Author of the article:
Soldatova Lyudmila Nikolaevna
Candidate of Medical Sciences, Professor of the Department of Clinical Dentistry of the St. Petersburg Medical and Social Institute, Chief Physician of the Alfa-Dent Dental Clinic, St. Petersburg
Inflammation of the gums, or periodontitis, is one of the most common dental diseases. This pathology of the oral cavity can occur due to both chronic diseases and local traumatic injuries.
The main symptom of periodontitis is an acute inflammatory process of gum tissue. Lack of treatment can lead to the development of severe forms of the disease, characterized by tooth loss and displacement.
Prevention and treatment of periodontitis at home
The most effective method of treating almost any disease, including periodontitis, is its prevention. There are simple prevention methods that can be used at home. Their use will prevent the occurrence of periodontitis symptoms and avoid the need for drug and surgical treatment.
The main thing that needs to be done to prevent any pathologies of the oral cavity is to strictly follow the principles of dental hygiene:
- brush your teeth twice a day with therapeutic and prophylactic toothpaste using a medium-hard brush;
- After a meal, remove leftover food using dental floss.
- a rinse with an antibacterial effect, for example, Asepta based on lemon balm, calendula or St. John's wort extract, has a soothing effect on the gums;
- it is necessary to regularly consume solid and plant foods, ensuring sufficient chewing load on the teeth;
- one of the reasons for the development of periodontitis is a lack of vitamins A, C and B vitamins in the diet. To prevent the disease, it is recommended to take a vitamin complex containing a sufficient amount of these vitamins;
- You should visit your dentist twice a year for preventive teeth cleaning. Timely removal of plaque and tartar will help avoid gum inflammation and further development of pathology.
How to treat periodontitis correctly:
Treatment of periodontitis will depend primarily on the severity of the inflammatory process in a particular patient. The more significant the level of bone loss and the degree of tooth mobility, and the more missing teeth you have, the more difficult, time-consuming and expensive the treatment will be. It all starts with a consultation, and you should not go to a regular dental therapist, but only to a periodontist (this is a doctor who specializes in the treatment of gum inflammation).
The author of this article has worked as a periodontist for more than 10 years, and therefore all our recommendations, which you will see below, really work (state-issued documents on advanced training in the Periodontology program can be viewed in the editorial section).
Consultation with a periodontist –
The first thing to do is make a treatment plan. This is not as easy to do as it might seem in reality. If the disease is mild, you may only need to consult a periodontist. However, in case of mobility and divergence of teeth, malocclusion, when there are already missing teeth or those that will definitely have to be removed, a joint consultation with an orthopedic dentist (prosthetist) is necessary.
X-ray diagnostics – for a full consultation, a panoramic X-ray will be required to assess the level of bone tissue destruction, location and depth of periodontal pockets. The image will allow you to make the correct diagnosis, which will include the severity of your disease. For the patient (whose panoramic image is shown below), the diagnosis will be as follows: “Chronic generalized severe periodontitis.”
Pay attention to the photo. You can notice that the level of bone tissue (looks like light, finely looped cellular tissue in the picture) is reduced in some teeth by 2/3 of the root length, and in a small number of teeth - only by 1/4. The patient has roots that need to be removed, as well as caries that requires treatment. It is especially noticeable that the bone level is maximally reduced in the front teeth of the upper and lower jaws, which is also due to their chewing overload (due to the absence of a large number of lateral teeth).
In similar situations, if a decision is made to preserve the front teeth, it is necessary to make a temporary removable denture as quickly as possible. It will replace missing teeth and relieve increased chewing load from the front teeth.
Removal of supra- and subgingival dental plaque –
The cause of periodontitis is soft microbial plaque, as well as supra- and subgingival dental plaque. Treatment cannot be effective without removing the causative factor, and therefore the basis of treatment for inflammatory gum diseases is high-quality removal of dental plaque. There are 2 main techniques that can be used in patients with periodontitis:
- ultrasonic teeth cleaning,
- Vector system.
How ultrasonic teeth cleaning is carried out (video) –
There are fundamental differences between ultrasonic scalers and the Vector system, but we do not want to overload this article with unnecessary information (therefore, you can read more about the Vector system at the link above). The only thing worth adding here is that at the 1st stage of treatment, in any case, you need to use only the classical ultrasound technique. And so to speak, “polishing the result” can be done in about 4-6 weeks using a Vector-Paro device, but it will cost 3-4 times more than conventional ultrasonic cleaning.
