Condylomas of the penis and foreskin are the result of infection with the human papillomavirus, which is expressed in the pathological proliferation of epithelial cells in the form of papillae on the mucous surface of the penis. Genital warts are contagious and can develop into genital cancer, so they cannot be left untreated.
Appointment with a urologist - 1000 rubles. Comprehensive pelvic ultrasound - 1000 rubles. Appointment based on ultrasound or test results - 500 rubles (optional)
CLICK TO MAKE AN APPOINTMENT or ultrasound tests
Causes of condylomas on the penis
The content of the article
You can become infected with the virus only through sexual contact (not only genital, but also oral and anal); it is extremely rare that the infection is transmitted through household means.
At first, the virus does not manifest itself and can remain dormant for years. The appearance of condylomas is facilitated by a decrease in immunity caused by other diseases: influenza, ARVI, gastritis, STIs, stress, climate change, etc. Also, condylomas grow with changes in hormonal levels associated with male menopause and other reasons. When multiple genital warts appear, the urologist diagnoses “condylomatosis.”
Diagnostic methods
A preliminary diagnosis is made based on the patient's complaints and examination of the oral cavity. The doctor must take a swab from the tongue, through which the true cause of the disease (causative agent) is revealed. Additionally, a blood test is prescribed.
If the diagnosis does not reveal the causative agent of glossitis, other procedures are performed. In particular, the body’s reaction to certain substances is assessed (the allergen is determined) and the digestive organs are examined.
Why are genital warts dangerous for men?
The appearance of condylomas is caused by HPV strains No. 6, 11, 16, 18, 30, 42-45, 51, 52 and 53, accounting for about 2% of all types of papillomavirus. Moreover, it is these strains that are oncogenic and cause cancer in more than half of the cases. The most dangerous of them are types 6, 11 (to a lesser extent), 16 and 18.
In addition to oncology, condylomas cause other troubles:
- Psychological trauma
. Men are embarrassed by sexual diseases and are afraid of injuring tumors, so they restrain sexual activity. - Infection
. Condylomas come into contact with underwear, causing injury, and the same thing happens during washing. The infection easily penetrates the wounds, leading to inflammation. - Inflammation of the prostate
. Decreased sexual function leads to stagnation of secretions in the prostate and prostatitis.
Other complications are possible and are described below.
How does condyloma of the penis and foreskin develop?
The development of genital warts in men is more difficult to detect than in women. The virus has a long incubation period ranging from several weeks to 3 years, lasting an average of 2-3 months. First, it travels throughout the body through the bloodstream and inserts itself into the DNA of the cell, disrupting its division. Only at the end of the incubation period do the affected epithelial cells come to the surface in the form of pointed growths on the mucous surfaces of the genital organ.
A sick person is quite capable of infecting his sexual partner with dangerous HPV, even without having any symptoms! Moreover, the presence of HPV in the body does not mean the simultaneous appearance of condylomas. According to scientists, one or another strain of the virus is present in 62% of all inhabitants of planet Earth, but not everyone is diagnosed with condylomatosis.
The trigger mechanism for the development of the disease is external factors.
These include:
- injuries to the surface of the skin on the genitals (fissures of the anus, microtraumas of the frenulum);
- weakened immunity due to the presence of another disease (flu, hepatitis, pneumonia, etc.)
- stress and depression, which reduce the body's defenses;
- passion for saunas, cedar barrels and other types of overheating of the genitals;
- hypothermia;
- various infections (ureaplasmosis, pyelonephritis, trichomoniasis);
- frequent visits to solariums or prolonged exposure to the sun.
Prevention
Strong immunity, hygiene and safe sex are the best prevention of infection with genital warts.
- strengthening and maintaining the body’s defenses (immunity) at a high level;
- maintaining a healthy lifestyle: good fortified diet, adequate sleep, moderate physical activity;
- complete cessation of bad habits: smoking, alcohol, taking various medications;
- If possible, avoid stressful situations, increase mental stability;
- monitoring the general condition of the body, regular preventive examinations by doctors, laboratory diagnostics;
- timely treatment and control of chronic diseases;
- maintaining a sexual life with a regular partner, following the rules of contraception;
- avoid injuring the skin of the penis and adjacent areas to avoid infection;
- careful adherence to the rules of personal and intimate hygiene.
