Summary
Reconstruction and rehabilitation of patients with defects of the upper jaw are the most difficult in reconstructive maxillofacial surgery, occupying the minds of oncological surgeons working in this area, microsurgeons, plastic surgeons and orthopedic dentists involved in maxillofacial and somatotropic prosthetics.
The fundamental difference between patients who have undergone anatomical reconstruction of the alveolar process of the upper jaw, as well as nasal support with microsurgical grafts and patients who have undergone maxillofacial prosthetics with obturation structures is an increase in the volume of the respiratory space, improved speech, the absence of atresia, frequent acute respiratory viral infections and, fundamentally, in the absence of regular relocation of definitive orthopedic work [1]. An important difference is also the lack of mobility of dentures on dental implants, which avoids chronic trauma to surrounding tissues.
This article describes the experience of rehabilitation of patients with defects of the upper jaw using fibular and Chinese skin-bone flaps with further plastic surgery of bone and soft tissues in order to create conditions for dental implantation, orthopedic conditions and features of fixed prosthetics for this group of patients.
The developed protocols for the use of a particular graft on a vascular pedicle are described in terms of the type of defect and further restoration of bone joints, as well as measures for the formation of anatomically close to normal conditions for implantation and prosthetic dentistry in patients with a reconstructed upper jaw.
Total prosthetics after tooth extraction
The situation is considered separately - the removal of all teeth immediately before prosthetics. In this case, the patient is faced with complete adentia, which requires emergency treatment.
Option two:
- Removable prosthetics - quickly, inexpensively, with guaranteed atrophy of bone tissue subsequently, frequent replacement of the prosthesis and inconvenience of wearing the product.
- Implantation with installation of a fixed prosthesis - according to all-on-4 or all-on-6 protocols. The essence of the treatment is the installation of a fixed number of dental implants and the attachment of a full denture prosthesis to them. Implantation of 4 or 6 artificial roots is performed on the day of removal. An impression is immediately made, from which artificial teeth are made in a dental laboratory. The longest waiting period is 3 days, after which the patient receives a full-fledged jaw capable of withstanding all physiological loads.
Introduction
The upper jaw is the most complex area in reconstructive maxillofacial surgery, being more responsible for appearance than others, and due to the presence of such organs and anatomical formations as the eyes, zygomatico-orbital complex, and teeth.
The upper jaw is a support for the lower jaw from the point of view of the stationary container of antagonists, also a zone of concentration of air cavities and a complex of buttresses. Defects and deformations in this area lead to disfigurement and limit or make impossible vital body functions such as chewing, swallowing, breathing, and vision. Restoration of buttresses is necessary from the point of view of optimizing the transfer of stress of the masticatory load, as well as to strengthen the reconstructed alveolar process of the upper jaw. [3]
Despite the positive results of tissue autotransplantation using microsurgical techniques, creating conditions for fixed and conditionally removable dental prosthetics remains a serious problem. The presence of a skin area with an array of subcutaneous fat makes the creation of an orthopedic bed and the attachment of soft tissues around the completed orthopedic structures almost impossible and reduces the functional significance of the work performed aimed at the rehabilitation of the chewing function. [2]
The article is devoted to the synergistic efforts of a maxillofacial surgeon and an orthopedic dentist to create functionally significant conditions and long-term results in patients with reconstructed upper jaws using skin-bone autografts on a vascular pedicle.
In the world literature available to us on the rehabilitation of chewing function in patients with jaw defects, we did not find any descriptions of the formation of a prosthetic bed, features of the choice of orthopedic structures, or long-term results after dental prosthetics.
Key words: jaw defect, lack of occlusion, obstructive prostheses, dental implantation, fixed prosthetics, integrated implants, micro-surgical autotransplantation, bone grafts, fibula, parietal bone, three-dimensional bone augmentation.