Important: in patients with periodontitis, it is simply impossible to remove all dental plaque in just 1 visit, and it is usually necessary to make appointments with patients several times. This is due to the fact that searching for and removing subgingival dental plaque requires a lot of time. In addition, the patient comes to the second appointment with less swollen and inflamed gums, which leads to a decrease in its volume, as well as, to a small extent, the depth of periodontal pockets. Accordingly, thanks to this, we will be able to look deeper on the 2nd visit and see subgingival tartar, which we had not previously noticed and missed.
In addition, it is important not only to remove subgingival tartar, but also, if possible, to polish the exposed surface of the tooth roots in the depths of periodontal pockets. The latter is done by careful movements of the ultrasonic tip nozzle, using special nozzles at low power. Otherwise, the rough surface of the root will contribute to the rapid formation of a new portion of subgingival tartar. In general, removing plaque from periodontitis is not easy, it is not quick, and it requires the patience and perseverance of a doctor, and by definition, this cannot be cheap. It will be cheap only if you remove the tartar “quickly”.
Anti-inflammatory therapy for periodontitis –
The course of anti-inflammatory therapy for periodontitis usually lasts 10 days. It is prescribed by a periodontist immediately after the 1st session of removing dental plaque. The course will necessarily include medications for local use in the oral cavity - these are antiseptic rinses and anti-inflammatory gel for the gums, which the patient will use at home. In addition, if there is purulent or serous-purulent discharge from periodontal pockets, antibiotics are prescribed internally.
ANTI-INFLAMMATORY THERAPY SCHEME:
It is prescribed by a dentist, and carrying out such anti-inflammatory treatment of periodontitis on your own is not at all difficult. The standard course of treatment lasts only 10 days. Treatment of gums should be carried out by the patient 2 times a day - morning and evening. It looks like this... In the morning, treatment is carried out after breakfast and oral hygiene (it is important - breakfast first, and only then brushing your teeth, and not vice versa). Likewise in the evening - first dinner, then brushing your teeth, and only then are antiseptic rinses and applications of gel to the gums.
So, after breakfast/dinner and oral hygiene, you must first perform an antiseptic mouth rinse with a 0.2% chlorhexidine solution (we will tell you why the standard 0.05% solution is not very effective for these purposes). To do this, you must take approximately 10 ml of solution into your mouth, which is 1 average sip. And then, without spitting anything, you should rinse your mouth for exactly 1 minute. Important: after an antiseptic rinse, you should not rinse your mouth with water.
Applying gel to the gums – the second stage of treatment is applying an anti-inflammatory gel to the gums. Over the 10 years of working as a periodontist, I have tried many different drugs, but I responsibly declare that Cholisal gel works best. An important point - before applying the gel to the gums, it is advisable to dry them with a dry gauze swab (it can be made from a bandage), because Any gel will adhere better to the dried mucous membrane.
The application of the gel to the gum is carried out in front of a mirror, and you must grin so that during the procedure you can see the edge of the gum and where exactly you are applying the gel. The gel must be applied with your finger - precisely on that part of the gums that is located around the necks of the teeth (gingival margin), and this must be done not only from the front surface of the dentition, but also from the palate / tongue. Now let's look at how exactly you need to apply the gel to the den.
If we are talking about treating the gums from the front surface of the teeth, then it is better to do it in two stages. First, you squeeze a little gel onto your finger several times and rub it into the gum margin with light massaging movements. Then squeeze the gel onto your finger again, and then apply it to the gum edge, without rubbing. As for the treatment of the gums from the side of the tongue/palate, it can be done once - only by rubbing small portions of the gel with light massaging movements.
Important: saliva will always be released during the application of the gel, and there is no need to accumulate it or spit it out. You must swallow it - as you usually do. In addition, after applying the gel to the gums, it is advisable not to drink anything for 30-60 minutes, and also not to eat or rinse your mouth for 2-3 hours. The second treatment of the day is carried out in the evening according to a similar scheme (dinner → brushing teeth → antiseptic rinse → gel application). And so on for 10 days.
An important question regarding the concentration of chlorhexidine is
There are clinical studies (source) that show the comparative effectiveness of different types of antiseptics and their different concentrations in the treatment of chronic generalized periodontitis. The fact is that in most patients with periodontitis, not only pathogenic bacteria live in periodontal pockets, but also fungal flora. The presence of fungal flora in periodontal pockets has a very important impact on the effectiveness of anti-inflammatory gum therapy in general.
