When people say “my mouth is watering,” they usually mean that something looks and smells delicious. Alas, for those who suffer from hypersalivation, this expression takes on a different, much less pleasant meaning. Increased salivation may indicate health problems. Hypersalivation is often a side effect of a particular disease. If you think your body is producing too much saliva, consult your dentist or physician.
Below is some general information about saliva to help you better understand what to do about excess saliva.
Salivary glands – increased salivation and dry mouth
There are a number of tips to help keep
your salivary glands healthy:
First, you need to drink plenty of water. Secondly, you should use chewing gum that does not contain sugar. And thirdly, it is necessary to suck on lollipops, which also do not contain sugar.
In certain cases, your dentist may recommend gargling with artificial saliva. The above drug is sold in spray or liquid form. You do not need a prescription to purchase it, but use it several times a day. However, artificial saliva does not contain proteins, minerals and other necessary elements that are contained in natural salivary fluid. Thus, the above drug will simply be useless for digestion.
The role of saliva
As experts explain, saliva performs several important functions at once: it washes away food debris from the teeth, softens food, facilitating its subsequent digestion, and even supplies teeth with calcium, strengthening them. Indeed, chronic dry mouth is often a harbinger of caries. However, our body must produce exactly as much saliva as is necessary to ensure these important processes, and not a drop more. Drooling and the need to constantly swallow saliva can be signs of increased saliva secretion, which can cause a lot of discomfort.
Excess saliva in the mouth
By and large, a large amount of saliva is not a problem if the condition is not systemic. Typically, the amount of saliva you produce depends on what you drink or eat. In a healthy person, the body easily eliminates excess salivation. In general, excessive salivation is caused by overactivity of the salivary glands, as well as if a person has a disturbed swallowing process.
If you eat a spicy dish during your lunch break, your body will begin to intensively secrete saliva. This is because the taste buds on the tongue help increase the volume of fluid produced. For a visual example, you can put something sharp on your tongue. After a few moments, you will be able to feel a rush of saliva into your mouth. Also, sour foods affect excessive salivation. Accordingly, you can reconsider your diet if you are concerned about excess salivary secretion. In addition, the above symptom may occur as a result of certain diseases and abnormalities, as well as due to the use of special medications.
Diagnostics
With the problem of drooling, patients turn to a dentist, or less often to a therapist. Given the variety of causes of pathology, the doctor is required to take a detailed medical history and clarify related complaints. The diagnostic search begins with an examination of the oral cavity to identify signs of inflammation or caries. To establish the causes of drooling, the following instrumental and laboratory diagnostic methods are used:
- Biochemical analysis of saliva.
The study evaluates the amount of fatty acid metabolites formed during the life of bacterial flora. Based on the results of the analysis, it is possible to determine the presence of dysbacteriosis and determine the level of damage to the digestive tract. - General clinical studies.
Patients with drooling undergo a general blood test, changes in which indicate the presence of an inflammatory or infectious process. To exclude helminthic infestations, a coprogram is prescribed, a fecal examination for helminth eggs. According to indications, a clinical urine test and studies according to Nechiporenko and Zimnitsky are performed. - Instrumental techniques.
If a patient suffering from drooling has complaints about the functioning of the digestive system, an ultrasound of the abdominal organs and plain radiography are necessary. To exclude neurological diseases, CT or MRI of the brain is recommended. Electroneuromyography is effective for assessing the functions of peripheral nerves.
Diseases that cause increased salivation
Experts note a number of diseases that cause our salivary glands to work hard. Among them: central and peripheral paralysis, gastroesophageal reflux disease, mental development disorders, abnormally large tongue, Parkinson's disease, pregnancy (severe toxicosis), poisoning, stroke, rabies.
In addition, there are a number of drugs that cause excess salivary fluid. These include: drugs against schizophrenia, antiepileptic drugs, as well as medications prescribed to patients undergoing radiotherapy. The common medical term for excess salivation is sialorrhea or hypersalivation.
