What is endodontics
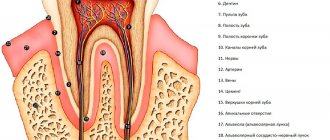
Endodontics is the treatment of the root canals of teeth. It is one of the most difficult in dentistry, because it requires experience and precision. The process involves cleaning the dental canals with diseased or dead pulp. The painstaking work of a dentist is aimed at preserving the functional characteristics of teeth and their aesthetically attractive appearance.
The need for treatment is due to the fact that inflammation occurs in the soft tissues of the tooth and severe pain appears. Over time, the process develops into a chronic stage. The patient no longer feels pain, but the inflammation is becoming increasingly widespread, penetrating deeply into the nerve and jawbone.
Who is an endodontist and what does he do?
This specialist treats root canals and cysts neurosurgically, using an operating microscope. This equipment makes it possible to diagnose the condition of the canals and carry out treatment, while ensuring extreme accuracy.
A dentist-endodontist (or endodontist) is a rather narrow specialization, so a dentist-therapist has the right to perform his functions. But for this he must have the necessary qualifications. Compliance with this requirement is of great importance, since the endodontist must be able to carry out various manipulations with the pulp and root canals. Also, this specialist must have an impressive theoretical base and be extremely attentive. Any mistake during the procedure can lead to tissue infection and tooth loss.
Good to know. To become a specialist in endodontics, you must obtain an additional three-year education at a medical university.
Medical Internet conferences
Apical foramen rupture. Excessive expansion of the apical foramen as a complication is more common in teeth with straight, well-passable canals. With this complication, the physiological apical constriction is destroyed by an endodontic instrument [17]. With this medical error, it is impossible to form an apical stop. This kind of complication can be caused by incorrect determination of the working length, loss of working length during canal expansion, incorrect tactics for treating the apical part of the canal, the doctor’s lack of an apex locator, and lack of diagnostic X-ray diagnostics, especially in the case of resorption of the root apex during periodontitis [18]. Prevention of this complication is the mandatory conduct of diagnostic radiography of the teeth before treatment, accurate determination of the working length and its correction during the passage of curved root canals using an apex locator, strict adherence to instrumental processing of the canal in its apical part without excessive apical pressure, the formation of an apical stop during mechanical and machine expansion method. In this situation, it is necessary to create an “artificial apical narrowing.” To do this, use a tool two numbers larger than the tool that was incorrectly processed to the specified working length [12].
Instrument breakage in the canal is a common and difficult to correct complication that occurs as a result of non-compliance with instrumentation technology. In practice, there have been cases of breaking off a pulp extractor during root pulp extirpation, breaking off canal expanders (K-reamer, K-file, N-file) during the passage and expansion of a root canal, breaking off a machine endodontic instrument when working with an endomotor, breaking off a canal filler when filling a root canal [ 14]. Breaks of an endodontic instrument occur as a result of violation of the sequence of its use, non-compliance with rotation angles, the application of excessive force when working with an instrument in a canal, working with a low-quality deformed instrument, refusal to use EDTA and working with files in a dry canal. The use of EDTA, regular irrigation of the root canal and removal of dentinal filings from its lumen contributes to easier and unhindered advancement of the endodontic instrument in the canal. The use of a flexible nickel-titanium alloy in endodontics has reduced the risk of this type of complication, but has not eliminated it [13]. When working with such an instrument, it is necessary to monitor the degree of wear and clearly control the number of sterilizations performed. It is necessary to cull endodontic instruments: monitor damage to the cutting surface, unwinding of the spiral, the sharpness of the blade of the working part, as evidenced by deformation of the instrument, violation of the rotation of the spiral, damage and shine of the cutting edge. It should be remembered that pulp extractors and instruments of ISO size 10 and smaller are disposable and must be disposed of after a single use. Instrument breakage in the canal gives the largest number of unfavorable prognoses for endodontic treatment. Removing the instrument from the apical and middle part of the root canal is almost impossible. If a periapical inflammatory process occurs, the teeth of the lower jaw must be removed. In the upper jaw, under favorable anatomical conditions, it is possible to eliminate the inflammatory process by performing surgical operations (resection of the root apex, hemessection of the root). Removal of the canal filler from the canal is possible if it is broken off at the mouth of the canal and there is extensive access. Prevention of this type of complication is consistent careful work in the root canal using high-quality instruments [15].