Despite the fact that gum inflammation during periodontitis is caused directly by pathogenic bacteria, the presence of fungal flora makes these bacteria less sensitive to antiseptics and antibiotics. Accordingly, this requires the use of higher concentrations of antiseptics and antibiotics, which must be effective against both bacterial and fungal microflora. Only 2 antiseptics have these properties - either 0.2% chlorhexidine or 0.1% hexetidine (0.1% Hexoral solution).
Examples of great mouthwashes are:
Important: most often, concomitant fungal flora with periodontitis occurs in the following categories of patients. For example, if your gum inflammation is long-term, chronic, or you smoke, or eat a lot of carbohydrates, or have concomitant chronic tonsillitis, or you have gastrointestinal diseases, or you have had at least 1 case of candidiasis in the past ( thrush) of any localization.
In all these cases, you should not use 0.05% chlorhexidine to rinse your mouth with periodontitis, but rather purchase a 0.2-0.25% chlorhexidine solution (in such concentrations it is highly effective, including against fungi of the genus Candida). Such concentrations of chlorhexidine are contained in rinses - Parodontax Extra, Lacalut Activ and PresiDent Professional. For more information about choosing agents for the treatment of periodontitis, read the articles at the links below.
→ The best mouth rinses for periodontitis, → Rating of the best gels for gums.
Systemic antibiotic therapy –
If you have periodontitis, you can’t just take and start drinking any antibiotic, because... it is necessary to take into account the nature of the microflora in periodontal pockets. There are 2 options here: either prescribe a broad-spectrum antibiotic, or first culture the contents of the periodontal pocket for microflora. However, culture is always recommended for patients with aggressive periodontitis and vertical type of bone resorption. For more information about the choice of antibiotics and their dosage regimens, read the article:
→ Choice of antibiotics for gum diseases
Sanitation of the oral cavity and depulpation of teeth –
In parallel with the removal of dental plaque and anti-inflammatory therapy, it is necessary to begin treatment of carious teeth and removal of decayed teeth. At this stage, temporary splinting of mobile teeth can be carried out, as well as restoration of missing teeth with a temporary removable denture (to urgently relieve the mobile teeth). In addition, a very important point is the need for tooth depulpation.
For example, it is necessary to remove nerves from teeth with deep periodontal pockets (having a depth of more than 1/2 the length of the root). It is ideal when, before filling the root canals in these teeth, the “copper-calcium depophoresis” technique is also performed, but it is advisable to do such a procedure only in those teeth that have mobility. This allows you to disinfect all microscopic branches of the root canals inhabited by pathogenic bacteria. The combination of “depulp removal + depophoresis” can significantly reduce tooth mobility (provided that the traumatic bite is also neutralized).
Everything we said above is only basic treatment. Depending on the specific clinical situation in the oral cavity, other methods of treating periodontitis may be used. This may include splinting mobile teeth with fiberglass, surgical techniques (curettage and flap operations), the manufacture of temporary and permanent dentures, as well as selective grinding of teeth.
Splinting for periodontitis –
Splinting of mobile teeth is usually carried out in the presence of their mobility. This technique allows you to strengthen your teeth, quickly reduce inflammation, and also stop the progression of bone tissue destruction around these teeth. Splinting can be temporary or permanent, and can be done using fiberglass or artificial crowns “soldered” together. In Fig. 12-14 you can see the beginning of the splinting process, and the fiberglass tape laid on the lingual surface of the lower teeth (later it will be covered with a light composite).
Read about the features of this method and its cost in the article: → Splinting of mobile teeth for periodontitis
Surgical treatment of periodontitis –
It must be said that this is one of the most important methods used in the complex therapy of periodontitis, the use of which can really stop the progression of this disease. There are several methods of surgical treatment, which include open curettage, as well as flap operations. The purpose of surgical intervention is to remove all dental plaque from under the gums, clean out all inflammatory granulations (which form at the site of destroyed bone tissue), and ultimately eliminate periodontal pockets.
Such operations are performed by dental surgeons specializing in periodontics. The operations are complex and require diligence and skill from the doctor, so there are very few good specialists in this field. In Fig. 15-16 you can see a fragment of the open curettage operation. The gum is detached from the teeth, the edge of the bone tissue is slightly exposed, the inflammatory granulations have already been cleaned out, but the deep periodontal pocket in the canine area is clearly visible (which in the second photo is filled with osteoplastic material, which will partially restore the bone level).
