Doctors Cost
Price list Doctors clinic
The feeling of numbness in the limbs is called paresthesia in medicine (from the Greek words “πᾰρά” - “outside, around, past” and “aisthesis” - “sensation”). This is the loss of normal tissue sensitivity due to impaired transmission of nerve impulses. It seems to a person that he is being touched through a layer of cotton wool.
Occurs at any age, often accompanied by tingling and goosebumps. It may be a physiological condition associated with prolonged compression of a nerve or blood vessels while in an uncomfortable position. When changing position, sensitivity is quickly restored. If the sensation is repeated, is not associated with an uncomfortable position, and lasts a long time, it requires diagnosis, as it may be a symptom of a dangerous disease.
Reasons for development
Various factors lead to impaired sensitivity, which can be divided into several large groups.
Table 1. Numbness of the extremities of the arms and legs: causes
| Cause | Examples of diseases, conditions |
| Squeezing blood vessels and nerve endings. | Intervertebral hernia, osteochondrosis, spondylosis, neoplasms. |
| Narrowing, blockage, deformation of veins. | Thrombophlebitis, varicose veins. |
| Cardiovascular diseases. | Cardiac ischemia. |
| Pathology of the nervous system. | Polyneuropathy, neuritis, radiculoneuritis, stroke. |
| Damage to blood vessels and nerves. | Injuries, postoperative complications. |
All paresthesias are fundamentally divided into two types.
- Transient. Caused by temporary compression of the neurovascular bundle – ischemia.
- Permanent. Occurs when there is anatomical damage to blood vessels or nerves.
If a person periodically experiences transient numbness, you should consult a neurologist for a thorough examination. This will help prevent life-threatening diseases: stroke, heart attack.
If an unpleasant sensation occurs and does not go away, you should also consult a doctor. Such problems do not disappear on their own. Without treatment, they can lead to disability.
1.General information
The term "paresthesia" in the broad sense of the word means "false tactile sensations." These are the same skin deceptions that we usually describe as goosebumps, tingling, electrical discharges, coldness, heat, causeless tickling in the absence of visible irritants, numbness, etc. It would seem that what could be simpler? However, the phenomenon of paresthesia is studied within the framework of more than serious disciplines: neurology, psychiatry, vertebrology, neurophysiology, psychology...
When it comes to the human body, and especially its neurophysiological organization, technical analogies do not always work. However, in this case, such an analogy is quite appropriate and accurate. The central nervous system exercises control and control through complex electrochemical reactions in the conductive nerves; from this point of view, paresthesia is a breakdown of insulation (as an electrical engineer would say, “to ground”), as a result of which the brain receives a false signal about skin irritation. In essence, such a violation of sensitivity is not a disease, but a symptom that is not causeless. The mechanisms of its occurrence are very diverse, but it is always based on either disturbances in nerve conduction or a malfunction in the “control panel” (when the brain itself begins to produce false sensations). In the International Classification of Diseases ICD-10, however, a separate nosological code is allocated for the designation of cutaneous paresthesia under the heading “skin sensitivity disorders.”
There are no statistical data on the incidence of paresthesia, and it is difficult to imagine collecting this kind of information, given the huge number of possible options and causes. Let us only note that most sources traditionally (and not unreasonably) classify paresthesia primarily as a neurological disorder, and interpret it precisely in this aspect.
A must read! Help with treatment and hospitalization!
Constant numbness in the extremities of the body
Carpal tunnel syndrome
The nerve fiber, located in a tight space limited by muscles and bones, is compressed by swollen tissues. Carpal tunnel syndrome is a common problem for modern people in certain professions: programmers, guitarists, artists, drummers - everyone whose work involves prolonged, monotonous stress on the hands. It manifests itself as paresthesia of the hand, pain, burning, sensation of electric shock, weakness, and inability to make some movements.
