Headache Pain (ICHD-3, 2018), SGR belongs to the 13th chapter “Cranial neuralgia and other facial pain” (13.11 Burning mouth syndrome).
ICHD-3 formulates diagnostic criteria for SGR [2]:
Oral pain meeting criteria B and C.
Repeat daily for 2 hours or more per day for three or more months.
Pain has both characteristics:
burning sensation;
felt superficially in the oral mucosa.
The oral mucosa shows no damage or changes, including sensory testing.
Does not correspond to a greater extent to another diagnosis from ICHD-3.
According to the International Classification of Orofacial Pain (ICOP Version 1.0 beta 2020), SGR belongs to the 6th group “Idiopathic orofacial pain”, the diagnostic criteria are almost identical to the criteria specified in ICHD-3, but two types of SGR are distinguished depending on the presence or absence of somatosensory changes during somatosensory testing [7].
In ICHD-3 and ICOP Version 1.0 beta 2022, the term “SGR” is used for idiopathic cases without any cause. Since numerous local and systemic diseases, as well as medications, can cause similar symptoms, the formulation “secondary” or “symptomatic” HRS is quite logical, but this term is not included in these classifications [8]. Thus, an accurate determination of the location of the syndrome in the structure of facial pain and the use of diagnostic criteria in clinical practice will contribute to further research into SGR and the provision of adequate care to patients.
How to put out a fire in your mouth?
If a burning sensation in the mouth accompanies the underlying disease, then eliminating the disease should relieve the unpleasant symptoms. Treatment for primary burnt mouth syndrome is more like a series of experiments. The British National Health Service advises to accept that the treatment process may take years.
Ways to relieve mild burning include:
- moisturizing mouth sprays, otherwise called saliva substitutes;
- lidocaine-based rinses;
- regular cool drinks;
- avoiding acidic foods, spicy foods and alcohol;
- using toothpaste for sensitive teeth;
- combating stress and anxiety: yoga, meditation, cognitive behavioral therapy.
Severe, burning pain in the mouth is treated like any other chronic pain: with anticonvulsants or low-dose antidepressants.
Diagnosis of glossalgia
These sensations can appear at any time of the day, often intensify in the evening, and rarely occur at night. These manifestations may be for no apparent reason, or may occur or intensify after irritating food, the burning sensation may completely disappear while eating non-irritating food. This is an important diagnostic sign of the syndrome.
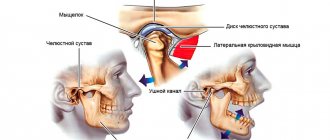
Burning sensations may be accompanied by swelling of the tongue with tooth marks along its edges, small cracks in the tongue, mild soreness of the tongue and taste disturbances often occur.
Patients may have neuropsychiatric disorders: disorders of the autonomic nervous system in the form of increased heart rate (tachycardia), sweating, pale skin, increased tendon reflexes, obsessive-compulsive neurosis, depression, etc.
The patient is advised to consult specialists: dentist, neurologist, gastroenterologist to exclude glossitis (inflammation of the tongue caused by infection, chemical irritant, injury to the tongue, allergies) and B12 and folic anemia, which causes burning and pain of the tongue with its characteristic changes: bright red, smooth and a shiny (varnished) tongue.
Classification by symptoms
Doctors distinguish three main types of manifestation of glossalgic syndrome. Assigning a specific clinical case to one of them helps to more accurately outline the causes of the problem.
- Type 1 . In the morning the patient wakes up without pain, but during the day it appears and gradually progresses, reaching a peak in the evening. Most often, such symptoms are combined with a lack of nutrients (iron, vitamin D), as well as systemic disorders (diabetes). Occurs in 35% of patients.
- Type 2 . The pain is constant, with almost no change in intensity throughout the day. In many patients, the burning sensation does not subside at night, which causes sleep disturbances. Symptoms are characteristic of various psychological disorders. Observed in 55% of patients.
- Type 3 . Symptoms are inconsistent, there is no clear localization and description of pain. At different periods, symptoms may intensify and disappear completely. Many experts associate this course of the disease with allergic reactions. It occurs significantly less frequently than other variations, in 10% of cases [1, 2].
Why does post-Covid syndrome occur?
Coronavirus is an insidious disease that can affect almost all organs and systems:
- upper respiratory tract;
- bronchi and lungs;
- nervous system;
- gastrointestinal tract;
- cardiovascular system.
Post-Covid syndrome can occur regardless of the form of coronavirus in a person: latent, mild, moderate, severe or critical.
Currently, there are several hypotheses that try to explain the formation of post-Covid syndrome. One of them claims that pathological symptoms after coronavirus are manifestations of chronic thrombusculitis.
Everyone has heard of such a complication of coronavirus as pneumonia, which affects the lungs. However, this is far from the most common complication of infection. With COVID-19, severe pneumonia occurs in only a small proportion of patients. Much more common is inflammation of the walls of blood vessels in the brain, which can continue after coronavirus.
This hypothesis partially explains some symptoms of post-Covid syndrome, but not all. Modern medicine has yet to find the exact causes of its occurrence and fully evaluate the consequences.
How does post-Covid syndrome manifest?
Signs of post-Covid syndrome can be divided into several groups. Let's look at each of them in detail.
Symptoms of general health problems
The main signs of impaired general well-being after coronavirus include:
- attacks of weakness. Weakness can be so severe that a person is forced to remain in bed for several weeks;
- a sharp decrease in exercise tolerance. Even a little activity leads to complete exhaustion of physical strength;
- disruption of the rhythms of life. Insomnia, excessive drowsiness, sleep inversion (waking at night, sleeping during the day) may develop;
- muscle pain. With a coronavirus infection of any form, there is always a significant decrease in protein mass, which negatively affects the condition of the muscles.