Read more about this treatment method in our article: → Curettage for periodontitis
Prosthetics for periodontitis –
Orthopedic treatment of periodontitis is carried out in those patients who have missing teeth, or the method of splinting mobile teeth using artificial crowns has been chosen. This stage of treatment is essentially the final one (not counting subsequent periodic maintenance therapy), and the prognosis of the teeth will largely depend on it. The goal of the orthopedic stage of treatment is to restore the chewing efficiency of the dentition, reduce the chewing load on weakened teeth, thereby preventing displacement, protrusion or fan-shaped divergence of teeth.
As we said above, prosthetics can be temporary or permanent. Temporary prosthetics with a removable denture are necessary when a large group of teeth is missing. Such a prosthesis will reduce the load on the remaining teeth, increase the effectiveness of anti-inflammatory therapy, reduce tooth mobility, and also stop bone destruction. In addition, if curettage or flap surgery is planned, then ignoring the need for temporary prosthetics in such a situation can only lead to an increase in tooth mobility, as well as to stimulation of horizontal bone resorption in the operation area.
Gums are bleeding - contact a periodontist
If you notice the slightest symptoms of periodontitis, immediately go to the doctor. The first sign is regular bleeding of the gums after mechanical impact.
If there is a single bleeding, there is no reason for serious concern: to strengthen the gums, you can change the toothpaste to a special product for the treatment and prevention of periodontitis, or use a strengthening gel or balm. But if bleeding becomes regular, you need to see a specialist.
If the disease progresses, some teeth may need to be removed. Therefore, the earlier the diagnosis is made and treatment is started, the greater the chances of completely getting rid of periodontitis without negative consequences.
Symptoms
- Inflammation of the gums;
- hyperemia (redness) of the mucous membrane, swelling, reaction to temperature stimuli;
- sore gums;
- discomfort, bleeding gums when chewing, oral hygiene;
- detachment of the gum from the tooth wall;
- formation of periodontal pockets;
- abundant plaque and tartar around the tooth;
- pus from the gums;
- loosening of the gum edge;
- exposure of tooth roots;
- tooth mobility;
- inflammation of the submandibular lymph nodes
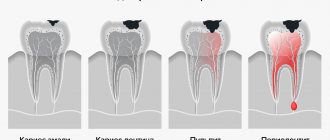
Symptoms of periodontitis vary depending on the extent of the inflammatory process. The more severe the stage of the disease, the more pronounced the symptoms. The disease does not occur suddenly; the early stage of periodontitis is catarrhal gingivitis - inflammation of the gums, not accompanied by a violation of the integrity of the mucous membrane.
Acute and chronic periodontitis: symptoms and treatment
As mentioned, the treatment plan will depend on the severity of the inflammation and how widely it has spread. Periodontitis affecting a few teeth is localized; periodontitis affecting most (or all) teeth is generalized.
Acute periodontitis, which has pronounced symptoms, occurs less frequently than chronic periodontitis and usually affects one or two teeth. It is often caused by trauma to the tooth or periodontal tissue, or improper installation of a crown or filling. This type of disease often occurs aggressively, causing rapid destruction of bone and muscle tissue.
If the pathology is chronic, then phases of exacerbation are replaced by phases of remission. At the same time, chronic periodontitis slowly and steadily progresses from the initial stage to the severe one. This form of pathology can be caused by both local factors (for example, trauma to the oral cavity) and general ones.
Classification
Periodontitis is classified according to location, nature of the course, and severity.
According to the nature of the flow
There are acute and chronic forms. In the first situation, the signs of periodontitis are pronounced, the gums are loose, bleed, and hurt. If the patient does not consult a doctor or ineffective treatment is prescribed, the disease takes a chronic course. In the chronic form, the symptoms are smoothed out, there are no acute signs of inflammation, but the consequences are more severe. Chronic pathology is characterized by periodic exacerbations, when the symptoms become pronounced.
By localization
According to the distribution of the pathological process, periodontitis is divided into:
- Localized
(focal) - occurs in a small area, in the area of 1 or several teeth. - Generalized
periodontitis is inflammation of all or most teeth in a row.
The symptoms of localized and generalized forms of the disease are no different, the only difference is in the number of teeth around which the pathological process has spread.