Radiculopathy
Compression of a nerve root by an intervertebral hernia. Numbness of an arm or leg depends on the level of compression and is accompanied by pain, muscle weakness, and impaired reflexes. At first it manifests itself as mild numbness of the extremities, gradually the symptoms increase. The pain decreases when lying down, but increases when the person stands, coughs or sneezes.
Metabolic polyneuropathy
It is characterized by a symmetrical lesion that develops due to a disturbance in metabolic processes in nerve fibers. It can be caused by diabetes mellitus, alcoholism, chronic renal failure, deficiency of vitamin B1, B12. Manifested by paresthesia, loss of sensation in the lower extremities, weakness, paresis.
Multiple sclerosis
Associated with the destruction of the myelin sheath (demyelination) of nerve fibers, which disrupts the conduction of nerve impulses. First, a transient sensation of numbness in the arms or legs appears, crawling along the fingertips, then the symptoms become more pronounced and permanent.
Polymyalgia rheumatica
Develops in people over 50 years of age. Accompanied by severe pain in symmetrical muscles, aggravated by movement, persisting at night. Most patients complain of muscle stiffness, numbness of the limbs in the morning and after prolonged immobility.
Factors of occupational hazard
Paresthesia is often caused by vibration and ultrasound. They damage peripheral nerves, cause loss of tactile sensitivity, numbness of the fingers, and intolerance to cold.
Author: Reznick JB
Translation: Kirill Kulik
Pain, swelling, bleeding, and muscle contracture are common during wound healing following extraction of impacted third molars. Complications are not that common and can be avoided if the case is carefully selected and the surgical protocol is followed. The purpose of this chapter is to discuss the potential complications following third molar extraction.
A retrospective cohort study by Bui, Seldin & Dobson found that the overall complication rate after extraction of mandibular third molars was 4.6%. There is less risk when working on maxillary third molars than when working on mandibular third molars. Risk factors include the patient's age, the position of the third molar in relation to the inferior alveolar nerve, and a complicated medical history.
Possible complications include paresthesia, alveolar osteitis, socket infection, bleeding, jaw fracture, osteomyelitis, adjacent tooth injury, buccal fat pad exposure, oro-antral communication, third molar migration, aspiration, periodontal tissue damage, and temporomandibular joint injury. The four most common complications according to publications are paresthesia, alveolar osteitis, socket infection and bleeding.
Paresthesia
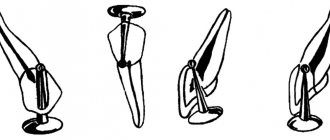
The impacted mandibular third molars are very close to the lingual, inferior alveolar, mylohyoid and buccal nerves (Figure 1)
Figure 1. Nerves pass near the lower third molar.
The possibility of developing paresthesia is often the reason why general dentists turn to maxillofacial surgeons. This usually occurs in situations where panoramic radiography indicates the location of the root of the lower third molar adjacent to the mandibular canal. However, as we know from Chapter 2, the roots of the lower third molar often overlap the mandibular canal on radiographs. Thus, the roots can be located more buccally or lingually than the canal.
There has been much research on the risk of nerve injury during lower third molar extraction. Some of them are given here.
Studies on the buccal and mylohyoid nerves
Although the buccal and mylohyoid nerves can pass near the third lower molar, they are rarely injured during its removal. In his study, Alves, after examining the heads of 10 cadavers, concluded that the buccal nerve crosses the anterior edge of the ramus far enough from the retromolar region that the risk of hitting the buccal nerve during the extraction process is very low.
According to Merril and MacGregor, the buccal nerve is often transected during incisions during third molar extraction, but little sensory change is noticed. The author found only one study focusing on mylohyoid nerve injuries. A 1992 Carmichael article states that mylohyoid nerve injury occurs in 1.5 percent of cases, probably due to retraction to the lingual side.