Compliance with medical recommendations and monitoring the state of the immune system prevents the development of viral activity and associated complications. The patient will get rid of the infection by carefully following the doctors' instructions, changing his lifestyle and streamlining his sex life. Self-medication in such cases is strictly contraindicated.
How does HPV, which causes condylomas on the genitals in men, manifest?
The first alarming thoughts arise when a man discovers skin growths on his genitals that look like cauliflower inflorescences or small papillae. In homosexuals, condylomas also appear around the anus. They are also localized on the scrotum, frenulum, and at first do not cause concern. But over time, the tumors gather in groups, itch and cause microtrauma.
Depending on how strong a person’s immunity is, the human papillomavirus has four stages of development. Stages of development of condylomatosis:
- Incubation period
. Lasts from several weeks to several years. The disease does not manifest itself in any way; it can only be detected by PCR analysis. - Initial stage
. On the head of the penis and foreskin, single papillary-shaped neoplasms are noticeable, matching the color of the skin. They do not cause pain or discomfort. If the immune system is restored and the patient undergoes treatment, the condylomas disappear on their own. Many men do not want to hope for a miracle and turn to a urologist to remove tumors. - Chronic form
. Condylomas merge into groups resembling cauliflower inflorescences. The affected areas are itchy and make urination or sexual intercourse difficult. Here it is definitely necessary to remove condylomas. - Launched form
. Condylomas have affected nearby areas of healthy tissue, which dies, rots and emits a foul odor. Any mechanical trauma to the tumor leads to the degeneration of the epithelium into cancer cells. There is no way to do this without surgery.
Types of processes
Most often, flat or pointed warts form in the oral cavity:
- Flat formations have a small protrusion above the mucous membrane and tissues, their shape is predominantly round. Condyloma differs in color from the general background in a brighter shade, so identifying it is quite simple. It is quite dense to the touch and is localized on the lower part of the tongue and oral mucosa.
Flat build-up
- Pointed papillomas form individually in the form of nodules or as a whole family, which makes them similar to cauliflower. They are moderately soft and elastic to the touch.
Pointed growth
Another type of growth is condylomas lata, which are localized not only on the tongue, but also on other parts of the oral mucosa. The reason for their appearance is syphilis.
How is condylomatosis transmitted and how to protect yourself from it?
There are three common ways of transmitting HPV, which leads to the appearance of condylomas on the male genital organ.
- Unprotected sexual contact and protected sex with a sick partner
. Even using a condom does not protect 100% from the virus. During sexual intercourse, cells of the affected epithelium penetrate the mucous tissues of a healthy partner, and this is the most common method of infection among people 18-35 years old. - During childbirth from mother to child
. The baby is born already infected, and neoplasms on the child’s penis can be seen already in the first year of life. - Contact and household method
. This happens extremely rarely, mainly in conditions of lack of sanitation (when using one razor, a shared towel or comb) and only if there is microtrauma on the surface of the skin.
A person can be a carrier of HPV, but he or she will not develop condylomas until the carrier of the virus has a weakened immune system. In this case, the affected epithelium will begin to multiply atypically (with the formation of cells unusual for this tissue), forming condylomas on the surface.
Condylomas pose the greatest danger to women, in whom in 99.9% of cases the disease is the cause of cervical cancer, therefore, upon learning about your disease, you must definitely warn your partner. Girls who are promptly vaccinated with the Gardasil vaccine against HPV have a lower risk of infection. By the way, this vaccination is also given to young men.
Preventive measures
Use mouthwash after meals.
Preventing the development of a disease is always easier than fighting harmful microorganisms and the results of their vital activity. To prevent the formation of growths in the oral cavity, the following measures are recommended:
- perform hygienic cleaning of the mouth at least 2 times a day;
- after eating, use a mouthwash;
- develop a diet so that it contains mainly fresh vegetables and fruits (to strengthen the immune system);
- regularly visit the dentist for preventive examinations;
- do not borrow other people’s household items (dishes, towels, cosmetics);
- undergo an annual examination with an oncologist;
- lead an active lifestyle (if you work sedentarily, include morning exercises and twice-a-day workouts on simulators in your daily routine).
