For almost everyone, dental treatment is a kind of test. There are risks of developing complications after an incorrectly installed filling or a poorly extracted tooth. There is also the possibility of undesirable consequences from the anesthetic injection. Local anesthesia is almost always used: treatment of deep carious cavities, pulpitis, periodontitis, tooth extraction, prosthetics, implantation, etc. If numbness after an injection does not go away for quite a long time, you need to identify the causes and find ways to eliminate the disease.
How long does it take for a painkiller injection to wear off?
Dentists use several types of anesthesia:
- Applique. An anesthetic in the form of a gel or ointment is applied to the desired area of the gum.
- Conductor. Administered by injection.
- Infiltration. Three-stage anesthesia is usually performed before complex manipulations.
After treatment or tooth extraction, depending on the type of anesthesia, a feeling of numbness remains. If pain relief was carried out correctly, without violating the technology of administering the anesthetic, the numbness goes away after some time.
Experts have identified maximum thresholds for each type of anesthesia:
- after application with gel or ointment, numbness disappears in no more than thirty minutes;
- after conduction anesthesia, the numbing effect lasts up to five to six hours;
- after infiltration anesthesia, numbness disappears within three to four hours.
In order to identify the maximum time threshold, it is also necessary to take into account the individual characteristics of each patient: age, weight, etc.
When do you need a doctor’s help and who to contact?
How long does numbness last after tooth extraction and when is it time to sound the alarm? It was already mentioned above that sensitivity should be restored a few hours after the anesthetic injection was given. But situations are different - for example, after a complex removal of the “eight”, after osteoplastic surgery or installation of an implant, etc. numbness can last 1-2 days, less often up to 5-7 or even up to 10-14 days. But, as practicing dentists note, sensitivity is restored after 2 weeks in almost all patients. If after 14 days there is no improvement, then you need to go to the doctor. To begin with, you can contact the dentist who performed the previous treatment, then you can contact a neurologist or a neurophysiologist.
Read on the topic: is it necessary to take an x-ray after a tooth has been removed?
Possible complications
The human factor plays a huge role in all dental procedures, including the administration of anesthetic.
Complications that may occur after local anesthesia:
- Unpleasant sensations in the injection area. Injecting the medicine too quickly or too slowly may cause pain.
- Hematoma at the site of needle insertion. The formation of a hematoma indicates problems with blood vessels or that the injection site was chosen incorrectly.
- Allergy. An allergic reaction to one or even several components of an anesthetic.
- Inflammatory process, development of infection. This is possible if errors were made during the administration of the anesthetic, due to which microbes penetrated the soft periodontal tissues and caused inflammation.
- Numbness of the facial muscles. The patient cannot control his facial expressions and cannot close his lips.
Local complications and errors during the anesthesia procedure
Before any surgical intervention in the maxillofacial region, it is necessary to carry out complete tissue analgesia, since anesthesia in dentistry is not only a humane attitude towards the patient, but also a method of pathogenetic therapy, which is used in the treatment of any inflammatory process and diseases of a traumatic nature that develop in shock zone.
The doctor cannot expect that the disease will proceed without complications if he performed the intervention without providing complete anesthesia in the area of injury or inflammation.
Inadequate pain relief is one of the most common mistakes made by clinic doctors when treating patients in all areas of their specialty.
Another common mistake doctors make is administering the anesthetic too quickly. Under no circumstances should it be allowed during infiltration anesthesia of soft tissues. The anesthetic is injected under high pressure, so a depot of anesthetic solution, which is necessary for tissue infiltration near the needle tip, is not formed. Instead, the solution is shot into the depths in the form of a jet and disperses. The desired analgesic effect is not achieved.
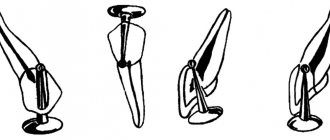
When introducing an anesthetic into the bone, for example, when performing intraligamentary anesthesia, the desired effect is achieved precisely when the drug is administered under high pressure. However, even in this case, it must be taken into account that too rapid administration of the drug can cause rupture of the periodontal ligaments of the tooth and its displacement from the socket.