Degrees of periodontitis
- Mild
– fiber disintegration of the compact plate, reduction of the interalveolar septum to 1/3 of the length of the tooth root, signs of osteoporosis, slight tooth mobility, periodontal pockets of 2.5-3.5 mm. - Medium
– the depth of periodontal pockets increases to 5 mm, moderate tooth mobility is observed (grades I-II), bone atrophy around the teeth reaches 1/2 of the roots. Exposure of the necks and roots of the teeth or inflammatory growth of the gums occurs, abscesses (abscesses in the gums) can form. The teeth begin to “diverge” under chewing pressure, and the gingival margin becomes deformed. This is especially noticeable in the area of the front incisors. The gums bleed when chewing or brushing teeth, the necks of the teeth are exposed, and react painfully to temperature stimuli. - Severe
– symptoms increase, exacerbations of chronic periodontitis in adults are accompanied by the formation of abscesses, severe swelling of the gums, and pain. The depth of periodontal pockets reaches 6 mm, right up to the root apex. The interdental spaces increase, there is strong tooth mobility (II-III degrees), bone resorption, up to complete resorption of the alveolar septum.
Depending on the individual characteristics of the body, the disease progresses differently. Aggressive forms of periodontitis are characterized by rapid, almost rapid destruction of periodontal tissue, loosening of teeth, and their painless loss. In another part of patients, the disease progresses slowly, with occasional exacerbations, and long remission.
The most severe form is necrotizing periodontitis.
, in which the gum tissue stops receiving nutrition, blood circulation in them stops, and necrosis of the periodontium, periodontal ligaments, and alveolar bone occurs. This form of the disease occurs in patients with severe immunodeficiency conditions (AIDS, DiGeorge syndrome, SCID, etc.).
Professional hygiene for effective treatment of periodontitis
In the vast majority of cases, the development of this disease is associated with insufficient oral hygiene. The periodontal tissues become inflamed due to extensive dental plaque, so the first thing to do to treat periodontitis is a professional cleaning.
This procedure includes the following steps:
- removal of dental plaque
- polishing the tooth surface
- treating the tooth with protective varnish.
Modern cleaning methods are gentle on the enamel and cause minimal discomfort. Also, at the stage of removing tartar and plaque, preparations should begin for the treatment of caries and the removal of hopelessly affected teeth.
Is it possible to eliminate periodontitis with a laser?
Laser treatment of periodontitis is one of the most effective and minimally invasive ways to combat the disease, which is one of the stages of complex treatment. The laser has cleansing and antibacterial properties. During the procedure, each periodontal pocket is treated for a certain time, sufficient for the laser light beam to destroy pathogenic bacteria. The procedure is bloodless and virtually painless. However, a good effect can only be obtained with an integrated approach to the treatment of periodontitis.
Drug treatment of periodontitis
The next stage of treatment is to relieve inflammation and eliminate bleeding gums to prevent further development of the disease. This goal is achieved through drug therapy.
Medicines for the treatment of periodontitis are divided into local and general:
- local remedies are used to treat the affected areas. This includes rinses, antiseptic solutions, anti-inflammatory gels and balms. Local treatments also include therapeutic and prophylactic toothpastes, which can be used as an addition to the main therapy;
- general drugs, which are combinations of antibiotics in the form of tablets or intramuscular injections.
Non-invasive treatment for periodontitis may also include physical therapy. Auxiliary procedures using laser or electrophoresis will help eliminate inflammation faster.
Splinting procedure for periodontitis
The need for splinting in the treatment of periodontitis arises when there is mobility of more than 2-3 dental units in a row. Splinting helps strengthen teeth and also helps to quickly eliminate inflammatory processes in soft tissues.
Splinting can be carried out in different ways. A specialist can use fiberglass tapes in manipulations, install welded dental crowns or a clasp denture. The method of splinting is selected based on the clinical picture of a particular case.
Surgical methods
Treating periodontitis surgically is the most radical method. But in the later stages of the disease, it is necessary to eliminate periodontal pockets and remove non-viable teeth. This can only be done surgically.
The degree of intervention depends on the severity of the pathology. In some cases, a positive result can be achieved by simply depulping the tooth to remove pathogenic bacteria. The procedure for splinting teeth (connecting mobile teeth with adjacent teeth to ensure immobility) and other methods is also used.
A separate stage of surgical treatment is prosthetics. This is done to restore the functionality of the dentition, distribute the chewing load evenly, and prevent displacement and further loss of teeth. In some cases, a temporary prosthesis can be used to quickly unload the chewing surfaces and eliminate mobility during the recovery phase.
Diagnostics
- Taking anamnesis;
- dental examination with measurement of the depth of periodontal pockets (periodontogram);
- orthopantomogram (OPTG), CT;
- rheoparodontography (assess the tone of blood vessels);
- Schiller-Pisarev test;
- microbiological studies (PCR);
- blood tests (general, sugar).
