Features of dental canal treatment
Differences in the structure and functions of the “representatives” of the dentition largely determine the nature of the treatment approach. Treatment of canals for different groups of teeth has its own nuances.
Front tooth canal treatment
The front teeth most often have one canal. They are often curved and difficult to pass through for instruments. In order to preserve aesthetics, the opening of the cavity of these teeth is carried out from the vestibule of the oral cavity. Due to their frontal location, it is important to prevent tooth enamel from darkening, so filling materials containing dyes are not used.
Treatment of wisdom tooth canals
Wisdom teeth can have more than 5 canals; they often have a branched structure, which is not always revealed by x-ray examination. These factors, along with the marginal location of the “eights”, significantly complicate the high-quality treatment of root canals. At the final stage of treatment, various filling pastes are traditionally used.
Root canal treatment of temporary teeth
Endodontic treatment of tooth root canals is usually used only at the stage of root stabilization. When choosing the optimal treatment tactics, it is necessary to take into account the specific structure of temporary teeth. The small thickness of the canal walls, the insignificant degree of dentin mineralization and the relatively large size of the apical foramen are the main reasons for special caution during instrumentation. Zinc oxide eugenol and iodoform pastes, as well as materials based on calcium hydroxide, are usually used as filling agents. They are not toxic to the permanent tooth germ and are able to dissolve along with the temporary root.
How to independently determine pulp inflammation?
Sometimes, with pulpitis, it is difficult to determine the direct source of pain - that is, the most painful tooth - since the pain sometimes radiates throughout the entire jaw. Most often, a diseased tooth reacts to cold, so the easiest way to determine it yourself is to touch all teeth in turn with something cold. For example, a piece of ice from the refrigerator. Of course, this is the most artisanal method, and it is not suitable for normal diagnosis, but at a doctor’s appointment you can at least point out the tooth that definitely hurts more than the others.
This diagnosis includes an x-ray examination of “suspected” teeth. A high-quality orthopantomogram allows you to 100% accurately identify a pulpitic tooth: in such an X-ray image, the border of the tooth surface and the border of the inflamed pulp will be located very close to each other. There are other obvious signs indicating pulpitis that can be seen on such an image - a hidden carious cavity at the root of the tooth, enlargement or dilation of blood vessels, etc.
Stages of tooth canal treatment
Endodontic treatment usually lasts several hours and includes a number of stages.
- Removal of the pulp (pulpectomy).
The inflamed soft tissue of the tooth is eliminated. - Root canal sanitation.
The procedure is a “cleaning” of bacteria and dead tissue elements. Pulpectomy and canal sanitation pursue one of the most important goals - eliminating existing inflammation. - Channel formation.
The root canal, freed from pathological contents, undergoes appropriate treatment. In addition to ensuring good passage of the canal, it is imperative to ensure that its apex reaches the apical part of the tooth. - Canal filling.
The last stage of the intervention is filling the root canal with filling material, followed by grinding.
Dentists' mistakes when filling canals -
- Incorrect measurement of root canal length –
Root canals in a tooth must be filled strictly to the apex of the tooth root.
To do this, it is necessary to correctly determine the length of each root canal. Errors at this stage lead to the fact that the canals are either filled not to the apex of the root, or the filling material is carried beyond the apex of the root, directly into the bone. In the unfilled part of the canal, an infection develops, which leads to the formation of inflammatory foci at the apexes of the roots of the teeth, for example, apical granulomas or radicular cysts, which is accompanied by periodic suppuration and the appearance of pain when biting on this tooth. Refilling the canals can also lead to long-term pain, neuralgia, numbness of the lip and chin.
- Poor quality mechanical processing of the canals - such processing is necessary to widen the canals and give them a slightly conical shape. Only under this condition can they be sealed later. Numerous mistakes by the dentist at this stage (insufficient expansion of canals, formation of steps, root perforations) lead to subsequent poor-quality fillings and, again, to the development of inflammatory complications requiring new expensive retreatment.