Excessive salivation during pregnancy
During pregnancy, hormonal changes occur in the female body. The main reasons why an expectant mother’s salivation increases.
- Heartburn. When the acid-base balance in the stomach is disturbed, the body begins to produce a lot of saliva. This is a defensive reaction.
- Reaction to medications.
- Toxicosis. To stop gagging, the expectant mother tries to swallow saliva less often. Therefore, it may seem that there is more saliva in the mouth than usual.
A large amount of saliva does not threaten the fetus, however, if this is a consequence of any disease, then the pregnant woman should monitor her condition.
What complications are possible?
- Impaired taste perception of food.
- Dehydration of the body.
- Insomnia, disturbance of psycho-emotional state.
- Deterioration of the skin condition on the face and body.
- Infectious diseases.
Excess saliva, or how to prevent it
By and large, there are three types of therapy that are used to treat increased salivation. These include Botox injections, surgical treatment and medications that are available only by prescription. It all depends on the factors that caused the disease. It is clear that the simplest thing will be to prescribe certain medications. Typically, the above drugs will include scopolamine and glycopyrrolate. Side effects include increased heart rate, trouble urinating, drowsiness, and blurred vision.
For severe forms of drooling, specialists resort to Botox injections into the salivary glands (one or more). The treatment is considered safe, but its effect only lasts for several months. And only in very severe cases do doctors resort to surgery. During surgery, the salivary glands are removed or the direction of the excretory ducts is changed.
With the help of surgery, you can permanently get rid of increased salivation. Salivary glands – increased salivation and dry mouth
Hypersalivation, treatment
To successfully eliminate hypersalivation, treatment must begin with a search for the true cause of the pathology - only an accurate diagnosis will allow one to prescribe effective methods of therapy. In the case where high salivation is caused by diseases of the oral cavity, treatment by a dentist will be necessary: examination and sanitation of the oral cavity, anti-inflammatory therapy.
If the pathology is caused by disturbances in the functioning of other systems (digestive, nervous, endocrine), joint supervision of the dentist and related specialists - gastroenterologist, endocrinologist, neurologist will be required. In any case, even if the problem is caused by some kind of systemic failure in the body, successful therapy will require high-quality sanitation of the oral cavity with the elimination of all infectious and inflammatory foci.
In some cases, hypersalivation is treated with drugs that reduce salivation. You can take such drugs only on the recommendation and under the supervision of a doctor; moreover, you need to remember that sometimes they cause unwanted side reactions. In addition, the doctor may prescribe physiotherapeutic procedures, massage and facial gymnastics, rinsing - all these methods are usually used in combination. In particularly difficult situations, surgical intervention to remove large salivary glands is possible, but surgical treatment is used only as a last resort.
What to feed a child with nausea and vomiting?
Many parents do not know what their baby’s diet should be if he is constantly vomiting. With repeated vomiting (especially in case of poisoning, when it is accompanied by diarrhea), the baby loses a lot of fluid, which threatens dehydration. It is necessary to give small portions of water, dried fruit compote, cooled herbal teas or rosehip decoction. Under no circumstances should you use sugary water or carbonated drinks for drinking - this can dramatically worsen the condition. Also, you should not let your child drink a lot of liquid at a time - this can provoke a new attack of vomiting. Source: E.O. Komarovsky Handbook of sensible parents. Part 2. Emergency care. Eksmo-Press, 2011
In each case, the doctor gives individual recommendations on the child’s nutrition, but the general principle is this: the load on the gastrointestinal tract should be reduced as much as possible. It is necessary to remove smoked, over-salted, fatty foods from the diet. Porridge with water, jelly, homemade compotes and crackers, steamed cutlets and vegetables - all this belongs to a gentle diet and will help the baby recover faster.
Medical doctors have extensive experience in treating gastrointestinal diseases in children. Advanced examination methods and qualified doctors will help you quickly identify the causes of nausea in a child and begin effective treatment.