Another type of complication is damage to the vessel by the injection needle and the formation of a hematoma. This complication is common with intraoral “tuberal” anesthesia. In rare cases, it occurs during anesthesia of the infraorbital nerve. Taking into account the fact that anesthesia of the area near the tubercle of the upper jaw almost always leads to the formation of a hematoma, and its suppuration leads to the formation of phlegmon of the pterygopalatine fossa and infratemporal space, which seriously threatens the patient’s health, it is necessary to abandon the use of this method of anesthesia. In addition, infiltration anesthesia using modern means ensures the achievement of the desired anesthetic effect for any type of dental intervention in the area of the anatomical structures of the upper jaw.
In order to prevent the occurrence of a hematoma during anesthesia at the lower orbital foramen, it is necessary to advance the needle in the direction of distribution of the solution. You should not insert a needle into the canal, since modern anesthetics have diffusion capabilities that allow the injected drug to quickly spread and block the nerve trunk. If there is a suspicion of the development of a hematoma, then it is necessary to clamp the area of tissue with a tampon for several minutes. After the analgesic effect is achieved, the planned intervention can begin. You can also use hypothermia, and after three days - resorption therapy.
A rare, but more serious complication is the breaking off of an injection needle. Most often this happens if the anesthesiologist makes too sudden a movement when the syringe needle is already in the muscle tissue. The risk of complications increases if the needle is completely immersed in the tissue. In order to avoid complications, it is necessary to control the quality of the needles used for injections, as well as the extent to which the doctor adheres to the rules of anesthesia. Do not allow the needle to be completely immersed in the tissue or make sudden movements with the injector. If the needle does break off, it can be removed on an outpatient basis only if the end is visible above the surface. If tissue dissection is necessary to remove a broken needle, the patient must be hospitalized. An X-ray examination must be done before surgery. X-rays should also be taken at the stage of the operation, the volume of which can be significant.
Damage to the nerve trunk by an injection needle is relatively common, resulting in the development of traumatic neuritis, which is accompanied by paresthesia or severe pain. To prevent this from happening, the needle must be advanced in the direction of the anesthetic flow. If paresthesia or pain appears, it can last from 3 days to a week and even up to several months. In this case, taking B vitamins and analgesics, as well as physiotherapeutic procedures, are indicated.
If the fibers of the internal pterygoid muscle are damaged by an injection needle, its contracture may develop and the function of the lower jaw may be impaired. In order to prevent complications from developing during anesthesia of the inferior alveolar nerve, you must carefully follow the technique of advancing the needle to the bone of the inner surface of the jaw branch to the mandibular foramen. Most often, contracture can be eliminated within a few days using physical therapy and painkillers. If its course is prolonged, then mechanotherapy should be performed. Even more severe damage to the nerve trunk or muscle fibers can occur when the tip of the injection needle is bent; for this reason, syringes with a deformed needle should not be used.
Post-injection pain and swelling can occur due to trauma to the periosteum, or as a result of too intense injection of anesthetic into the soft tissue. Another cause of complications lies in the use of expired painkillers. Prevention of such complications comes down to compliance with the rules of anesthesia. It is necessary to exclude subperiosteal and too intense injection of an anesthetic solution into the tissue, as well as the use of anesthetics that have been certified and have not expired.
Treatment of complications is reduced to physiotherapeutic procedures. It is also recommended to use painkillers and antiallergic drugs, such as diphenhydramine and suprastin.
Paresis of facial muscles develops as a result of blocking the branches of the facial nerve with an anesthetic drug. This can be observed during extraoral anesthesia on the maxillary tubercle and during anesthesia of the inferior alveolar nerve. The paresis of individual facial muscles that develops as a result goes away after the painkiller wears off and does not require treatment.