Differential diagnosis of periodontitis is carried out with gingivitis, eosinophilic granuloma of the jaw, periodontal changes in Lefebvre-Papillon syndrome. What examination methods will be required depends on the form and severity of the disease.
Treatment and prevention of periodontitis at home
After successful treatment of periodontitis, it is necessary to pay increased attention to oral hygiene. To do this you should:
- Visit your dentist regularly to remove plaque and tartar;
- eliminate caries and fill dental canals at the slightest manifestation of pathological processes;
- use hygiene products designed to prevent gum disease;
- After each meal, use dental floss and mouthwash with an antiseptic;
- follow other rules for the prevention of periodontitis.
Is it possible to treat at home?
Decoctions of medicinal herbs (tricolor violet, calendula, lingonberry leaf, calamus, oak bark) will help relieve symptoms of acute inflammation. But no amount of rinsing will get rid of supragingival, and especially subgingival dental plaque. Only professional hygienic cleaning at the dentist's office can handle this. Folk remedies in the form of formulations of hydrogen peroxide, soda and lemon will only aggravate the situation. But maintaining the condition of your gums after treatment at home is not only possible, but also necessary. The dentist will give you all the necessary recommendations on how to treat periodontitis at home.
Asepta Parodontal - specialized products for the treatment of periodontitis
has developed a whole range of drugs for the treatment and prevention of gum disease. It includes:
- Asepta therapeutic and prophylactic toothpaste, which helps eliminate inflammation and bleeding of the gums. Contains a unique complex of medicinal extracts and active ingredients;
- Asepta Sensitive toothpaste for sensitive teeth. Provides gentle care for sensitive enamel and gums prone to inflammatory processes. Thermal mud in the paste helps heal damaged tissue and relieve irritation;
- Asepta mouthwash is intended to relieve symptoms of gingivitis, periodontitis, stomatitis and toothache caused by infection. The antimicrobial components of the drug help relieve inflammation and pain, and also have an antiseptic effect;
- Asepta Fresh mouthwash eliminates inflammation and bleeding of gums, prevents the formation of dental plaque, and also gets rid of pathogenic bacteria that cause bad breath;
- Asepta gel with propolis has an intense anti-inflammatory effect, reducing the sensitivity of enamel and promoting the healing of trophic ulcers. Effectively strengthens periodontal tissues and is suitable for patients of all ages.
- The adhesive balm in this series eliminates the causes and symptoms of inflammatory diseases of the mouth. The sticky base ensures a longer and more effective effect of the drug, allowing it to remain on the gums for a long time;
- Asepta vitamin and mineral complex contains all the necessary substances and active components for healthy teeth and gums.
Take care of your health with professional hygiene products!
What consequences can untreated periodontitis lead to?
Loss of teeth
The advanced stage of the disease destroys the soft and hard tissues around the teeth, which leads to their loss.
Deterioration of conditions for implantation
As mentioned earlier, with severe periodontitis, the volume of the jaw bone is significantly reduced, which makes it difficult to install implants, requiring preliminary bone growth, and in extremely severe cases makes implantation impossible.
The occurrence of other diseases
Periodontitis contributes to diseases of the gastrointestinal tract, diseases of the lungs, heart and even the formation of blood clots.
Clinical researches
According to the results of the clinical use of the Asepta line of products: the examined patients, already at the first follow-up examination (after 1-2 days) of using the Asepta line of products, showed a decrease in complaints of discomfort in the gums. On examination, hyperemia and bleeding of the gingival papillae are noted. On the 7th day, complaints of gum bleeding persisted in a minority of patients.
Upon examination, a decrease in hyperemia and swelling of the gums was noted, but bleeding persisted upon probing. On day 14, 2 patients continued to complain of bleeding gums when brushing their teeth; upon examination, a significant decrease in hyperemia and swelling of the gums was noted. After the final application of the gel with propolis, normalization of clinical manifestations was revealed, which is manifested by the absence of bleeding during brushing and probing.
Improved dynamics of indicators allows us to recommend the Asepta line of products for the local treatment of inflammatory periodontal diseases.