Sources:
- Lilenko S.V. Motion sickness in children and adolescents: pathogenesis, symptoms, prevention and treatment // Russian Pediatric Journal. 2016; 19 (1):49-54. DOI 10.18821/1560-9561-2016-19 (1)-49-54
- E.O. Komarovsky “Handbook of sensible parents. Part 2. Emergency care." Eksmo-Press, 2011
The information in this article is provided for reference purposes and does not replace advice from a qualified professional. Don't self-medicate! At the first signs of illness, you should consult a doctor.
Causes of nausea in a child
Based on their origin, the causes of nausea can be divided into several categories.
Nausea in a child due to “nerves”
The central nervous system is involved here. The condition occurs when:
- head injuries and concomitant concussions;
- hypertensive or hypotensive crisis (sharp increase or decrease in blood pressure). This phenomenon is not uncommon in children during adolescence, when the body experiences hormonal overload, and surges in blood pressure occur quite often. Vomiting may provide relief, but not for long;
- encephalitis (inflammation of the membranes of the brain);
- the presence of benign neoplasms in the brain (slowly progressing and not metastasizing);
- meningitis (inflammation of the brain);
- malignant tumors of the brain, cerebellum;
- "sickness" in transport. This condition is associated with weak functioning of the vestibular apparatus. It may disappear completely with age. If your child is prone to such conditions, you should not travel long distances, and you should always have antiemetics with you. The peculiarity of this type of nausea is its suddenness. Vomiting does not bring relief, after it the condition may even worsen. Source: Lilenko S.V. Motion sickness in children and adolescents: pathogenesis, symptoms, prevention and treatment // Russian Pediatric Journal. 2016; 19 (1):49-54. DOI 10.18821/1560-9561-2016-19 (1)-49-54
If a child experiences repeated nausea without fever (or with low temperature) and diarrhea or without vomiting, there can be a variety of reasons. Such conditions are reasons to immediately consult a doctor. With timely treatment, the prognosis is generally favorable.
"Toxic" nausea
It is associated with the presence in the body of toxins of various origins that circulate through the circulatory system:
- The most common cause of this ailment is poisoning from stale foods that contain E. coli. You can also be poisoned by various poisonous plants (mushrooms) or by exceeding the permissible dose of medication. Poisoning in a child, in addition to nausea, causes fever and abdominal pain, diluted stool; Source: E.O. Komarovsky Handbook of sensible parents. Part 2. Emergency care. Eksmo-Press, 2011
- renal failure. It can be caused by a number of diseases - from congenital insufficiency to acquired pathologies. If the kidneys do not perform their function properly, an excess amount of toxins appears in the body, causing permanent nausea;
- liver failure. The liver, like the kidneys, performs the function of removing toxins. Liver cell destruction (which can be acute or chronic) also causes occasional nausea in children;
- various types of benign and malignant tumors;
- thyrotoxicosis (associated with dysfunction of the thyroid gland) - poisoning of the body with hubbub.
Nausea caused by diseases of the gastrointestinal tract
- gastritis – inflammation of the mucous membranes of the stomach. Nausea appears after eating and may also be accompanied by a burning sensation and a feeling of heaviness in the stomach, heartburn;
- taking certain medications (for example, antibiotics). You should carefully study the side effects of the medicine, and if such symptoms appear, ask your doctor to prescribe another drug;
- duodenitis (inflammation of the duodenum);
- pancreatitis – inflammation of the pancreas. The child experiences nausea after eating. May be accompanied by bitterness in the mouth, a feeling of heaviness in the right hypochondrium, bloating;
- appendicitis. One of the signs of inflammation of the cecum, in addition to pain in the side, is periodic nausea. If you suspect appendicitis, you should immediately call an ambulance;
- peptic ulcer of the stomach or duodenum - the formation of wounds on the mucous membranes of the gastrointestinal tract;
- cholecystitis (inflammation of the gallbladder) and cholelithiasis. Accompanied by a feeling of bitterness in the mouth;
- tumors of the gastrointestinal tract;
- disruption of the gastrointestinal tract (natural movement of food and feces through the digestive system). It often occurs due to a foreign object swallowed by a child;
- congenital pathologies of the gastrointestinal tract.
