What is this disease?
Herpetic stomatitis is a pathological process that develops in the mucous membrane lining the oral cavity. The causative agent of this disease is herpes simplex virus type 1. In children under the age of five, this virus is detected in 60% of all cases. By adolescence, it is detected in the vast majority of people. Herpes stomatitis in children develops during the baby’s first contact with the virus. This occurs most often before the age of three.
The high incidence is explained by:
- low level of production of own antibodies;
- immaturity of cellular immunity;
- the fact that the baby does not receive antibodies from mother's milk;
- high reactivity of the child's body.
If the baby is bottle-fed, he may get sick in the first months of life. Viral infection often goes into a latent state. It persists in the nerve ganglia.
Causes
The cause of the development of the pathology is the herpes simplex virus type 1. It belongs to DNA viruses belonging to the Herpesviridae viral family. The pathogen multiplies rapidly in the epithelial cells of the oral mucosa. Then it enters nearby lymph nodes (submandibular) and continues to reproduce in them. Then it enters the blood and migrates to the parenchymal organs (spleen, liver, kidneys). There it multiplies and enters the bloodstream again. As a result, it again appears in large quantities in the epithelial cells of the skin and mucous membranes. They are massively defeated. It is localized in the oropharynx, oral cavity, nose, lips, and nearby skin. Stomatitis and herpes of the skin and mucous membranes develop when the infection generalizes simultaneously.
Children become infected with it as follows:
- through contact and everyday life (using shared utensils, toys, through kissing);
- airborne (coughing, sneezing);
- from a sick mother to the fetus through the placenta or during childbirth.
A baby can become infected from sick adults, children, and carriers.
The following factors contribute to the development of the disease:
- previously suffered inflammatory processes;
- previous antibiotic therapy;
- deficiency of microelements and vitamins in the body;
- mechanical damage to the skin and mucous membranes;
- insufficient fluid intake;
- poor oral hygiene.
In children, the virus is especially easily transmitted through contact. The infectious process quickly spreads to healthy areas.
What are the symptoms in babies?
Symptoms may range from mild to severe. This depends on the level of bilirubin in the blood and the duration of the disease. The causes and consequences of jaundice in newborns can vary, but there is one common characteristic - jaundice of the skin and sclera. It is worth noting that the eyes show symptoms faster. The baby may experience increased drowsiness with a decreased sucking reflex. Convulsions may occur. Without treatment, advanced jaundice can cause deafness, mental retardation and paralysis.
Does your newborn have symptoms of jaundice?
Only a doctor can accurately diagnose the disease. Don't delay your consultation - call
Classification
According to the flow, acute, chronic, and wave-like variants of the pathology are distinguished. The following degrees of severity of the pathological process are distinguished:
- Mild - it is typically characterized by a slight increase in body temperature, moderate inflammation of the mucous membrane in the mouth, and enlargement of regional lymph nodes. Rashes form on the mucous membrane and skin.
- Medium – high temperature rises. Severe weakness and sudden deterioration in health. The baby begins to vomit and the pain in the mouth increases. Significant rashes appear in the mouth and the skin around it.
- Severe - a severe headache is added to the pathological process. High temperature rises, severe muscle pain. Not only regional but also distant lymph nodes enlarge. The rashes are located not only in the oral cavity, but on the skin next to it. They appear on the mucous membrane of the eye, on the eyelids, and on other parts of the face.
The severity of the pathology depends on the viral load (the amount of virus in the body) and the general reactivity of the body.
Snot in a baby
Very often situations arise when a child has snot, but there are no signs of a cold. This type of runny nose is physiological in nature and can continue until the newborn is 2 months old. Factors that cause snot in newborns:
- Infection. Most often, colds occur when a viral infection enters the body, transmitted by airborne droplets. ARVI in infants progresses rapidly and manifests itself with pronounced symptoms.
- Allergy. Snot in children can also be allergic in nature. They occur when nasal inhalation of allergens such as dust, pollen of flowering plants, fluff, and wool. In such situations, the breathing process becomes more difficult, the baby begins to sneeze, and watery snot comes out of the nose. Vascular response to external stimuli. Very often, snot in newborns occurs when the nasopharyngeal vessels are highly sensitive to environmental factors. This process usually manifests itself with bouts of sneezing, alternating sinus congestion, and copious nasal discharge.