Treatment of teeth with problematic root canals
Filling dental canals
A relatively simple technology for treating tooth canals is filling with a special paste with or without a pin. According to the “gold standard” of endodontics, the canals are also filled with a latex-like material - gutta-percha. Several methods of its use have been developed, including the Termafil system, lateral condensation, injection or liquid thermogutta-percha (vertical condensation). In some cases, in particular when treating a tooth canal cyst, filling is carried out with a substance based on calcium hydroxide (copper-calcium hydroxide “depopheresis” method). However, special nanocomposite materials are increasingly used in dentistry.
Treatment under a microscope
The age-old “tough nut to crack” for the dentist is curved or branched root canals of the teeth. A dental microscope, often in combination with a laser, allows you to completely pass through them and adequately process them along their entire length to reduce tissue trauma. Sometimes it becomes necessary to treat a sealed tooth canal with the evacuation of remaining material of various nature, for example, fragments of fillings, tissue fragments and even instruments. Then a microscope also comes to the rescue. Read more about the technology in a separate article.
In what cases are the nerve and pulp removed?
- Pulpitis and spread of carious destruction;
- Periodontitis;
- Several carious cavities at once or one, but large carious cavity;
- Mechanical trauma to the tooth (impact, chipped tooth, bleeding from the roots).
Of course, if there is an opportunity to keep the tooth “alive” and leave the nerves and pulp, the doctor will certainly take advantage of it. However, with pulpitis or severe damage, there is one difficulty: there are no 100% methods that would cure pulp inflammation. That is, if once it becomes inflamed, then with a high probability it will be an irreversible process. Of course, if you looked into a tooth with a microscope, you could accurately determine whether the pulp can be cured, or whether it is easier to remove it - but the problem is that you cannot look at a living patient under a microscope, and dentists are not pathologists after all. Therefore, to avoid risk, the pulp is almost always removed.
Also, in some cases, the pulp is removed before prosthetics.
- especially if the original, natural tooth has been severely damaged. In addition, when using metal-ceramic prosthetics, most of the tooth is still filed down, and during this process, the nerve can be damaged - so it is also easier and more reliable to remove.
If your tooth hurts after root canal treatment
If after root canal treatment your tooth hurts when you press it, this is normal. This phenomenon is associated with insufficient anesthesia in the area of endodontic intervention. Another reason why a tooth hurts after canal treatment is excessive treatment with the instrument moving beyond the apical foramen.
How long does a tooth hurt after root canal treatment? Sometimes pain persists for several days due to intensive intervention in the tissue structure in such a limited area. A similar situation occurs when an excess amount of filling material is placed into the canal, which causes discomfort when pressure is applied to the walls. As a result, the tooth “aches” after canal treatment. In any case, the presence of post-filling pain signals the need for a second visit to the dentist.
Dental clinic No. 2
In order to always anticipate surprises, the doctor must be prepared to expand access to the dental cavity to facilitate the preparation of complex root canals and carefully examine the floor of the tooth cavity to look for such anatomical variations.
Endodontic dogma is that careful cavity and root canal preparation and obturation is the key to successful canal therapy. Endodontic preparation can be divided into cavity preparation (coronal preparation) and root canal preparation (radicular preparation). Transferring the principles of preparation of carious cavities according to Black in relation to endodontics, the following endodontic principles of preparation can be distinguished: creation of external, comfortable, retention (holding) and resistant forms. A complete preparation along the entire length of the tooth is the external form. In turn, the external shape can be modified for a comfortable shape to accommodate anatomy, canal curves and instrumentation. In some endodontic techniques, the canal can be prepared with slight retention of the first gutta-percha point (retention form). But the most important is the resistant form, in which the so-called “apical stop” is prepared in the apical section, a barrier that protects the tissues of the apical periodontium from the removal of the filling material and irrigating solution beyond the apex and creates a limit for the compaction of gutta-percha in the canal (Fig. 1).