Material and methods
From 2008 to 2014 in the reconstruction of the upper jaw, we used a fibular autograft for the reconstruction of total defects (5 cases) and a radial autograft for the reconstruction of subtotal defects (10 cases). When using a radial skin-bone autograft in the subsequent placement of dental implants, there is a need to recreate the second cortical-spongy layer of the alveolar process on the lingual side, which can be achieved using parietal or mandibular free autoblocks.
With VRGN, relatively small defects of the alveolar process of the frontal part of the upper jaw are noted; more often the problem is the elimination of the defect of the palatal plate. Bone reconstruction requires the alveolar process, represented by genetically modified bone tissue in the projection of the bone cleft. A palatal bone defect does not require repair, since functional loss does not occur in the absence of reconstruction of the bone component. It should be noted that with complete clefts the main problem is communication with the nasal cavity. To eliminate defects of the upper jaw, we have developed a technique for using a free split chin graft and transplanting a fasciocutaneous graft [Application: 2010118686/14, 05/12/2010. Patent No. 2435537 ](4 cases).
In cases where the patient's health condition did not allow microsurgical transplantation, we installed Zygomatic system implants and fixed prosthetics (6 cases).
After a clinical assessment, instrumental diagnostic methods were used to study the pathology of the integrity of the jaw/s: OPTG, TRG, CT (with angiocontrast and soft modes).
If a tumor was present, the extent of resection was assessed and the optimal graft was selected according to the developed algorithm. If the X-ray picture of the tumor was detected, a biopsy was performed and, when the diagnosis was verified, resection of part or all of the jaw was performed. For jaw defects, after clinical and instrumental analyses, treatment planning began.
Preoperative planning was carried out using 3D visualization programs that made it possible to simulate the sizes, shapes, and position of the revascularized autografts relative to the bone structures, taking into account the positioning of the condylar processes of the mandible in the temporal fossae (anterior-superior position in the articular cavities) according to CT studies and the formation of anatomical buttresses for the upper jaw. A special feature of the programs is the absence of distortions in the individual dimensions of the patient’s skull.
We used fibular and radial autografts, since only they allow us to perform 3D modeling of the bone component congruent with the defect in the maxillary defect. Subsequently, when using a radial graft, the technique of transplanting free cortical-cancellous grafts was used to thicken the alveolar process for further dental implantation. Thus, a comprehensive and step-by-step reconstruction of the jaw defect was carried out to create conditions for restoring chewing function with fixed and conditionally removable orthopedic structures, which is important for any jaw defects.
After engraftment and activation of the dental implants, the subcutaneous fat pad of the fibular and radial flaps and the removal of excess skin pad were removed.
Orthopedic rehabilitation consisted of choosing the design of the prosthesis and precise adherence to the accuracy of taking impressions to transfer the complex relief of soft tissues and the position of the implants onto precise plaster models. The usual occlusion and central relationship of the jaws were recorded for the subsequent selection of prosthetic tactics for patients with reconstructed upper jaws. Plaster models were installed into the articulator using a facebow. The existing occlusion and centric relation were assessed. Depending on the type of defect, we selected the desired position of the lower jaw to create optimal chewing function and aesthetic results.
Particular attention was paid to the creation of a prosthetic bed for a future orthopedic design supported by dental implants. In these clinical situations, there is no attached keratinized mucous membrane around the implants in the oral cavity, which makes it difficult to accurately transfer the relief of the soft tissues of the prosthetic bed to create adapted non-removable orthopedic structures.
After the manufacture and fixation of temporary crowns on the implants, the presence of tumor-like growths of the mucous membrane around the installed orthopedic superstructures, which were histologically described as polyps, was noted. Patients complained of bleeding and discomfort around the installed crowns. Attempts to change the eruption profile of structures from implant shafts did not produce a positive result.
We used a method of simultaneous surgical correction of the subcutaneous fat area of autografts with the installation of provisional structures supported by dental implants. In a number of cases, we used a removable compression acrylic plate on the gum formers, which held the surgically created profile until permanent prosthetics or installation of provisional fixed and conditionally removable structures.
After 3 months, we made permanent orthopedic fixed or conditionally removable structures.