The development of diplopia (double vision) is possible when the anesthetic solution spreads into the infraorbital canal with appropriate anesthesia, resulting in paresis of the extraocular muscles. This complication goes away on its own after the effect of the anesthetic wears off.
The most serious complication that threatens the health and even the life of the patient is tissue necrosis; it develops as a result of the introduction of a non-isotonic solution by mistake. This could be alcohol, calcium chloride, gasoline, or some other drug. The first sign of necrosis is severe pain that occurs at the beginning of solution administration. It is necessary to immediately stop administering the drug, infiltrate the tissues with a diluted anesthetic and, if possible, cut the tissues wide to allow intensive drainage. If a non-isotonic solution was injected into deep tissues, then after first aid the patient should be immediately hospitalized. This is necessary because severe tissue swelling may soon develop, possibly spreading to the neck, causing difficulty breathing and requiring emergency resuscitation.
When observing patients who were mistakenly injected with aggressive liquids during anesthesia, in one of the patients, due to the administration of a non-isotonic solution near the mandibular foramen, necrosis of the pterygomaxillary, perimaxillary space and the lateral surface of the neck began to rapidly develop. On the eleventh day, bleeding appeared, which is why the external carotid artery had to be ligated. Another patient was mistakenly injected with alcohol into the pterygomaxillary space, which resulted in persistent contracture of the lower jaw and extensive tissue scarring. This required extensive surgical intervention. The erroneous administration of 2 ml of a vasoconstrictor drug to a teenager ended tragically.
For preventive purposes, to avoid such complications, carpule technology is used. This eliminates errors when selecting an anesthetic drug.
Symptoms and causes of numbness after an injection
Numbness of the jaw after anesthesia is considered normal. But if it is accompanied by the following symptoms, you should seek the help of a doctor:
- numbness, burning or tingling of the tongue;
- numbness of the cheek;
- painful sensations in the tooth;
- sagging of the lower parts of the face;
- excessive salivation;
- pulsation in the gum.
Factors that influence the occurrence of symptoms:
- when injecting the anesthetic, the needle entered a blood vessel;
- a nerve was damaged during the injection;
- due to increased toxicity, the anesthetic itself caused numbness.
A little about the anatomy and course of the branches of the trigeminal nerve
The teeth of the upper and lower jaw are innervated by the branches of the trigeminal nerve, which provide all types of sensitivity directly to the teeth, skin and mucous membrane of the lips and cheeks. The lower jaw - by the mandibular nerve, the upper - by the alveolar branches of the maxillary nerve, forming the dental plexus.
The alveolar branches of the maxillary nerve pass along the wall of the maxillary sinus to the apexes of the roots of the upper teeth, where they form a nerve plexus responsible for the sensitivity of the upper teeth and gums. The mandibular nerve passes through the bone canal of the same name, innervating the lower teeth and gums, lower lip, and part of the cheek.
Computer anesthesia
In order to eliminate the possibility of developing complications after an injection, modern dentistry uses computer anesthesia.
Advantages of the technique:
- There is no numbness of soft tissues. Computer anesthesia only numbs the area where the anesthetic is injected.
- Computer anesthesia is painless.
- The pressure of the anesthetic is controlled by a computer, so it is administered at the desired speed and in smaller quantities.
- There is no feeling of gum swelling.
- The influence of the human factor is eliminated due to the fact that the computer controls the entire process.
- The tip is shaped like a pen, which is less intimidating for patients who are afraid of injections.
Diagnostics
If partial or complete numbness occurs after sinus lifting and bone grafting, you should undergo a number of diagnostic procedures:
- Examination of the oral cavity by a dentist. Allows you to assess the general situation and in some cases even make a diagnosis immediately. Must go through first. If there is displacement of the implant or nerve injury during surgery, then further examination methods can be of a purely clarifying nature.