| pic 1 |
Basic tools for preparing a tooth cavity. For trephination of an intact tooth crown, Ingle JI suggests using a cone-shaped fissure bur with a working rounded top for a turbine tip (Fig. 2 B). It is first directed at a right angle in the long axis of the tooth to remove only the enamel. Then it should be located parallel to the longitudinal axis of the tooth (Fig. 2 C, D). The roof of the tooth is removed using a low-speed tip with a round bur (Fig. 2 E, F) No. 2, 4 less often No. 6 of regular length (9 mm) for molars and premolars or surgical length (14 mm) for incisors and canines. The protrusion (“shoulder”) inside the cavity of the anterior teeth, which prevents the direct passage of the endodontic instrument into the root canal, is eliminated using a long, conical diamond bur on a turbine drill (Fig. 2 G). The remaining pulp from the pulp chamber is removed using a spherical bur No. 1 or 2 (Fig. 2 H).
| pic 2 |
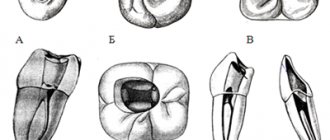
It is necessary to remember the following axioms of the structure of the coronal cavity of the tooth and root canals when searching for root canal orifices (Ingle JI). 1. The two root canal orifices of the first maxillary premolars are located further buccal and lingually than is usually realized (Fig. 3 A). 2. The orifices of the mesiobuccal canals of the upper and lower molars are located under the mesiobuccal cusps, and the external shape should often be more expanded due to these cusps (Fig. 3 B, C). 3. The mouth of the palatal canal in the upper molars is located not so far to the palatal wall of the tooth cavity, but in the center of the medial half of the tooth (Fig. 3 B). 4. The orifice of the distal-buccal canal of the upper molars is not located so distally-buccally, but almost directly to the buccal side of the palatal canal (Fig. 3 B). 5. The orifice of the distal canal in mandibular molars is not so distally located, but in fact almost exactly in the center of the tooth (Fig. 3 C, E). 6. The orifice of the mesial-lingual canal of the lower molars is not so far mesial-lingual, but in fact directly buccally from the orifice of the distal canal (Fig. 3 B). 7. Certain anatomical variations that occur quite often: The mesial buccal root of the maxillary first molar often (up to 95% [4]) has an additional mesiopalatal canal located exactly oral to the orifice of the main canal. The mouth of the additional channel is located in the groove, which forms the mouth of the main channel like a “comma tail”. This entire groove should be examined to locate the mouth of the accessory canal (Fig. 3 B). The lower second molar often has a common mesial orifice, which divides approximately 1 mm below the floor of the dental cavity into mesial buccal and mesial lingual canals (Fig. 3 D). The lower first and second molars may have two distal canals with separate orifices or a common one. orifice, like the previously described medial canals (Fig. 3 E). The mandibular first premolar often has a second canal that branches off from the main canal buccally or lingually a few millimeters below the floor of the dental cavity (Fig. 3 E). The lower incisors and canines often have two canals. The medial lingual canal is hidden under the internal protrusion (“shoulder”), which corresponds to the lingual girdle. This protrusion should be removed with a #2 long shank round bur or finishing diamond cone bur to allow proper exploration of the root canals (Figure 3 G).
| pic 3 |
Table 1. Degree of deviation of teeth from the central axis
When preparing a tooth cavity, it is necessary to take into account the degree of deviation of the tooth from the central axis in the vestibulo-oral and medio-distal projections (Table 1). The upper incisors and canines are inclined palatally by 29°, the lower incisors are inclined lingually by 20°. The lateral lower and upper incisors are deviated medially at 17 and 16? respectively. If the doctor does not know about these deviations or ignores them, then he can make a perforation and a ledge on the walls of the tooth cavity (Fig. 4. A, B, C)
| pic 4 |
Table 2. Incidence (%) of root canals.