If a child periodically experiences nausea, this is a serious reason to contact a pediatric gastroenterologist, who will prescribe tests. The sooner treatment is started, the more favorable the medical prognosis will be.
Symptoms of pharyngitis
The first signs of the disease may differ depending on the type of pharyngitis. They are both local and general in nature. But there are common signs that are characteristic of any type of pharyngitis: sore throat, bad breath, stuffy ears and difficulty swallowing. With an active inflammatory process, an increase in body temperature above 38° can be observed - this is how the body fights a foreign infection. General signs: sweating, poor appetite, weakness, dizziness, fatigue, fever, chills. Some complain of pain and noise in the ears, and discomfort when exposed to loud sounds.
- During acute catarrhal pharyngitis, swelling and redness of the mucous membranes of the larynx appears. Also, red follicles may form on the back wall of the throat, and clear and slightly cloudy mucus may accumulate. There is swelling and redness of the tongue.
- In the purulent form of acute pharyngitis, ulcers with an accumulation of purulent masses appear on the surface of the posterior pharyngeal wall.
Drooling (sialorrhea, hypersalivation, ptyalism) is characterized by an increase in the amount of saliva with its flow from the oral cavity through the border of the lips in such a volume that it negatively affects the social and domestic activities and daily life of the patient, leading to damage to the soft tissues of the oral cavity, lips and chin . Parkinson's disease (PD) is the most common cause of sialorrhea in adults. The incidence of this suffering in PD varies from 45 to 80% [1, 2]. Some researchers note a lower prevalence of sialorrhea - 10%. Initially, drooling only bothers you at night, but later, as the disease progresses, it also occurs during the day. Although the association of sialorrhea with PD has been known since the time of J. Parkinson's classic monograph, the pathophysiology of sialorrhea has not been sufficiently studied.
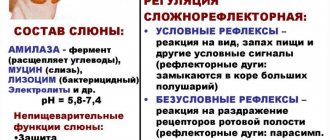
Functioning of the salivary glands under physiological conditions
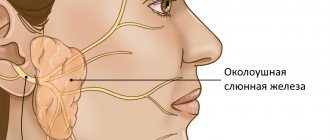
Depending on the size, small and large salivary glands are distinguished. The minor salivary glands are localized in the mucous membrane of the lips, cheeks, tongue, hard and soft palate. The large salivary glands are located outside the mouth. Three pairs of major salivary glands (parotid, submandibular, sublingual) produce and secrete saliva. Parotid glands ( glandula parotidea
) are located directly under the skin, in front and downward from the auricle, on the lower jaw, at the posterior edge of the masticatory muscle.
The external carotid artery and its branches pass through the parotid gland. Per day, the parotid glands secrete about 1/3 of the volume secreted by all salivary glands (approximately 0.2-0.7 liters of saliva).
Submandibular salivary gland ( glandula submandibularis
) is located superficially, under the cervical fascia and skin. Medially it borders with the styloglossus and hyoglossus muscles, above with the lower jaw, and below it emerges from under its lower edge. In front, the gland is in contact with the posterior edge of the mylohyoid muscle, and laterally it is adjacent to the facial artery and vein. The submandibular gland secretes saliva containing both mucous and serous (protein) secretions.
Sublingual gland ( glandula sublingualis
) is located immediately under the mucous membrane of the floor of the mouth, on both sides of the tongue, on the upper surface of the mylohyoid muscle. Laterally it comes into contact with the inner surface of the body of the lower jaw, medially with the genioglossus, geniohyoid, and hyoid-glossus muscles. The sublingual glands secrete saliva containing a serous (protein) secretion. It is richer in mucin than the saliva of the parotid and submandibular glands, has a pronounced alkaline reaction and high phosphatase activity [3].
The secretory activity of the salivary glands is regulated by the salivary zone of the cerebral cortex and the nuclei of the brain stem. This zone is excited by signals coming from taste buds. Next, the cortical zones interact with the upper (in the region of the parvocellular reticular nucleus) and lower (in the lateral part of the reticular formation) salivary centers of the brain stem.