The final stage of endodontic treatment is high-quality sealed obturation of the root canal. A common complication in the treatment of complicated forms of caries is poor-quality root canal filling. This includes incomplete obturation and removal of material beyond the root apex. Incomplete filling of the root canal can occur as a result of incorrect determination of the working length, insufficient expansion of the canal, errors in the technique of filling it, incorrect selection of the size of the filler (gutta-percha pin), or if the size of the canal filler does not correspond to the diameter of the canal lumen. Knowledge and mastery of filling techniques is of great importance. Filling a canal with gutta-percha is effective only with adequate obturation of the apical foramen; for this it is necessary to create an apical stop and a taper of the canal corresponding to the diameter and taper of the pin. In practice, these conditions are not always strictly fulfilled by doctors. It has now been established that filling the canal with one paste does not lead to complete obturation due to delayed shrinkage of the material, the formation of voids in the root canal and rapid resorption of the material if it is not mixed correctly and there is moisture in the root canal. In cases of incomplete or partial obturation of the root canal, post-filling pain may occur immediately or in the next 3-5 days with an increasing effect. Against this background, a chronic inflammatory process occurs at the root apex, which requires repeated endodontic intervention; its result is not always favorable [6]. During endodontic treatment, during canal filling, the filling material is often removed beyond the apex of the tooth root (possibly removed into the periodontium, into the bone tissue, into the surrounding soft tissue, into the mandibular canal, into the maxillary sinus). This error can occur as a result of careless work of the doctor during canal treatment: incorrect determination of the working length of the tooth, lack of apical stop, excessive expansion of the apical foramen, excessive pressure on the filling material, lack of skills in filling root canals, use of a mechanical canal filler at high speed. When the filling material is removed beyond the root apex, post-filling pain is often observed, which can be of various types (spontaneous pain, pain when biting, intense neuralgic pain) [18]. To prevent this complication, the doctor needs theoretical training, knowledge of the anatomical and topographical features of the structure of the root canals of the teeth, provision of the doctor’s workplace with the necessary tools and equipment at all stages of endodontic treatment, the presence of practical skills and abilities of the doctor, compliance with the algorithm and sequence of endodontic manipulations. Currently, the method of obturation of root canals with gutta-percha has an advantage (method of one pin, lateral condensation, three-dimensional obturation of the canal with hot gutta-percha, combined method). When using gutta-percha, it is necessary to strictly dose the amount of sealer and use a small amount of pastes [19]. Prevention of complications during filling is compliance with root canal filling techniques in accordance with modern requirements for endodontic treatment, mastering and improving the skills of doctors in three-dimensional obturation of the root canals of teeth with gutta-percha [20-22].
When to start treatment
The patient should contact a specialist if the following symptoms occur:
- severe aching pain in the tooth;
- there were difficulties with chewing;
- teeth become sensitive to heat and cold;
- tooth color has changed;
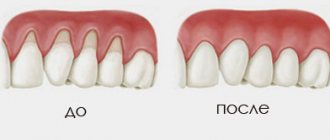
- swelling of the gums occurred.
It is important to know. The use of modern techniques and drugs makes it possible to treat impassable canals and save teeth that need to be removed.
Patients must undergo treatment:
- with pulpitis, deep caries;
- periodontitis, periostitis (flux);
- the presence of inflammation in the root region;
- preparation for prosthetics;
- replacing old fillings;
- injuries that lead to tooth damage and the formation of large cavities.