For successful endodontic treatment, it is also extremely important to know the variations in the number of root canals in order to avoid the error of missing a canal. Although back in 1921, Hess W., studying 513 teeth, indicated that four canals were found in 54% of the first molar, this fact was ignored. F. Pineda, J. Cutler (1972), studying the medial buccal roots of the first molars, found that in 39% of cases this root has one canal, in 61% - 2 canals. Later studies (J.K. Kalild and D.D. Peter, 1990) showed that in a study of 51 medial buccal roots of the upper first molars, a two-canal variant of the structure was identified in 95% of cases. Table 2 summarizes information from various authors about the frequency of occurrence of additional channels. As follows from this table, in the lower incisors, canines and premolars it is always necessary to look for the second canal, and the first upper molar should be considered a four-canal. Lower premolars can be extremely difficult teeth to treat endodontically. Two narrow canals are usually located vestibulo-orally; division into two roots can occur in the apical third. At higher magnifications, it is often possible to view more complex anatomy. The dentist’s knowledge of the anatomy of the tooth cavity and root canals is an important part of endodontic treatment, guaranteeing the success of the treatment and avoiding errors and complications.
Author: Trigolos N.N.
Possible complications
Not all cases go smoothly. Let's consider the main problems that arise after the procedure.
- Perforation.
The phenomenon is the formation of holes between the dental canals and surrounding tissues. Treatment of perforation consists of medicinal treatment and filling. - Cheek swelling.
The reason why the cheek is swollen after root canal treatment is believed to be the impregnation of the periodontal tissues and mucous membranes with an anesthetic drug, which themselves are quite loose and easily absorb liquid. - Instrument fracture.
The probes for passing through the channels are very thin. If they break during medical procedures, the fragments are removed with special devices. Modern dental instruments made of nickel-titanium alloys are less susceptible to wear and break less often. - Adverse reactions to medications.
The range and severity of side effects of modern anesthetics are minimal. Before treatment, the doctor must collect an allergic history - information about drug intolerance - and the likelihood of a full-blown allergic reaction is practically reduced to zero. Adverse reactions of moderate and minor degrees are mostly short-term, can be easily corrected or can be overcome by changing the drug. - Other complications.
Situations such as swallowing particles of fillings, tooth dust, and small instruments now practically do not occur thanks to the use of a rubber dam - a latex plate that separates the tooth or teeth being treated from the oral cavity.
When inflammation begins - diseases and treatment
The internal structures of the tooth can become inflamed as a result of rapid development, caries, pulpitis or periodontitis. To determine the exact cause of the problem and the stage of development of the pathology, the patient must undergo an x-ray examination. The standard treatment regimen is as follows:
- the doctor removes an old filling or opens a carious cavity to open access to the insides of the teeth,
- if the nerve is still there, it is removed using a special instrument - depulpation is performed,
- Next, the doctor carefully cleans the canals and treats the walls with an antiseptic,
- fills the canals and fixes the filling on top. When treating periodontitis, to ensure the elimination of inflammatory processes, it is usually necessary to apply medication and install a temporary filling - and this procedure will have to be completed more than once.
“My root canals were cured in just 2 visits. It’s a pity, of course, that the nerve had to be removed. They say the tooth can darken. But the treatment was quite quick and easy, and there were no problems afterwards. I heard that sometimes people go for several months to clean out the roots, but at my second appointment they gave me a permanent filling. By the way, it was the first time they filled with gutta-percha, and it still has the same smell!”
KirillMigo, from correspondence on the forum www.32top.ru
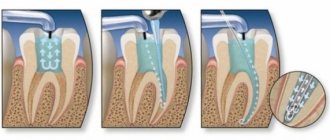
The photo shows a treatment regimen for periodontitis.
The treatment regimen described above is a universal scenario that can be changed depending on the type, shape and stage of the pathological process. But the essence remains the same: it is important that all passages are thoroughly cleaned and sealed. Otherwise, relapses of inflammatory processes are possible, and then the risk of complete tooth loss will increase significantly.
When is tooth extraction necessary after root canal treatment?