There is very little mention in the literature of possible damage to the buccal or mylohyoid nerve during the extraction of impacted mandibular third molars. Damage to the inferior alveolar and lingual nerves is much more common. Many studies have been conducted in an attempt to evaluate the risk of damage to these nerves during third molar extraction, and summaries of some of them are presented below.
Studies on the inferior alveolar nerve (IAN)
Sarikov and Juodzbalys conducted a systematic review of 14 studies. By
Diagnostics
Clinical symptoms are of great importance for making a diagnosis. Therefore, the doctor carefully asks the patient about when the disease began, how it manifests itself, and what helps.
Table 2. Differential diagnosis of numbness and tingling in the extremities. Possible reasons
| Affected limbs | Localization, features of numbness | Presumable disease |
| Upper | Sudden lesion of one arm. | Intervertebral disc herniation, spondylosis, osteochondrosis, plexitis, tunnel syndrome |
| Combined with impaired active movements. | Polyneuropathy, plexitis, tunnel syndrome. | |
| Symmetry. | Intoxication, infection. | |
| Blueness of fingers. | Raynaud's disease. | |
| Affects all fingers except the little finger | Carpal tunnel syndrome. | |
| Paresthesia of the little finger | Ulnar nerve neuritis, ischemic heart disease | |
| Lower | The pathological process affects the legs and lower back. | Osteochondrosis, lumbar hernia, atherosclerosis, pinched sciatic nerve, cauda equina syndrome. |
| Combined with impaired active movements. | Arthritis, multiple sclerosis, carpal tunnel syndrome, polyneuropathy, stroke. | |
| Damage to the lower leg and foot in combination with pain and muscle tension. | Thrombophlebitis, neuropathy, varicose veins. | |
| Paresthesia of the toes. | Arthritis of the thumb, radiculoneuritis, neoplasm, polyneuropathy. | |
| Top and bottom | Numbness of the left or right limbs | There may be several reasons: stroke, brain tumor, multiple sclerosis, transient ischemic attack. |
Accompanying illnesses
Paresthesia often develops against the background of such pathologies:
- sciatica;
- cervical spondylosis;
- diabetic neuropathy;
- transverse myelitis;
- restless legs syndrome (tingling and burning in the legs).
If complications occur, the disease can progress rapidly. Therefore, patients with these diseases should undergo periodic medical examination.
Treatment
Table 3. Numbness of the extremities: causes and symptoms, treatment
| Cause | Symptoms, examples of pathologies | Treatment |
| Circulatory disorders | Ischemia, arterial hypertension, thromboembolism. | Treatment of the underlying disease. |
| Orthopedic problems | Disc herniation, osteochondrosis. | Conservative or surgical therapy to eliminate compression of the nerve roots. |
| Nerve compression | Tunnel syndrome, polyneuropathy. | Elimination of tissue edema, restoration of metabolic processes. |
Medicines
Photo: posleudaleniya.ru
Of the B vitamins, preference is given to thiamine (B1) and cyanocobalamin (B12). It is better to use it as intramuscular injections to achieve the required concentration of the vitamin in the blood.
If there is a concomitant disease that increases the risk of developing blood clots, antiplatelet drugs (for example, aspirin) are prescribed. The action of this drug is aimed at preventing the formation of a primary blood clot by inhibiting the process of platelet adhesion. This helps improve blood circulation, as a result, eliminating the feeling of numbness.
Of the antihypoxants, Actovegin has a good effect. This drug consists exclusively of physiological components that are normally present in the human body. The active substance is a deproteinized hemoderivative of calf blood. Every cell in the body needs oxygen, which is used as energy. Actovegin stimulates oxygen consumption by the cell, thus exhibiting its antihypoxic effect.
One of the representatives of antioxidants is vitamin E. It is the main fat-soluble antioxidant that protects fatty acids in and around cells from free radicals and lipid oxidation. Often used in combination with another antioxidant, vitamin C. This vitamin protects muscle and nerve tissue from the effects of free radicals.