Complications of condylomatosis: genital warts are very dangerous!
If you ignore tumors on the genitals or glans, the following problems will arise:
- Spread of condylomas to the urethra
. They block the urethra, leading to inflammation and viral urethritis. - Viral infection of the rectum
leads to the formation of paraproctitis, which interferes with bowel movements, causes severe pain, bleeding, and is difficult to treat. - The exophytic nature of condylomas
is that they grow inside the organ. - Condyloma has the ability to degenerate into a cancerous tumor
. With reduced immunity, the virus that infects the epithelial cell (the upper layer of the skin) begins to produce new cells that differ in structure from the maternal one (atypical). This is how condyloma degenerates into cancer. - Condylomas have an unaesthetic appearance
, causing disgust in the partner. A man may experience psychological and even physical discomfort during sexual intercourse, which significantly reduces the quality of sexual life. - Men suffering from diabetes mellitus have wide lesions of the foreskin, and their inguinal lymph nodes become inflamed.
- Phimosis
develops - the inability of the foreskin to expose the head of the penis. - In advanced cases, pus accumulates around condylomas, and the patient experiences unbearable pain.
- Condylomas located at the opening of the urethra impede the passage of urine and cause general intoxication of the body, which leads to decreased vitality, drowsiness, poor health, and depression.
In 100% of cases, the patient’s regular partner also becomes infected with HPV.
What to do at home if a growth appears - folk methods
In addition to traditional treatment of growths under the tongue, many patients use traditional recipes. It is impossible to replace treatment with a completely unconventional method, but nothing prevents you from trying it.
Popular folk recipes for growths under the tongue:
- daily rubbing of the formations with garlic juice or applying cloves of spice;
- lubricating newly appeared growths with egg white;
- treating affected areas with castor oil (using cotton swabs);
- rinse the mouth twice a day with decoctions of medicinal herbs (medicinal chamomile, string, sage, echinacea, etc.);
- ingesting rosehip decoction, freshly squeezed potato or carrot juice.
Any infections and viruses developing in the body signal a decrease in immunity, so during the treatment period you should take care of taking fresh vegetables and fruits. A good vitamin complex is also suitable for these purposes.
Before using an unconventional approach, you should consult your doctor to rule out contraindications.
How are condylomas of the penis and foreskin diagnosed?
There are various diagnostics aimed at identifying the presence of HPV in the human body, as well as the oncogenicity (ability to produce cancer cells) of condyloma. The most common methods for identifying genital warts:
- Visual examination of the genitals and anus by a urologist or dermatologist
. To visualize atypical cells, the doctor covers the condylomas with acetowhite rayon, and the oncogenic cells are stained against the background of unstained healthy epithelium. - Biopsy
. This is a sampling of tumor tissue to determine its cellular composition. The most dangerous are strains 16 and 18, which degenerate into cancer cells; - Polymerase chain reaction test
, which uses biotechnology to detect DNA and RNA of a virus foreign to the body. This method can confirm the presence of human papillomavirus, but does not determine whether the cells are cancerous or degenerating. - Tests for HIV and tests for sexually transmitted infections. Condylomas appear when immunity decreases, and, in parallel with HPV, other infections can develop in the body;
- Test - urethroscopy.
If neoplasms are suspected, an internal examination is performed on the urethra.
Urologists
Erkov Igor Viktorovich Urologist andrologist
Cost of admission 2500
₽
Make an appointment
Fomenko Alexander Pavlovich Urologist andrologist
Cost of admission 2500
₽
Make an appointment
Removal of condylomas from the foreskin and glans penis
HPV today is an incurable disease, because there is no medicine that would destroy the virus itself, but relapses are successfully removed. The sooner treatment is started, the greater the chances of getting rid of condylomas.