- Enlarged adenoids. A peculiarity of the physiology of the children's respiratory system is that at birth, adenoids begin to grow rapidly in children. They sometimes provoke the formation of snot, which has a greenish color. In such cases, it is necessary for the baby to drip a 1% solution of collargol into the nose.
Treatment of rhinitis in newborns is difficult, due to the narrow nasal passages. The course of rhinitis in newborns has its own characteristics, which is explained by the physiological and anatomical characteristics of the infant. The complexity of the course of the disease lies in the fact that infants cannot independently free their noses from accumulated mucus, and also do not know how to breathe through their mouths, which is especially dangerous during sleep and breastfeeding.
Many parents don’t know what to do when their newborn’s snot bothers their baby day and night. You can’t start drug treatment for your baby’s rhinitis on your own; therapy can only be prescribed by a specialist.
How to treat a runny nose in a newborn depends on the factors that caused this condition of the child’s nasal mucosa. Even before visiting a specialist’s office, parents can take steps to alleviate their baby’s condition. First of all, if a baby has a severe runny nose that makes nasal breathing difficult, it is necessary to clear the nasal passages of pathological secretions. Solutions based on sea water or regular saline are well suited for this procedure.
Humidifying the air should be another action for parents who don't know what to do when their baby has a runny nose. A well-ventilated room with moist air promotes faster recovery of the nasal mucosa. You can increase the humidity in a dry room by using a humidifier. The optimal air humidity in the room where the sick child is is 50% at a temperature of 20-21ºС.
Treatment of clear snot in a child should be carried out only as prescribed by a doctor, since such a symptom may indicate several diseases. Regardless of the cause of rhinitis, parents should regularly clean the baby’s nose, thereby improving nasal breathing. To do this, you can use a special device for suctioning mucus - a nasal aspirator. If the clear mucus in the nose is so thick that it is difficult to remove it from the nasal cavity, the mucus must first be thinned. Solutions based on sea water, as well as decoctions of herbs such as chamomile, are well suited for this. You need to drop a few drops into each nasal passage of the child, and then use an aspirator. It is important to adhere not to symptomatic treatment, but to take actions aimed at eliminating the cause of the disease. Parents should promptly contact specialists who will tell you how to treat clear snot in a child, having previously established an accurate diagnosis.
Pharynx
In children, near the median septum of the retropharyngeal cellular space, there are lymph nodes into which lymphatic vessels flow from the palatine tonsils, posterior parts of the nasal and oral cavities. With age, these nodes atrophy; in children they can fester, forming a retropharyngeal abscess.
Adenoids are common in children.
Larynx
In newborns and young people, the larynx is located slightly higher than in adults (in adults, the upper edge of the larynx is at the border of the IV and V cervical vertebrae).
In children, the Adam's apple is soft and not palpable.
In children, the subglottic cavity has a well-developed loose submucosal layer. Its inflammatory swelling is called false croup.
Outer ear
In a newborn and infant in the first 6 months of life, the entrance to the external auditory canal looks like a gap due to the fact that the upper wall is almost closely adjacent to the lower one.
In newborns, the temporal bone is not yet fully developed, so they do not have the bony part of the ear canal, there is only a bone ring to which the eardrum is attached. The bony part of the auditory canal is formed by the age of 4, and up to 12-15 years the diameter of the lumen, shape and size of the external auditory canal change.
Eardrum
In children, the eardrum has an almost round shape and is much thicker than in adults (0.1 mm), due to the inner and outer layers. Therefore, with acute otitis media in children, perforation of the tympanic membrane may not be observed.
Middle ear
The auditory (Eustachian) tube in children is wider and shorter than in adults.
Mastoid
In a newborn, the mastoid part of the middle ear looks like a small elevation behind the superoposterior edge of the tympanic ring, containing only one cavity - the antrum. The formation of the mastoid process ends by the beginning of the 7th year of the child’s life.
Clinical manifestations
Stomatitis in children is characterized by a gradual onset of the disease. Clinical signs of the disease do not appear immediately after infection. The incubation period is typical for this pathology; it lasts from two days to three weeks.
Symptoms of herpetic stomatitis in children appear starting from the prodromal period.
Each period has its own clinic:
- Latent – lasts up to two weeks. The child's sleep is disturbed and he refuses to eat. The baby becomes restless and whiny. He has increased salivation, possible nausea and vomiting. The lymph nodes are enlarged and painful on palpation.