The secretory activity of the salivary glands is provided by sympathetic and parasympathetic innervation. However, when eating and swallowing, the activity of parasympathetic innervation is mainly activated. Parasympathetic afferent pathways, receiving a signal from the receptors of the pharynx and esophagus, reach the salivary center located in the medulla oblongata through the system of the vagus nerve and visceral nerves [2–4].
Parasympathetic efferentation occurs through two pathways. The glossopharyngeal nerve innervates the auricular ganglia and subsequently the parotid gland via the auriculotemporal nerve. The facial nerve innervates the submandibular ganglia through the chorda tympani and then through the lingual nerve ensures the functioning of the submandibular and sublingual glands [5] .
The process of salivation is inextricably linked with swallowing. The act of swallowing consists of three phases: oral, pharyngeal and esophageal. The oral phase is voluntary, while the pharyngeal and esophageal phases are involuntary. The act of swallowing begins with the involvement of more than 30 different muscles of the oropharynx to form and move the bolus of food into the esophagus. Subsequently, the upper esophageal sphincter (EES) opens and the food bolus passes from the pharynx into the esophagus and then into the stomach [2, 6]. Central motor control of swallowing function is provided by the premotor cortex, primary motor cortex, basal ganglia, pedunculopontine nucleus, and cerebellum. Central neurons project to the stem swallowing centers, in particular the nuclei of the solitary tract (common to the facial, glossopharyngeal and vagus nerves, providing taste sensitivity). These centers further regulate the functions of structures involved in the swallowing process, such as the tongue, muscles of the larynx, pharynx and upper esophagus. At the same time, the muscles of the tongue are controlled by the nucleus of the hypoglossal nerve; the muscles of the larynx, pharynx and upper esophagus are controlled by n . a mbiguous
(common to the vagus and glossopharyngeal nerves) [4, 7]. In patients with PD, the oropharyngeal phase of swallowing is predominantly affected.
Function of the salivary glands in PD
Two causes of drooling in BP are actively debated. One of them is a violation of saliva production, and the other reason may be insufficient saliva utilization. Overproduction of saliva can certainly cause drooling. However, many studies have shown [8, 9] that patients with PD produce even less saliva than healthy people. The exact mechanisms causing the decrease in salivation remain unknown [10].
A decrease in salivary secretion in PD may reflect the involvement of the stem salivary nucleus and cranial autonomic ganglia. One possible explanation is a dopamine deficiency. Experimental studies in animal models have shown that dopamine modulates salivary secretion [11, 12]. Studies in rats have demonstrated that activation of central and peripheral dopamine receptors induces salivation [11]. It is known that damage to the striatum, globus pallidus and the descending pathway to the lateral part of the reticular formation of the midbrain can significantly reduce salivation [13]. Pathological studies have revealed the presence of Lewy bodies in patients with PD both in autonomic formations (in the superior cervical ganglion, sympathetic trunk of the cervix, peripheral vagus nerve) and in the submandibular gland [14]. Although Lewy bodies are found in peripheral ganglia, involvement of the cranial parasympathetic ganglia in the degeneration process has not been established. Dopamine has been confirmed to stimulate salivation, even with the administration of the peripheral D2 receptor blocker domperidone, which is indirect evidence of the involvement of higher levels of regulation in this system, including the basal ganglia and brainstem, which may be responsible for reducing salivation in these patients [15]. .
Studies assessing the intensity of production and rate of salivary excretion of the parotid glands using scintigraphy did not show a difference in saliva production, but the rate of saliva excretion to discrete stimuli was significantly higher in patients with PD compared to healthy controls [16, 17]. Thus, increased salivary flow is not a major contributor to the pathophysiology of drooling in BP. However, increasing the excretion rate partially increases sialorrhea.