Treatment methods are divided into surgical and conservative. The latter include:
- Immunotherapy to enhance immunity
. It should be noted that immunostimulants should be taken carefully and only after consultation with a doctor, because they contribute to the development of oncology. Those. If you already have cancer, it will only get worse! Immunomodulators used in the treatment of HPV are of two types: based on interferon-alpha-2 (Altevir, Intron-A, Realdiron) and stimulators of interferon protein production by microphages and lymphocytes (Cycloferon, Arbidol, Amiksin). - The use of ointments that stop the proliferation of condylomas
(Oxolin, Viferon, Aldara cream, Panavir gel, Epigen cream). They are applied to the affected areas of the skin, stopping the further spread of atypical cells, healing tissues and increasing the intracellular production of interferons. - Immunostimulants and ointments
are used as a general course for several months in the initial stages of the disease. Their use is effective only for single small-sized condylomas.
Treatment of ulcers under the tongue
If a parent discovers a sore in the child’s tongue area, he should immediately take him to a dentist for examination. This is the doctor who deals with such diseases. He will conduct an examination and, if necessary, ask the patient to see a doctor of another specialization.
Traumatic ulcer during teething
To make a diagnosis, the doctor must talk with the patient. This will allow us to understand the nature of the lesion in the oral area. A microscopic examination will also be required.
The easiest way to understand how to treat ulcers that appear as a result of mechanical damage. As a rule, they heal fairly quickly if the affected area is provided with suitable care. To quickly get rid of a sore that has formed under the tongue, you must immediately treat it with an antiseptic. Can be used:
- hydrogen peroxide;
- brilliant green;
- propolis spray;
- soda solution.
Propolis spray effectively heals wounds
This antiseptic treatment is usually prescribed for stomatitis. Additionally, vitamin complexes are prescribed.
Individual therapy must be selected for each patient. In addition to treatment with an antiseptic, the attending physician may prescribe:
Painkillers. They contain benzacaine or lidocaine. Ointments and gels based on corticosteroids. Flucinocide is especially in demand. In particularly severe cases, corticosteroid drugs are used. They are necessary for patients who suffer from recurrent aphthous stomatitis.
Squamous cell carcinoma at the bottom of the tongue
If the ulcers were caused by herpes, the patient is prescribed the use of local medications, this may be Acyclovir ointment. Candidal stomatitis cannot be defeated without antifungal drugs, which are used in local and internal treatment.
When stomatitis is accompanied by deterioration in health, namely fever, inflammation of the lymph nodes and exacerbation of a number of diseases, then the patient is immediately sent to the hospital. It is very difficult to cure a patient, especially a child, at home in such a situation.
Tongue herpes in a child is very painful
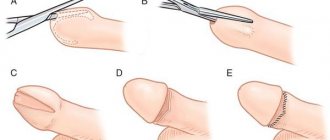
How to remove condylomas of the penis and foreskin
Surgical methods for eliminating condylomas include:
- Electrocoagulation.
An effective, inexpensive, but painful method. It involves applying an electric current to the condyloma, causing it to fall off, leaving a small scar. The method is already outdated. - Cauterization with a solution of acetic and nitric acid
. As a result, the condyloma tissue dies, and it dries out and falls off. Used on separately located large condylomas. The method is not recommended, as surrounding healthy tissue may be damaged, and healing on the penis will take a long time. - Cryodestruction
. This is the effect of ultra-low temperatures of liquid nitrogen on an atypical area, as a result of which condyloma cells change structure and self-destruct. This is a painless method that does not leave scars. But it is effective for small, separately located condylomas. - Laser removal
. The method is painful and requires local anesthesia. Depending on the size of the condyloma, the doctor selects the depth of exposure of the laser beam. It burns out the base of the condyloma, it is deprived of nutrition and falls off, leaving no scar. - Surgical removal
with a metal, argon, plasma scalpel. Used to remove large condylomas located in groups. Requires stitches and long healing. - Radio wave method
. The most modern, effective and painless method. With the help of radio waves of various frequencies, the condyloma is completely excised and disappears. The nearby healthy tissues remain intact, and the patient is left with no scars. The relatively high cost of the method (from 500 rubles per tumor) is dictated by the high cost of complex professional equipment.
Effective methods of traditional medicine
Not only traditional, but also folk medicine can tell you what to do to heal ulcers in the mouth under the tongue. Our great-grandmothers used their own recipes that helped them overcome this disease.