Sources:
- Clinical experience in using the Asepta series of products Fuchs Elena Ivanovna Assistant of the Department of Therapeutic and Pediatric Dentistry State Budgetary Educational Institution of Higher Professional Education Ryazan State Medical University named after Academician I.P. Pavlova of the Ministry of Health and Social Development of the Russian Federation (GBOU VPO RyazSMU Ministry of Health and Social Development of Russia)
- The use of adhesive balm "Asepta®" in the treatment of inflammatory periodontal diseases L.Yu. OREKHOVA*, Dr. med. Sciences, Professor, Head of Department V.V. CHPP**, Dr. med. Sciences, Professor, Head of Department S.B. ULITOVSKY*, Dr. med. Sciences, Professor A.A. LEONTIEV*, dentist A.A. DOMORAD**, O.M. YAKOVLEV** SPbSMU named after. acad. I.P. Pavlova, St. Petersburg - *Department of Therapeutic Dentistry, **Department of Microbiology
- The use of new anti-inflammatory drugs in the complex of therapeutic and preventive measures for periodontal diseases (E.D. Kuchumova, A.A. Leontyev, O.V. Kalinina, L.Yu. Orekhova, S.B. Ulitovsky) E.D. Kuchumova, Ph.D., Associate Professor, A.A. Leontyev, dentist, O.V. Kalinina, dentist, L.Yu. Orekhova, Doctor of Medical Sciences, Professor, Head of Department, S.B. Ulitovsky, Doctor of Medical Sciences, Prof. Department of Therapeutic Dentistry of St. Petersburg State Medical University named after. acad. I.P. Pavlova
- Article “Treatment and hygiene features for mild and moderate periodontitis” by S.B. Ulitovsky head Department of PFS, Professor, Doctor of Medical Sciences, A.A. Leontyev Associate Professor of the Department of PFS, Ph.D. PSPbSMU named after. I.P. Pavlova
- Evaluation of the effectiveness of treatment of chronic generalized periodontitis of mild and moderate severity using Asepta antibacterial agents (S.I. Gazhva, A.I. Voronina) S.I. Gazhva, Doctor of Medical Sciences, Prof., Head of Department A.I. Voronina, aspirant, dentist, Department of Dentistry, Faculty of Dentistry, State Educational Institution of Higher Professional Education "Nizhny Novgorod State Medical Academy"
- Study of the clinical effectiveness of treatment and prophylactic agents of the Asepta line in the treatment of inflammatory periodontal diseases (A.I. Grudyanov, I.Yu. Aleksandrovskaya, V.Yu. Korzunina) A.I. GRUDYANOV, Doctor of Medical Sciences, Prof., Head of Department I.Yu. ALEXANDROVSKAYA, Ph.D. V.Yu. KORZUNINA, asp. Department of Periodontology, Central Research Institute of Dentistry and Maxillofacial Surgery, Rosmedtekhnologii, Moscow
Introduction
The information world is very huge. Each of us is haunted by a million points of view
for any problem in any field of knowledge, you just need to ask a search query. The same thing happens in medical circles on the Internet - discussions of health problems are widely represented by both patients and doctors and often reach the point of absurdity:
For example, in questions:
- loosening of the tooth,
- exposure of the neck of the tooth,
- why are my gums and teeth exposed?
that is, in situations where the gums on a tooth have receded, patients are always confused: they have periodontal disease
, then suddenly it changed to
periodontitis
, then periodontal disease returned again. And the search for an answer to the question becomes endless.
The problem of “how to treat periodontal disease” is picked up by doctors who only add fuel to the fire by recommending medications and even folk remedies for periodontal disease, without having sufficient competence to do so.
Let's consider these points of view professionally, and try to convey one simple truth, which for the vast majority of patients (and even some doctors) will be a revelation: the diagnosis of periodontal disease of the gums
» —
does not exist
.
An expert point of view is expressed by the famous periodontist, Doctor of Medical Sciences Laura Mikhailovna Tebloeva:
As a rule, for patients who come to me and say: “I have periodontal disease,” I always clarify - did you make this diagnosis yourself or did you see a doctor? Often patients answer that they have this information from their doctor. It turns out that the patient did not read somewhere and determine the diagnosis of “periodontal disease” for himself, but, unfortunately, such a diagnosis was made by a doctor.
Antibiotics and antiseptics
Pathogenic microorganisms are not the main cause of periodontal disease, but their vital activity indirectly contributes to its development - it is no coincidence that a significant proportion of patients suffering from this disease exhibit one or another degree of decreased immunity. Accumulating in enlarged periodontal pockets and interdental spaces, the bacterial mass can cause inflammation, which in normal cases is not characteristic of this disease. That is why, in case of periodontal disease, it is often recommended to use various agents that can destroy pathogenic microflora and reduce the risk of secondary infection.