In PD, the function of the blood-salivary barrier is disrupted, its permeability to calcium, magnesium and zinc increases and the concentration of copper in saliva decreases. Taking levodopa brings the permeability of the blood-salivar barrier closer to functional compliance with healthy ones [18]. Thus, dopamine regulation of not only the volume of saliva secreted, but also the ratio of its mucosal and serous components and elemental composition is not excluded.
Swallowing dysfunction may be one of the leading causes of drooling in patients with BP. It is known that the dorsal motor nucleus of the vagus nerve is affected already in the early stages of PD, although other central regulators of swallowing remain intact for a long time. At the same time, the pedunculopontine tegmental nucleus, which modulates the activity of the medulla oblongata nuclei, is also affected quite early in PD.
The nucleus ambiguus regulates the function of the striatal muscles of the pharynx and upper esophagus. The dorsal motor nucleus of the vagus nerve controls the intermuscular nerve plexuses of the smooth muscles of the esophagus. While the myenteric plexus and dorsal nucleus are affected in the early stages of PD, the pathology of the oral and pharyngeal stages in patients with PD at the onset of the disease is associated not with the involvement of the nucleus ambiguus, but with a violation of the supramedullary control of swallowing.
Oropharyngeal phase disruption found in PD may contribute to the accumulation of saliva in the oral cavity. Oropharyngeal dysphagia is thought to result from bradykinesia. Animal studies have shown that after injection of 6-hydroxydopamine (6-OHDA), the rate of tongue protrusion slows down in experimental rats, and the average duration of tongue pressure becomes significantly longer compared to the control group [19]. Another study [20] showed that the maximum tongue pressure in patients with severe stages of PD was weaker compared to patients with early or moderate stages, and the transit time of the bolus in the oropharynx was negatively correlated with the speed of tongue movement. Both studies reflect the fact that patients with PD have bradykinesia of the oropharyngeal phase of swallowing and impaired tongue muscle function.
Thus, dysfunction of tongue control contributes to dysphagia and may be a cause of drooling. A videofluorographic study in a model of parkinsonism in rats (after injection of 6-OHDA) showed a slower progression of the food bolus compared to the control group [21].
A study using barium in patients with drooling in PD demonstrated a direct correlation between the severity of dysphagia and the severity of sialorrhea [22]. Scintigraphy showed the presence of subclinical manifestations of dysphagia in all patients with sialorrhea. Patient complaints of drooling aggravated swallowing disorders [17]. Thus, oropharyngeal dysphagia may be a major pathophysiological factor in drooling in PD.
Another cause of drooling may be impaired motility of the upper esophagus. Data from manometric studies provided evidence of impaired EEC relaxation in patients with PD compared with controls.
Often, a manifestation of PD is a dystonic swallowing disorder [23]. In this case, dysfunction of the pharyngo-cricoid muscles leads to dysphagia. The pharyngo-cricoid muscles are the upper sphincters of the esophagus. Accordingly, impairment of their ability to adequately relax during swallowing can lead to impairment of the ability to swallow solid food. This condition is often called crico-pharyngeal achalasia and is characterized by insufficient relaxation of the upper esophageal sphincter in duration and severity.
However, this factor cannot be the only cause of dysphagia, and if the patient has sufficient pharyngeal propulsive force, swallowing will not be significantly affected [24, 25]. There is probably a combination of disturbances in the oropharyngeal and esophageal phases of swallowing.
Hypomimia, involuntary opening of the mouth, slouching or drooping head can also lead to inability to retain saliva in the mouth [26]. At the same time, there is no evidence that drug-induced dyskinesias can cause drooling. Thus, today three main mechanisms of sialorrhea in PD are considered: increased secretion of saliva, inability to retain saliva in the oral cavity (hypomimia, involuntary opening of the mouth, stooping or drooping head), deterioration of salivary clearance (lingual bradykinesia, oropharyngeal dysphagia, upper sphincter dysfunction esophagus).
Epidemiology and maladjustment
On average, 50% of patients with PD complain of drooling, subclinical sialorrhea is objectified (videofluoroscopy) in 90% [2, 7]. Drooling is present in 86% of patients with dysphagia and only 40% without it [27].