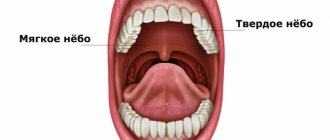
- The height of the disease - at this time rashes appear on the skin and mucous membranes. They are located on the soft, hard palate, gums, cheeks, lips and tongue. They are group or single, up to three millimeters in size. They are thin-walled bubbles filled with a clear liquid. Their formation lasts up to four days. The vesicles quickly open, then erosions and painful aphthae form. They are shallow ulcers covered with a white coating. The mucous membrane in the mouth is swollen and bleeding. The child develops a high temperature of up to 40 degrees. A runny nose, cough, and conjunctivitis occur.
- Fading - aphthae, erosions gradually heal and epithelialize. These formations heal without scarring. Often there is a wavy course of the disease. The periods of appearance of rashes alternate with rises in temperature.
The illness usually lasts up to two weeks. In children under one year of age, generalization of the process is possible. The development of sepsis, damage to all internal organs and meninges is likely.
Normalization of nasal breathing function in infants. New approaches
Impaired breathing through the nose can cause a number of disorders in children in the first months of life. In infants, the act of sucking and swallowing is disrupted, the baby begins to worry, refuses to eat, and sometimes gains weight more slowly. Lack of nasal breathing can even lead to increased intracranial pressure and dysfunction of the central nervous system. At the same time, the child becomes restless. Some children have sleep disturbances. Severe and prolonged difficulty in nasal breathing leads to hypoxia, which slows down development. Children with impaired nasal breathing begin to breathe through their mouths, and cold air entering the respiratory tract easily leads to colds; such children get sick more often.
Thus, the state of breathing through the nose should be monitored starting from the birth of the child. It is necessary to care for the baby’s nasal cavity daily - carefully, using special cotton swabs or turundas, remove crusts and thick mucus with rotational movements, after dropping 1-2 drops of sterile petroleum jelly or vegetable oil or isotonic solutions that help thin the mucus and facilitate its removal from the nose, enhancing resistance of the nasal mucosa to pathogenic bacteria and viruses, for example, Otrivin Baby drops for irrigation - a sterile isotonic solution of sodium chloride 0.74%, the pH level of which is close to the natural secretory fluid of the nasal mucosa. Otrivin Baby is used intranasally, a few drops from a dropper bottle 2-4 times in each nasal passage daily.
If a child has a large amount of mucus accumulated in the nose, which happens after heavy regurgitation or with a runny nose, you can use a special mucus pump or a small enema bottle and carefully suck out the contents of the nasal cavity. It seems convenient to use an Otrivin Baby aspirator, specially designed so that air cannot penetrate into the nasal passages and mucus does not get back into the nose. Replaceable disposable aspirator tips will help avoid re-infection. In addition, it is necessary to remember the need for regular examination not only by a pediatrician, but also by a pediatric otolaryngologist. Specifically for children, since the upper respiratory tract of children, as well as the child’s body as a whole, has a number of anatomical and physiological characteristics, and even minor inflammation of the nasal mucosa causes swelling in infants and, as a result, difficulty breathing through the nose.
The nasal cavity (cavum nasii) (Fig. 1) is located between the oral cavity and the anterior cranial fossa, paired maxillary and paired ethmoid bones. The nasal septum divides it sagittally into two halves, opening anteriorly with the nostrils and posteriorly, into the nasopharynx, with the choanae. Both halves of the nasal cavity are surrounded by paranasal sinuses: the maxillary, ethmoidal labyrinth, frontal and sphenoid, each of which communicates with the nasal cavity by an anastomosis. The nasal cavity has four walls: inferior, superior, medial and lateral.
The lower wall (bottom of the nasal cavity) is formed by two palatine processes of the upper jaw and, in a small area posteriorly, by two horizontal plates of the palatine bone (hard palate), connected along the midline by a suture. Congenital violations of this suture lead to various defects (for example, non-fusion of the hard palate). In front and in the middle in the bottom of the nasal cavity there is a nasopalatine canal (canalis incisivus), through which the nerve and artery of the same name pass into the oral cavity, anastomosing in the canal with the great palatine artery. In newborns, the bottom of the nasal cavity comes into contact with the tooth germs, which are located in the body of the upper jaw.