For the manufacture of orthopedic structures, we used cobalt-chrome alloy, titanium and zirconium dioxide.
As a rule, after the integration of implants and placement of gum formers at the prosthetic stage, we were faced with the need to modernize the prosthetic elements of the implantation system for specific clinical cases.
The gum formers were needed to be longer and predominantly conical in shape. The cylindrical shape of the gum former created parallel walls of the crater of the mucous membrane, which caused rapid collapse of the walls during the placement of the impression coping and caused severe discomfort to patients during manipulations. We attribute this to the presence of excess connective tissue layer, which is located on the autograft bone.
It is important to note that immediately after corrective operations on the skin-fat part of the flaps, orthopedic compression plates were fixed to prevent further growth of the soft tissue component.
Patients were monitored every seven days and appropriate compression plate adjustments were made.
Depending on the chosen permanent structure, a set of further orthopedic manipulations was carried out to make prostheses.
The results were recorded using a Canon D 60 camera, 100 mm lens, and MR-100 ring flash.
Description of clinical observations
Patient U. , 18 years old, was admitted to the clinic on April 1, 2008 with a diagnosis of osteoblastoma of the upper jaw, a condition after subtotal resection of the upper jaw on the left. From the anamnesis: a neoplasm was discovered and removed in early childhood at the Federal State Institution Central Research Institute of Infectious Diseases and Maxillofacial Surgery. The patient was sent to the clinic of the Russian Scientific Center for Surgery named after. acad. B.V. Petrovsky.
Status localis: the configuration of the face in front and profile is changed, the upper lip is retracted on the left. On palpation, a defect in the alveolar process of the upper jaw on the left is noted.
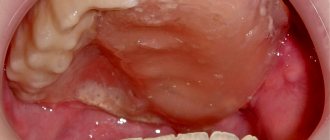
Mouth opening is not limited, there is a through defect in the alveolar process of the upper jaw with teeth 21-28, the patient wears an obturating denture, the denture teeth are in the bite.
Bite according to the second class according to Angyu.
On OPTG and CT: there is a defect of the zygomatic tubercle, alveolar process on the left, absence of the spine of the upper jaw, the base of the pyriform foramen on the left, defect of the tubercle of the upper jaw on the left. An impacted 28th tooth is noted in the remains of the pterygomaxillary articulation.
Treatment tactics: since the defect of the upper jaw was subtotal and through, a radial skin-bone graft on a vascular pedicle was used. When transplanting a radial cortico-periosteal-skin graft, a zygomatic-maxillary buttress was formed using a free split graft from the branch of the mandible on the right. The second stage involved the formation of the alveolar process using parietal grafts.
Rice. 1. Appearance of the patient, existing defect of the upper jaw, bite, obturating prosthesis, CT scanThe patient was noted to have no nasal lining, and to anatomically restore aeration, before transplanting a microsurgical graft, the nasal lining was formed with local tissues.
Rice. 2. Stages of planning the bone and soft tissue components of the graft Rice. 3. Stages of surgeryRice. 4. Computed tomography of the patient after surgery and condition on the third day
Rice. 5. Scintigram after surgery
In the postoperative period, there was a divergence of the sutures and a reduction in the volume of the flap, and therefore a protective mouth guard was made to protect the soft tissue component of the flap from food getting into the graft. Kappa also pressed the flap into the defect area to allow healing by secondary intention.
Rice. 6. Postoperative mouth guard
2 months later, the patient, being a cycling athlete, fell from the “saddle” and received a fracture of the upper limb at the site of collection of the radial skin-cortical-periosteal graft on the vascular pedicle. Therefore, the patient underwent osteosynthesis with the Ilizarov apparatus.
Rice. 7. Condition after osteosynthesis of the upper limb on the left, condition in the oral cavity
After 5 months, we installed three dental implants in the area of the reconstructed alveolar process using parietal bone autografts. Thanks to this technique for reconstructing the alveolar process, it was possible to obtain adequate bone thickness and height for placing dental implants.