Patients suffering from excessive salivation experience difficulty articulating speech and swallowing, and have bad breath. Constant leakage of saliva from the oral cavity forces one to resort to the use of handkerchiefs or towels, leading to perioral cracking, irritation, and maceration of the skin. Wetness and soiling of clothes and bedding increases the burden on caregivers. Psychologically, excessive drooling can lead to decreased self-esteem and social isolation.
Treatment methods
Treatment of sialorrhea in PD includes methods aimed at reducing saliva production with the prescription of acetylcholine transport blockers, cholinesterase inhibitors; use of clozapine and quetiapine; improvement of motor symptoms of PD with dopaminergic agents and surgical neuromodulation. However, the effectiveness of these methods is only partial, and new pharmacological and non-pharmacological approaches to the treatment of sialorrhea are needed. For this purpose, various groups of drugs are being studied, including anticholinergic drugs, adrenergic receptor antagonists, and botulinum toxins (BTX).
Anticholinergic drugs.
For selective action, blockers of M3-cholinergic receptors, predominantly localized in the salivary glands, are required. This way you can avoid side effects such as confusion, hallucinations, constipation, urinary retention, and drowsiness. For this purpose, the following were studied: sublingual atropine [28], sublingual ipratropine bromide spray [29], oral glycopyrrolate [30], and oral tropical tropamide [31]. Current MDS guidelines for the use of anticholinergic drugs for the treatment of drooling in PD indicate that glycopyrrolate is effective, but proven efficacy lasts for 1 week and there is insufficient information on its tolerability. There is also insufficient information on the effectiveness and tolerability of ipratropine.
Adrenergic receptor agonists
may partially reduce sialorrhea. Clozapine, yohimbine, and α2-adrenergic receptor antagonists have been reported in the literature as having drooling as a side effect. Based on this, α-2-adrenergic receptor agonists should reduce salivation. Specifically, clonidine reduced sialorrhea in a small, randomized, double-blind, placebo-controlled trial of 32 patients [32]. Oral modafinil 100 mg daily also reduces drooling. However, modafinil is an α-1-adrenergic receptor agonist, and the reduction in sialorrhea is most likely due to a reduction in dysphagia rather than suppression of salivary production [32]. Thus, there are currently no recommendations for the use of α2-adrenergic receptor agonists in the treatment of hypersalivation, but clonidine and modafinil may be considered promising agents.
Botulinum therapy
The main mechanism of action of BTX is inhibition of acetylcholine release. Local injections into the salivary glands inhibit cholinergic parasympathetic and postganglionic sympathetic activity, causing a decrease in salivary secretion. Two serotypes of BTX are being studied to reduce sialorrhea: serotype A and serotype B. Two types of BTX type A, onabotulinumtoxin and abobotulinumtoxin, are used in the treatment of sialorrhea.
Studies have been conducted to study onabotulinumtoxin of various designs (observational, open, open case-control, randomized placebo-controlled) [33-38]. In all of these studies, injections were made into the parotid gland. One of them [37] included patients not only with PD, but also with multiple system atrophy and dementia with Lewy bodies. Two studies [33, 36] used ultrasound guidance. One study [33] showed no difference in the effectiveness of injections with and without ultrasound guidance. The therapeutic effect was assessed after 1–16 weeks. BTX was administered in doses of 5 to 50 units into the parotid gland and 5 units into the submandibular gland with a significant reduction in salivation and a duration of effect of up to 4 months.
Abobotulinum toxin (Dysport) was injected into the parotid gland in all studies. In some of them [39], BTX was additionally injected into the submandibular salivary gland. Most studies did not use additional injection control methods. Only two of them [39, 40] used ultrasound guidance. The duration of outcome assessment ranged from 1 to 4 weeks. All studies demonstrated the effectiveness of abobotulinumtoxin in doses of 75-146.2 units when injected into each parotid gland and 78.7 units into each submandibular salivary gland. Salivation was significantly reduced in patients not only with PD, but also with multiple system atrophy, corticobasal degeneration, and amyotrophic lateral sclerosis [41]. Both according to objective assessment methods and according to the subjective feelings of patients, the therapeutic effect persisted for 1-4 months. Additionally, it was found that there are no significant differences in therapeutic effects between injections of the drug into the parotid or submandibular glands [26].