The upper wall (roof) of the nasal cavity in front is formed by the nasal bones, in the middle sections - by the cribriform plate (lamina cribrosa) and cells of the ethmoid bone (the largest part of the roof), the posterior sections are formed by the anterior wall of the sphenoid sinus. The filaments of the olfactory nerve pass through the openings of the cribriform plate. It should be remembered that in a newborn, lamina cribrosa is a fibrous formation that ossifies only by the age of three.
The medial wall, or nasal septum (septum nasi), consists of one anterior cartilaginous and posterior bone sections. The bony section is formed by the perpendicular plate (lamina perpendicularis) of the ethmoid bone and the vomer (vomer), the cartilaginous section is formed by quadrangular cartilage, the upper edge of which forms the anterior part of the dorsum of the nose. In the vestibule of the nose, anteriorly and downward from the anterior edge of the quadrangular cartilage, there is a skin-membranous movable part of the nasal septum (septum mobile) visible from the outside. In a newborn, the perpendicular plate of the ethmoid bone is represented by a membranous formation, the ossification of which ends only by the age of six. In a newborn, the height of the vomer is less than the width of the choana, so it appears as a transverse slit, and only by the age of 14 the height of the vomer becomes greater than the width of the choana, and it takes the form of an oval, elongated upward.
In the formation of the lateral (outer) wall of the nasal cavity, the medial wall and frontal process of the maxilla, the lacrimal and nasal bones, the medial surface of the ethmoid bone, and in the posterior part, forming the edges of the choana, the perpendicular process of the palatine bone and the pterygopalatine processes take part in the anterior and middle parts. sphenoid bone. On the outer (lateral) wall there are three nasal conchae (conchae nasales): lower (concha inferior), middle (concha media) and upper (concha superior). In a newborn, the inferior concha descends to the bottom of the nose, and there is a relative narrowness of all nasal passages.
On the side wall of the lower nasal meatus, at a distance of 1 cm in children and 1.5 cm in adults from the anterior end of the concha, there is an outlet of the nasolacrimal canal. This hole forms after birth; if its opening is delayed, the outflow of tear fluid is disrupted, which leads to cystic expansion of the canal and narrowing of the nasal passages. The posterior ends of the lower conchae come close to the pharyngeal mouths of the auditory (Eustachian) tubes on the lateral walls of the pharynx, as a result of which, with hypertrophy of the conchae, the function of the auditory tubes may be impaired and their disease may develop.
The mucous membrane of the nasal cavity (Fig. 2) covers all its walls in a continuous layer and continues into the paranasal sinuses, pharynx and middle ear. The anterior section of the nasal cavity is distinguished - the vestibule (vestibulum nasi) and the nasal cavity itself (cavum nasi), which in turn is divided into respiratory and olfactory. The respiratory region of the nasal cavity (regio respiratoria) occupies the space from the bottom of the nose upward to the level of the lower edge of the middle concha. In this area, the mucous membrane is covered with multirow columnar ciliated epithelium.
Under the epithelium is the actual tissue of the mucous membrane (tunica propria), consisting of connective tissue collagen and elastic fibers. There are a large number of goblet cells that secrete mucus, and tubular-alveolar branched glands that produce serous or serous-mucosal secretion, which exits through the excretory ducts to the surface of the mucous membrane. Somewhat below these cells on the basement membrane are located basal cells, which are the basis for the regeneration of the epithelium after its physiological and pathological desquamation.
The mucous membrane throughout is tightly fused with the perichondrium or periosteum, which forms a single whole with it. In the area of predominantly the medial and lower parts of the inferior concha, the free edge of the middle concha and their posterior ends, the mucous membrane is thickened due to the presence of cavernous tissue, consisting of dilated venous vessels, the walls of which are richly supplied with smooth muscles and connective tissue fibers.
Atmospheric air passing through the nose is warmed and moistened. In addition, the nose is a kind of filter that purifies the inhaled air. 0.5–1 liter of mucus per day is secreted into the nasal cavity, which moves in the posterior two-thirds of the nasal cavity at a speed of 8–10 mm/min, and in the anterior third at 1–2 mm/min. Every 10 minutes a new layer of mucus passes through, which contains bactericidal substances and secretory IgA.
In the neonatal period, as well as in infants, frequent regurgitation contributes to irritation of the mucous membrane of the nose and nasopharynx with gastric contents and inflammation - rhinitis, which is manifested by prolonged difficulty in nasal breathing. The first 3–5 months of life, which is the period of “physiological humoral immunodeficiency” of a person, pass “under the cover” of passively transmitted maternal antibodies against most respiratory viruses. The only exception is respiratory syncytial infection, in relation to which the intensity of passive immunity is insufficient, especially in premature newborns [1].