It happens that you have to part with a treated tooth. Typically, such a sad outcome is due to the following factors:
- initially unsatisfactory root canal treatment with the development of poorly controlled inflammation;
- some cases of wisdom teeth treatment;
- the complexity of the anatomical structure of roots and canals in a particular patient;
- late request of the patient for specialized help, in which adequate therapeutic measures do not lead to the desired result.
What is pulpitis of a single-canal tooth?
Inflammation of the neurovascular bundle located inside a tooth with one root canal is called pulpitis.
The disease develops as a result of infection getting inside the tooth. The main reason for the development of pulpitis is the advanced stage of caries. When inflamed, the pulp swells and puts pressure on the inner walls of the tooth. The person experiences severe pain. Symptoms of the development of pulpitis of a single-canal tooth are:
- Acute pain. In some cases, pain becomes stronger when a person moves to a horizontal position.
- The presence of a reaction to temperature changes. The symptom manifests itself when eating cold or hot food.
- Reaction to sour and sweet foods.
- Attacks of throbbing pain that appear at regular intervals.
If symptoms occur, you should contact a qualified professional. Failure to visit the dentist in a timely manner can lead to the development of the disease and its development into a chronic form. The constant use of painkillers is not advisable, since they eliminate pain but do not have a therapeutic effect. Failure to contact a specialist in a timely manner will lead to gradual tooth decay.
What is the cost of treatment?
How much does root canal treatment cost? The cost largely depends on the method used and the quality of the materials. When using laser and microscopic technology, nanocomposites and other advanced developments, the cost of tooth treatment with canal filling increases significantly. Approximate prices for root canal treatment in Moscow with gutta-percha filling and composite filling are presented in the table below.
| View | Price |
| Single channel tooth | 9,500 – 12,5000 rubles |
| Double channel tooth | 11,000 – 14,500 rubles |
| Three-channel tooth | 13,500 – 17,000 rubles |
The cost of root canal treatment should not be the determining factor in choosing a clinic. Contact only dentistry with a good reputation and experienced specialists who use modern equipment and the latest techniques in their work. Remember - the future fate of your teeth and the aesthetics of your smile depend on the quality of canal treatment!
Features of the structure of the root system in children
Each baby tooth has one nerve, just like the molars. In addition, they have a similar root system structure. In pathological processes, temporary elements are also opened, processed and filled, but the tactics largely depend on how long ago they erupted and how much time is left before the bite changes. Thus, the roots of baby teeth are usually filled with a special paste, which dissolves as the root system dissolves.
The process of root formation in permanent incisors, canines and molars takes about three years. If the root system is still at the stage of its development, special compounds are chosen for filling it - pastes with a high concentration of fluorine and calcium.
The photo shows the process of resorption of the roots of baby teeth
Number of roots and canals
The human mouth contains special organs – teeth. They are endowed with a specific shape and structure. They are systematized into dairy and indigenous ones. There are 20 milky ones, 32 indigenous ones. In the rarest cases, organs appear beyond the set.
Any unit contains a crown, root and neck. The chewing organs are endowed with 2 and 3 roots with canals. On top of the crown there is enamel, which protects the masticatory organs from injury and is considered a durable tissue (A collection of different and interacting tissues form organs)
human body.
Dentists' tips for disease prevention
The development of dental pathologies can be prevented only by following the advice of trained doctors and observing the rules of oral hygiene.
So, for prevention purposes, dentists advise:
- Do not abuse the rules of hygiene, brush your teeth only in the evening and during the day. The most common effect on tooth enamel is its abrasion;
- hygiene procedures must be carried out half an hour after eating;
- use rinses to destroy bacteria remaining in the mouth after cleaning;
- Cleaning should be carried out for at least 3 minutes, performing radial movements.
The basic rule is in case of detection of the first signs of the disease (disruption of normal functioning, performance)
, you must contact your dentist immediately. This will help prevent the upcoming development of pathology and preserve teeth.