Condyloma acuminata can develop into cancer
As soon as a person discovers a painful rash under the tongue, he should immediately rinse his mouth thoroughly. This is the most effective method of combating the disease. The easiest way to rinse your mouth at home is with a solution based on baking soda. To make it, you need to mix one teaspoon of the product in a glass of warm water. Additionally, you can apply a paste of the same soda to the affected area.
Herpes inflammation of the tongue in an adult
Fans of radical methods of getting rid of mouth ulcers can try treating them with salt. It also needs to be rinsed. A teaspoon of salt should be mixed in one glass of water. It is allowed to add a couple of drops of iodine to the medicinal solution to enhance the effect.
It is necessary to rinse your mouth with salt or soda every three to four hours.
It is also recommended to carry out the procedure after eating. Rinse can be prescribed even for children, as it is completely harmless.
Soda and honey - folk remedies
Natural honey will help disinfect an inflamed wound and speed up its healing. Children will especially like this method of getting rid of unpleasant rashes under the tongue. To remove the ulcer, you need to slowly dissolve a piece of honey. You should also chew honeycomb or propolis. All these bee products have the same healing effect.
A cyst under the tongue requires surgical removal
To quickly get rid of ulcers in the tongue area, you need to use medicinal herbs.
Is it possible to protect yourself from the human papillomavirus?
To date, there is no medicine that would destroy the virus itself. But you can get a vaccination that protects the body from oncogenic strains of HPV. It is advisable to get the vaccine at the age of 9-17 years, and it is effective only for uninfected boys. It is of no use to those who are HPV carriers.
People under the age of 45 can be vaccinated; later it is no longer effective. If you vaccinate an uninfected young person under the age of 26, this will protect him not only from genital warts, but also from oncological processes of the male genital organs.
Currently, the most effective vaccine for men against penile cancer is Gardasil. It protects against oncogenic strains 6, 11, 16, 18, and the Gardasil-9 vaccine will additionally protect against non-oncogenic strains 31, 33, 45, 52 and 58.
The vaccination is done in three stages: the first vaccination is given in the shoulder muscle, the second is given 2 months later, and the third is given several months after the first, depending on age. The drug Gardasil does not contain living or dead viruses, it only contains particles similar to the DNA of the virus. The vaccine also does not contain mercury or the toxic antiseptic component thiomersal. The effectiveness of Gardasil vaccination is 97.9%.
The drug is used in 125 countries of the world, and in 20 of them it is a mandatory item in the vaccination card. It has few side effects, but causes blood thickening, so it is contraindicated for people with bleeding disorders and thromboembolism.
Vaccination may be accompanied by fever and general malaise, but some discomfort is not comparable to the effectiveness of the drug and its ability to protect the body from HPV.
Why do ulcers appear under the tongue?
An ulcer under the tongue occurs due to an inflammatory process of an erosive nature. An abscess can be caused by various factors. It is very important to identify the cause that provoked the disease. After all, this is the only way the doctor will be able to prescribe effective treatment to the patient.
The most common causes of mouth ulcers include:
Leukoplakia under the tongue - the spot cannot be removed
Development of stomatitis
It can be of three types, namely candidal, aphthous and herpetic. The second option is more common. This stomatitis is chronic, so it cannot be completely cured. Therefore, from time to time the patient will experience a sore under the tongue and in other parts of the oral cavity.
Mechanical damage to the oral mucosa
This reason is often explained by the appearance of ulcers on the frenulum of the tongue in a child. He may get hurt on cutlery or scratched by candy. Simply biting your tongue is enough to create a wound on it.
Frenum injury - rupture
Just one microcrack can cause serious inflammation in the mouth. It develops into an abscess due to the active activity of bacteria. Within a few hours, the first symptoms of the disease will begin to appear in a child or adult. If you do not provide first aid to the patient, the infection will spread throughout the entire oral cavity.
Hematoma on the frenulum after trimming
Somatic disease
Often a white sore is one of the symptoms of a dangerous disease that affects the human immune system. These diseases include tuberculosis and HIV. Ulcers will begin to appear due to poor personal hygiene, as well as decreased immunity.
Varicose veins under the tongue with inflammation
To find out why ulcers appeared under the tongue in an adult or child, you need to ask the patient about his health and find out if he was injured several hours before the onset of the inflammatory process.