In children suffering from rhinitis, before breastfeeding, it is necessary to suck out the mucus from each half of the nose and 5 minutes before feeding, drip vasoconstrictor drops for infants into both sides of the nose [2, 4], for example, Nazivin 0.01%, for children under 1 month - 1 drop 2-3 times a day for 3-5 days, for children from 1 month to 1 year - 1-2 drops 2-3 times a day for 3-5 days; Otrivin “Moisturizing formula” (sorbitol and methylhydroxypropylcellulose included in the drug have a moisturizing effect) drops 0.05%, for children from 1 month to 6 years - 1-2 drops 2-3 times a day in each half of the nose [2 ], can be used for up to 10 days.
In children with a burdened allergic history, suffering from rhinitis, accompanied by nasal congestion, itching, sneezing, rhinorrhea, the use of the combined drug Vibrocil, which has not only a vasoconstrictor and antihistamine, but also an additional moisturizing effect, is justified. The drug does not disrupt the functioning of the ciliated epithelium, does not cause ischemia of the nasopharyngeal mucosa, has a natural pH level, which meets the basic requirements of physiological treatment of the nasal mucosa and allows long-term (up to two weeks) use of the drug. Vibrocil nasal drops are prescribed to children under 1 year of age, 1 drop in each half of the nose 3-4 times a day [2].
In the second and third stages of the disease, 2–3% solutions of Protargol or Collargol (depending on age), which have astringent and disinfectant properties, are used. In childhood, the inflammatory process in the mucous membrane of the nasal cavity more often than in adults spreads to the nasopharynx (adenoiditis), auditory tube (in children it is short and wide), larynx, trachea, bronchi, and lungs.
Inflammatory diseases of the paranasal sinuses are also not uncommon in children under one year of age. At this age, the cells of the ethmoidal labyrinth are already developed, which are present even in premature babies. Purulent ethmoiditis in an infant can occur as a result of infectious diseases of the mother, as well as after acute respiratory viral infection. Ethmoiditis often leads to osteomyelitis of the upper jaw, sepsis, and orbital phlegmon. Swelling of the nasal mucosa leads to impaired drainage of the paranasal sinuses and middle ear, which creates favorable conditions for the activation of opportunistic flora and contributes to the development of bacterial complications. In such cases, it is advisable to prescribe drugs consisting of several components that have an antibacterial and anti-inflammatory effect [2].
A rare pathology of the newborn period, which also leads to impaired nasal breathing, is a cerebral hernia that extends from the cranial cavity into the nasal cavity and nasopharynx. There are cases when a cerebral hernia was mistaken for adenoids or nasal polyps and the patient died when trying to remove them [2]. Adenoid vegetations (enlarged nasopharyngeal tonsil) disrupt normal nasal breathing, and also, being a receptor field, can cause allergization of the body. In addition, adenoids contribute to the formation of malocclusion.
Choanal atresia also leads to disruption and sometimes complete impossibility of nasal breathing. In the case of bilateral complete fusion of the choanae, the diagnosis is established on the first day of the child’s life - the baby is in serious condition, does not breathe through his nose at all, and cannot eat, since asphyxia occurs during feeding. This condition requires urgent surgical intervention. Unilateral atresia is more severe: the child is bothered by difficulty in nasal breathing through one or both halves of the nose, fatigue when feeding, the appearance of nasal discharge, and snoring. Sometimes such children are diagnosed only when they enter school. For diagnosis, probing and contrast radiography are used; such a patient must undergo an endoscopic examination of the nasal cavity and nasopharynx.
Thus, a seemingly banal difficulty in nasal breathing in infants should be the subject of increased attention of parents and patronizing physicians, as well as a reason for contacting otorhinolaryngologists and allergists.
Literature
- Samsygina G. A., Bogomilsky M. R. Respiratory tract infections in young children. M.: Miklos. 268 p.
- Kryukov A.I., Arkhangelskaya I.I. Acute rhinitis in children // Consilium medicum, 2004, vol. 6, no. 3.
- Hochban W., Althoff H., Ziegler A. Nasal decongestion with imidazoline derivatives: acoustic rhinomanometry measurements // Eur. Journal of clinical pharmacology, 1999; 55: 7–12.