- Assessment of neurological status based on damaged branches of the trigeminal nerve. This task is more likely for a neurologist, rather than for a dentist. By testing reflexes and using special methods to determine sensitivity, it is possible to assess the presence/absence of nerve damage.
- X-ray or computed tomography. These examination methods make it possible to establish in detail and accurately the cause of loss of sensitivity. With the use of modern technologies, it becomes possible to calculate down to the millimeter the direction and degree of displacement of the installed structure, existing pathological foci of regeneration, and determine the presence of an inflammatory process both at the site of bone grafting and directly in the maxillary sinus.
Main causes of nerve damage during implant placement
Damage to the maxillary or mandibular processes of the trigeminal nerve, which is the main cause of long-term numbness of the lips, tongue, and chin after dental implantation, can be caused by an unintentional mistake by the dentist or negligence. Damage to the mandibular nerve, which provokes paresthesia, can occur in the following cases:
- Incorrect selection of implants (chosen too long).
- The specialist has not studied the anatomical features of the jaw and the implanted implant touches the nerve ending.
- Injury to the nerve ending by a needle during the administration of anesthesia or dental instruments during bone preparation.
If numbness in the lower part of the face is caused by injury to the nerve endings during the administration of anesthesia, the discomfort will go away on its own after the nerve fibers heal. Typically, the healing period ranges from 3 months to six months. You can understand that numbness of the lip and chin after implantation is associated with damage to the trigeminal nerve by the presence of the following signs after surgery:
- salivation increases;
- difficulty eating;
- facial expressions and articulation are impaired;
- the sensitivity of the tongue and lips decreases;
- there is pain and discomfort in the implant area;
- numbness is felt on the side where the titanium root is implanted.
Chief physician, Salatsky Dmitry Nikolaevich
Sign up for a free consultation
+7
If the feeling of numbness in the lower jaw does not decrease within several hours after implantation, then an urgent consultation with the doctor who performed the operation is necessary. Only after conducting diagnostic studies will a specialist be able to identify the extent of nerve damage and, based on this, prescribe appropriate treatment.
What to do, how to treat
Treatment of paresthesia due to unsuccessful implantation can be prescribed by the implantologist who performed the operation, dentist, neurologist, or physiotherapist.
Before moving on to restorative therapy, a diagnosis must be carried out, during which the nature and extent of the damage is established. The treatment is carried out comprehensively, aimed at restoring the conductivity and sensitivity of nerve fibers .
If the patient consults a doctor immediately, drug therapy in combination with physiotherapeutic procedures is very effective. In other cases, surgery is required.
Treatment
Numbness after anesthesia goes away on its own if no damage or disturbance has occurred. In case of complications after surgery, the help of a specialist is necessary if:
- numbness after treatment or removal does not go away after 24 hours;
- when removing a wisdom tooth - after 1-5 days.
The nerve is completely restored after 2-3 weeks. Associated symptoms should be taken into account. Shooting pain in the tooth, burning sensation in the gums, sagging tissue indicate disturbances that occurred as a result of the operation. Nausea or vomiting is a sign of poisoning in the body. In difficult cases, treatment is required.
Complications after the use of anesthesia are quite common. If the damage is not too complex, and the doctor’s recommendations are fully followed, then surgery can be avoided.
Medicines
To restore damaged nerves and normalize blood circulation, dentists prescribe:
- vitamin complexes containing vitamins B and C;
- Actovegin, Piracetam and other medications.
Folk remedies
At home, rinsing with oak bark and chamomile decoction is used to relieve inflammation. Valerian root is used in an infusion, as it has a sedative effect and relaxes muscles. Furacilin solution has proven itself well; it is used for rinsing.
It is not recommended to use heating or cooling yourself. Despite the feeling of relief in the first minutes, such procedures can cause harm.
Physiotherapy
Dentists resort to prescribing ultrasound therapy to warm up the designated areas. This promotes tissue restoration.