In the most severe cases, antibiotics in the form of capsules or tablets are used for this purpose, such as doxycycline and metronidazole, trichopolum, lincomycin. Broad-spectrum antibiotics effectively suppress the activity of microflora and contribute to the rapid elimination of inflammatory and infectious manifestations that complicate the course of the disease. However, long-term use of antibiotics is undesirable due to side effects and suppressive effects on the natural microflora of the body. They can only be used as prescribed by a doctor.
For a more gentle disinfecting effect, it is recommended to use rinses, gels, sprays and other external products containing antiseptics. In particular, the antibacterial rinse ASEPTA, which contains benzydamine and chlorhexidine. The adhesive balm ASEPTA, which contains metronidazole and chlorhexidine, thanks to its sticky base, is retained on the gums for a long time and has a long-term healing effect. Extracts of sage, witch hazel, chamomile, as well as xylitol, which are part of the ASEPTA Fresh mouthwash, also have a mild antiseptic and anti-inflammatory effect.
Vitamins and minerals
To restore damaged tissues, the body needs a wide variety of nutrients, which are not always contained in the required quantities in the daily diet. That is why the drug treatment regimen for periodontal disease often includes taking vitamin complexes. The best effect can be achieved by taking special complexes, for example, the vitamin-mineral complex for teeth ASEPTA.
The ASEPTA complex includes a whole range of substances necessary to strengthen gums and teeth. Vitamin C strengthens the walls of capillaries and blood vessels, helping to improve blood circulation in the gums, disruption of which is one of the main causes of periodontal disease. Vitamins B3 and B6 help reduce gum sensitivity, strengthen bone tissue and promote healthy mucous membranes. Vitamin A is involved in all metabolic processes occurring inside the body and increases protection against inflammatory and infectious diseases that often accompany periodontal disease.
In addition to vitamins, the complex also contains green tea extract - a natural component that has an antimicrobial effect, eliminates unpleasant odors, and slows down the aging process of tissues. An equally important component of the complex is coenzyme Q10, a substance that is a rich source of energy for the growth and restoration of cellular structures. Taking coenzyme promotes accelerated regeneration of damaged gums.
The complex also includes substances intended to strengthen the hard parts of the tooth, which are subject to increased stress during periodontal disease - coral calcium, which is well absorbed by the body, and vitamin D3, necessary for the proper absorption of calcium and phosphorus.
Question answer
Is periodontal disease inherited?
Yes, this is a chronic disease that can be inherited and be asymptomatic, destroying tissue, but without causing discomfort to the patient.
Is periodontal disease transmitted through kissing?
No, this is not a contagious disease that cannot be contracted through airborne droplets, through shared utensils, kissing, etc. This is a systemic disease that causes disruption of internal organs and is not transmitted from person to person.
Should teeth be removed if there is periodontal disease?
When the disease reaches an advanced stage, the dentist prescribes treatment in the form of strengthening the gums, building tissue, stimulating regeneration and blood circulation. Removal is carried out in the absence of alternative treatment methods.
Is there bad breath?
Yes, when interdental spaces appear, food particles get into them, which serve as a breeding ground for the development of bacteria that cause an unpleasant odor.
Prevention
Is it possible to avoid inflammation in periodontal tissues? Of course, and in most cases, careful hygiene and regular professional cleaning at the dentist are sufficient for prevention. It is also worth eating more solid foods - fresh vegetables, fruits, nuts. Such food gives the gums the necessary chewing load, promotes self-cleaning of teeth and supplies the body with valuable microelements. However, an additional course of dietary supplements containing calcium, fluoride and vitamin B will also not be superfluous. And of course, you shouldn’t put off correcting your bite, replacing missing teeth and treating caries. Then the likelihood of developing chronic periodontitis will be minimal.
Periodontal disease is a degenerative process of periodontal tissue due to deterioration of blood supply
The reason for the development of periodontal disease is a lack of blood supply to the periodontium, sometimes combined with cardiovascular and endocrine diseases. Blood delivers nutrients to all organs, therefore, with a lack of blood supply, the process of tissue degeneration begins.
with periodontal disease, bone decreases throughout the entire jaw, in contrast to periodontitis, which can also be local in nature
Periodontal disease develops very slowly and causes almost no trouble. The gums are pale, tightly cover the teeth and do not bleed; over time, the roots gradually become exposed, but the teeth can remain stable for quite a long time. Teeth are rarely affected by caries, and non-carious lesions (wedge-shaped defects and enamel erosion) are more common.