Rice. 9. Implantation in the area of 3D reconstruction with parietal blocks
After 5 months, we opened the implants and applied a method of one-stage surgical correction of the subcutaneous fat pad of the autograft with the installation of elongated gum formers in dental implants, which simplified the formation of soft tissues during surgery.
After completion of the surgical stage, the alginate impression was removed from the upper jaw and a compression plate was made using cold polymerization at a pressure of 3 atmospheres from acrylic plastic.
The patient was advised to wear the plate constantly, removing it only for hygiene procedures. Inspection and correction of the plate fit were carried out every seven days for a month.
Thus, we were able to form a stable mucosal contour around the gingival formers.
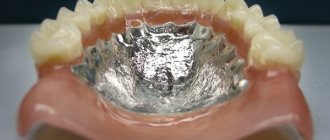
The next stage was the production of a conditionally removable prosthesis supported on a beam structure on implants.
Rice. 10. Correction of the subcutaneous fat area of the autograftConsidering the fact that microsurgical elimination of the jaw defect and reconstruction of the alveolar process was carried out by transplantation of free parietal cortical autografts, the further stage of orthopedic rehabilitation is practically no different from classical prosthetics for patients with an extended terminal defect of the dentition.
In order to be able to produce a conditionally removable beam-type prosthesis supported by implants, it was necessary to produce an accurate plaster model that displayed the entire relief of the prosthetic bed and accurately reproduced the position of the implants. To do this, we took primary impressions of the upper jaw using Clip-transfers for implants. The primary plaster model gave us the opportunity to make a custom impression tray with prepared transfer checks for precise transfer of the position of the implants.
Having made an accurate working model of the upper jaw and a model of the antagonists, we installed them in the articulator according to the average parameters. Registration of the central ratio was carried out using an occlusal hard wax plate with refinement on ALUWAX (soft wax with the addition of aluminum filings for long-term heat retention and elasticity).
Rice. 11. Impressions and plaster models
After analyzing the relationship of the plaster models in the articulator, we manufactured a beam frame supported by three implants. The beam frame was made by vacuum casting from cobalt-chrome alloy. To achieve a passive fit of the frame, we used adapters for external connection with the implants.
We fixed titanium ball locks into the cast part of the frame. Then a model of the upper jaw was made from a fire-resistant mass for modeling and casting the mating part of the prosthesis itself.
Rice. 12. Beam frame and mating part of the prosthesisTaking into account the possibility of changing the relief of the soft tissue component of the autograft, the frame of the response part was modeled in such a way that it was possible to change the acrylic base part, changing the fit of the prosthesis to the bed.
After fitting the beam and frame in the oral cavity, we manufactured the base part of the conditionally removable denture with the installation of acrylic artificial teeth, using the method of cold polymerization of plastic under a pressure of 3 atmospheres and a temperature of 50 degrees Celsius. We took into account all possible characteristics of the patient at rest and when smiling, creating the most natural appearance of the entire orthopedic restoration.
The final fixation of the prosthesis was carried out in a certain sequence:
- Cleaning and disinfection of all components of the prosthetic restoration.
- Removing the gum formers, irrigating the internal shafts of the implants with a solution of 3% hydrogen peroxide and 0.05% chlorhexidine solution, installing adapters on the external connection.
- Installation of the beam structure on three implants, tightening the fixing screws with a force of 30 N/cm2.
- Fixing the actual removable denture on the beam frame, checking the occlusion, teaching the patient about hygienic measures.
Prosthetics using implants
Today, implantation is the most effective method of restoring teeth. Implants can be installed for both partial and complete edentia.
The implant plays the role of a durable artificial root. It is implanted into bone tissue. The support necessary to put on the crown is attached to it. With proper care, the implant will serve the patient throughout his life. Replacements may require solely a crown.
The huge advantage of this method is that the bone tissue does not atrophy after tooth extraction. In modern dentistry, implantation can be performed in one operation - immediately after the removal of a dental unit, an implant is implanted in its place.