- Karpova E. P. Acute rhinitis in children // RMJ, November 3, 2006, volume 14, number 22, pp. 1637–1641.
O. V. Zaitseva , Candidate of Medical Sciences
Federal State Institution NCC of Otorhinolaryngology FMBA of Russia, State Institution MONIKI named after. M. F. Vladimirsky , Moscow
Contact information about the author for correspondence
Diagnostics
A patient suspected of having this disease is examined by a dentist. He asks the child’s parents about how the disease progressed. The diagnosis is established on the basis of the characteristic clinical picture of stomatitis, revealed during examination, anamnesis and characteristic complaints. Upon examination, typical mucosal lesions are revealed.
To confirm the diagnosis, laboratory testing of scrapings of the oral mucosa, the contents of ulcers, the patient’s saliva and blood is used.
The following are used for research:
- cytopolymerase chain reaction;
- immunofluorescence method;
- serological blood tests (RSC, ELISA, immunoglobulin M test);
- HSV test for the detection of immunodot G-specific glycoprotein.
These methods are used only for severe infections, as they are quite expensive.
Treatment
Treatment of herpetic stomatitis in children with mild and moderate forms is carried out on an outpatient basis. In severe cases and the development of complications, the baby is hospitalized. Treatment is carried out under the supervision of a pediatric dentist or periodontist.
Children are prescribed bed rest and a diet with pureed, non-irritating food. He is given separate hygiene items and dishes. Plenty of warm fluids are recommended.
The following drugs are prescribed:
- Non-steroidal anti-inflammatory drugs (Nise, Paracetamol, Nurofen) are used to relieve temperature and inflammatory reactions.
- Antihistamines (Clemastine, Loratadine) are used to relieve swelling of the mucous membranes.
- Antiviral drugs (Famciclovir, Acyclovir, Zovirax) are used at the beginning of treatment or in severe cases.
- Immunomodulators (Lysozyme, Gamma globulin, Thymogen) are used to enhance immunity.
During treatment, vitamin-mineral complexes and fish oil are used in monthly courses.
Local drugs that act directly on the mucous membrane are widely used.
For local treatment of herpetic stomatitis the following are used:
- antiseptics (Hexoral, Miramistin) - they are used to rinse the mouth every four hours for two weeks;
- ointments and gels with anesthetics (Kamistad, Lidochlor gel) are used for pain relief, they are lubricated with mucous membranes three times a day for up to two weeks;
- antiviral agents (Ganciclovir, Acicovir) - destroy the viral cell, gums are treated with these ointments five times a day, two weeks;
- proteolytic enzymes (Trepsin, Chymotrypsin) are used to cleanse the necrotic surfaces of ulcers; they are washed with these solutions twice a day.
- rinsing with decoctions of medicinal herbs (calendula, chamomile, sage) is carried out after each meal for up to two weeks;
- epithelializing ointments (Solcoseryl, Methyluracil) are used to enhance the healing of erosions and ulcers, used in the recovery stage, used up to four times a day for ten days.
Physiotherapy is applied locally. Irradiation of affected mucous membranes with ultraviolet and infrared rays is used.
Treatment of white plaque on the palate of a child
The white spots will disappear if the cause of the problem is eliminated. If you regurgitate frequently, for example, you should change your feeding method and sterilize your utensils. A small area of fungal infection is treated with topical preparations. Severe forms of the disease are treated medicinally using complex drugs. Fungal diseases are dealt with:
- Clotrimazole;
- Candide;
- Pimafucin;
- Fluconazole;
- Diflucan;
A sterile gauze ball is moistened with the solution. They gently wipe the oral cavity several times a day. The duration of therapy depends on the complexity of the situation. Treatment usually lasts 7-10 days. Irrigation or lubrication is also prescribed. To boost the body’s defenses, doctors recommend vitamin complexes and probiotics for children. This will restore the natural microflora in the intestines.
Prevention
Preventive measures are aimed at preventing infection. This presents certain difficulties, since the vast majority of the population is infected with it. It is better if the child gets sick from it at an older age.
For this it is recommended:
- avoid contact with infected people;
- will provide personal utensils and personal hygiene products for the child;
- Kissing people with herpetic rashes is prohibited;
- strengthening the baby's immune system.
It is recommended that the child be provided with adequate nutrition and regularly given vitamin and mineral complexes.