Psycho-emotional problems
Today we can draw conclusions that coronavirus negatively affects the psycho-emotional health of people. With post-Covid syndrome, the following may be observed:
- depressed mood. Almost all patients who have had coronavirus are in a minor mood. They develop despondency, depression, and melancholy. In some cases, depressed mood can lead to suicidal thoughts;
- unstable emotional state. Manifested by sudden mood swings, low self-control of behavior;
- panic attacks. People experience attacks of severe anxiety in combination with other symptoms: high blood pressure, shortness of breath, nausea, dizziness.
There are currently known cases in which a severe disturbance of the psycho-emotional state after coronavirus has resulted in suicide.
Symptoms associated with respiratory complications
Such signs can occur even if there was no damage to the respiratory system during the acute phase of coronavirus. These include:
- feeling of lack of air;
- tightness in the chest, inability to take a deep breath;
- bronchospasms.
Bronchospasms are characterized by a decrease in the lumen of the bronchi. With this complication, hypoxia develops - a lack of oxygen in the body.
Symptoms associated with complications of the respiratory system can last from several days to several months.
Neurological manifestations
The coronavirus is able to penetrate the central nervous system, affecting neurons and glial (auxiliary) cells. The main neurological manifestations of post-Covid syndrome include:
- intense headaches. The pain syndrome can be constant or in the form of a migraine - a paroxysmal, recurring headache;
- violation of thermoregulation. Some people have a low-grade fever (37–37.5 degrees) for a long time after COVID-19, while others have a low temperature (up to 36 degrees);
- chills, especially in the evening. Accompanied by a feeling of cold, muscle tremors. At the same time, body temperature can remain normal;
- visual impairment. A person may experience black spots before the eyes, blurred vision, photophobia;
- paresthesia is a sensitivity disorder. Manifested by a sensation of burning, tingling, crawling on the surface of the skin;
- disturbance of smell and taste. Such symptoms can last up to several months.
Another common complication is a malfunction of the vestibular apparatus, which is responsible for the ability to navigate in space and maintain balance. If the coordination system is disrupted, the gait becomes unsteady, a person can crash into any obstacle or fall out of the blue.
Symptoms associated with damage to the cardiovascular system
A distinctive feature of COVID-19 is its pronounced impact on the cardiovascular system. In every fifth patient, the infection causes arrhythmia, acute or chronic heart failure.
With sweating syndrome, the following may be observed:
- blood pressure disorder. Both high blood pressure and prolonged hypotension can develop. In addition, orthostatic collapse often develops. The condition is characterized by insufficient blood flow to the brain when there is a sudden change in body position. With orthostatic collapse, a person’s blood pressure quickly drops, vision becomes dark, dizziness and fainting occur;
- polymorphic dermal angiitis. It is caused by an inflammatory process that develops in the walls of blood vessels. It manifests itself in the formation of nodules, blisters, plaques, hemorrhages, blisters, bruises, and dark spots on the skin. Polymorphic dermal angiitis is one of the complications of thrombovasculitis;
- heart rhythm disturbance. After coronavirus, a person may experience arrhythmia, tachycardia, or a slow heart rate for a long time.
Many patients with post-Covid syndrome note that when they remain in an upright position for a long time, they experience weakness, dizziness, and cold sweat. Such signs are a consequence of a drop in blood pressure.
Gastrointestinal tract disorders
The consequences of COVID-19 often include disruptions to the digestive system:
- decreased intestinal motility, which slows down the movement of food through the gastrointestinal tract;
- stool disorder. Both constipation and diarrhea may develop;
- loss of appetite.
This triad of symptoms often causes dysbiosis - changes in the composition of the normal intestinal microflora. In an advanced state, dysbiosis can lead to decreased immunity, severe anemia, and allergic reactions.
Symptoms associated with disruption of other organs and systems
In addition to the listed pathological signs, the consequences of COVID-19 may be:
- decreased immunity;
- inflammatory processes of the urinary system;
- malfunction of the sexual sphere. Women often experience menstrual irregularities;
- endocrine diseases;
- allergic reactions.
It has been proven that coronavirus primarily affects organs affected by chronic diseases.
At the same time, during the post-Covid syndrome, hidden diseases that a person did not even suspect about often worsen. Therefore, people who have recovered from coronavirus infection need to be very careful
take care of your health and immediately contact a specialist if you experience any unusual symptoms.
How to quickly recover from coronavirus?
There is no magic cure for the effects of coronavirus. Rehabilitation after coronavirus can last from several months to a year. The list of rehabilitation measures depends on the individual characteristics of the patient and may consist of the following elements:
- therapeutic exercises;
- breathing exercises using respiratory simulators;
- massage;
- psychotherapy;
- diet therapy;
- physiotherapeutic procedures.
An effective method of rehabilitation after coronavirus is hyperbaric oxygenation - exposing the body to oxygen under high pressure in a pressure chamber. With coronavirus, hypoxia often develops. Hyperbaric oxygen therapy can eliminate it.
An important element of rehabilitation is the intake of vitamin-mineral and amino acid complexes, which help strengthen the immune system. The most important vitamins for post-Covid syndrome are A, D, E, C. Amino acid complexes compensate for the lack of protein in the body, which affects the production of immunological protective antibodies.
Online consultation with infectious disease specialist, allergist-immunologist Natalia Nikolaevna Gordienko
Cost of online consultation: 3500 rubles
Online consultation
During the consultation, you will be able to voice your problem, the doctor will clarify the situation, interpret the tests, answer your questions and give the necessary recommendations.