BTX type B (rimabotulinumtoxin, not registered in Russia) was also injected mainly into the parotid salivary gland [42–47], two studies used ultrasound guidance [31, 45]. All studies demonstrated the effectiveness of BTX type B in doses of 500-2000 and 250 units when injected into the parotid and submandibular glands, respectively, with an average duration of effect of 4.8 months.
The objective of one of the studies was to compare BTX types B and A (randomized, placebo-controlled, crossover, ultrasound-guided) [48]. Either 100 units of abobotulinumtoxin or 1000 units of rimabotulinumtoxin were injected into the parotid gland; either 25 units of abobotulinumtoxin or 250 units of rimabotulinumtoxin were injected into the submandibular gland. When assessing salivation using the DSFS (Drooling Severity Scale and Frequency Scale) and DRS (Drooling Rating Scale) methods 1 month after the injection, the result was better in the group that received BTX type B, but after 2 months the results were equal.
According to MDS recommendations, BTX are effective in the symptomatic treatment of sialorrhea in PD [49]. The therapeutic effect begins 1 week after the injection and lasts 3-5 months. Ultrasound-guided injections may be more accurate. There were no differences in the effectiveness of BTX types A and B. Typical side effects such as dry mouth are mild.
Pharyngeal-cricoid dysphagia can also be successfully compensated with BTX injections. Several injection techniques have been described, including both percutaneous and endoscopic techniques [50, 51]. Administration of BTX type A 30 IU for dysphagia into the pharyngo-cricoid muscle under the control of electromyography and esophagoscopy leads to a decrease in swallowing disorders after 48 hours: swallowing function improves, hyperactivity of the pharyngo-cricoid muscle decreases according to electromyography [52]. Dysphagia usually returns 22 weeks after injection. During these weeks of swallowing improvement, patients regain lost body weight [51, 53]. This fact is important in improving the quality of life of patients.
Non-pharmacological treatments
Various non-pharmacological treatments are offered, such as chewing gum, behavior modification, radiation therapy, and surgical methods. However, only 2 studies on this topic have been published. L. Marks et al. [54] conducted a randomized placebo-controlled trial in 6 patients with PD. Patients were required to voluntarily swallow each time they heard a sound. This modified behavior resulted in a significant reduction in sialorrhea as assessed by DRS. At the same time, the results that reached their maximum 1 month after training turned out to be minimal after 3 months. The authors concluded that patient motivation and voluntary control of swallowing should be considered and used in the treatment of patients with sialorrhea.
Another study used bilateral 12 Gy radiotherapy to the parotid and superior submandibular glands [5]. Hypersalivation decreased significantly after 1 month after radiotherapy, and the effect persisted for up to 1 year. The most common adverse events were decreased taste and dry mouth. However, 75% of adverse events were transient.
We have not found any studies in the literature regarding the effect of surgical neuromodulation. It is possible that in some cases, when chronic stimulation of the basal ganglia causes deterioration in swallowing, drooling may increase [56]. A recent study [57] showed an adverse effect of bilateral stimulation of the subthalamic nucleus.
The bottom line is that there are no current recommendations for the use of non-pharmacological methods in the treatment of sialorrhea in BP. However, behavior modification and, in refractory cases, radiotherapy can be considered as additional components of the overall treatment package.
In conclusion, drooling has negative consequences on the lives of both patients with PD and their caregivers. While the leading role in sialorrhea is probably not overproduction of saliva, but swallowing disorders, most treatment methods are aimed at reducing secretion. Currently, injections of botulinum toxins into the major salivary glands are the most effective treatment. The pathophysiology of ptyalism, standardization of diagnostic criteria, methods for assessing severity, and development of treatment strategies for sialorrhea in PD require further study.