You can make an appointment with an endodontist at the Saint-Dent Clinic in Moscow. The clinic has modern equipment; innovative techniques are used in the provision of dental services. You can find out the cost of treatment here, the clinic’s contacts are posted here.
Errors in identifying root canal orifices
Causes:
- insufficient knowledge of the topography of root canals;
- Features of endodontic anatomy.
To detect the mouths of root canals, a sharp angled probe, optical devices, and dyes are used. It is often difficult to find additional canals at the bottom of the tooth cavity, but sometimes the entrance to the canal is not identified due to ignorance of the anatomy. The fourth canal in teeth 16, 26, 17, 27 is usually located in the center of the main mesiobuccal canal and is sometimes connected to the main canal. The second canal in teeth 31, 41, 32, 42 is localized on the lingual side of the main canal. To detect it, it is necessary to expand the entrance to the cavity towards the neck of the tooth. In lower jaw teeth 34, 44 with two canals, one canal is located on the buccal side, the other on the lingual side. In teeth with three canals, one canal is located on the lingual side, the other two on the buccal side. If the additional channel remains undetected, the treatment prognosis worsens. The fourth canal in teeth 36 and 46 is located next to the main distal canal; it can be identified by the oval opening of the distal canal, elongated in the lingual-buccal direction.
Preparation for endodontic treatment
After examining the diseased tooth, the endodontist will prescribe an x-ray. The next stage is endodontic preparation for the upcoming procedure. It consists of filling carious cavities that are not endodontic entrances and treating periodontitis. The specialist must find out from the patient whether he has an allergy to anesthetics and other contraindications.
The preparation process also involves ensuring asepsis of the root canal during the preparation process. To do this, a rubber dam is installed and the working field is disinfected.
Discussion
Diagnostics is one of the main stages in medicine and dentistry in general, and in endodontics in particular. Indeed, an appropriate treatment plan cannot be determined without an accurate diagnosis and a thorough preliminary examination of the clinical case; This is the only way to deal with surprises in the best possible way (6). Endodontic anatomy is especially important for clinicians, so an optimal diagnostic approach, convenient accessible technology and high skill are necessary for the successful location, preparation, disinfection and filling of the root canal system (7). These days, however, when planning treatment, the endodontist can count on much greater safety and accuracy of diagnostic instruments than in the past.
Sequence of endodontic dental treatment
- Introduction of anesthesia. Additionally, you can use a special spray for local treatment.
- Drilling out the cavity.
- Depulpation (nerve removal). It is usually removed in one procedure. But if the patient has contraindications for anesthesia, the doctor applies a devitalizing arsenic paste and places a temporary filling, which needs to be treated for several days. During this time, the nerve dies and only after this is it removed.
- Treatment and cleaning of canals, removal of pulp residues. If there is an inflammatory process, medicine is placed inside the canals and a temporary filling is placed. After 3-7 days, you need to re-visit the endodontist and, if necessary, repeat the canal treatment.
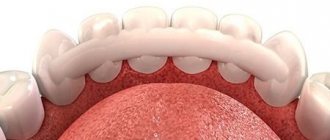
- Canal filling with gutta-percha.
- Restoration of the coronal part using filling material or prosthetic structure.
Perforation of the bottom or wall of the tooth
During mechanical treatment of the tooth cavity in the process of searching and expanding the mouths of the root canals, perforation of the bottom or wall of the tooth often occurs. The reasons for the development of these complications:
- poor knowledge of the topography of the dental cavity,
- insufficient opening of the tooth cavity,
- incorrect choice of tool and violation of the methodology for its use,
- excessive expansion of the orifices.
Perforation at the level of the tooth neck (sub- or supragingival) usually occurs due to poor visibility with insufficient opening of the tooth cavity and preparation without taking into account the inclination of the tooth. Perforation of the bottom of the tooth cavity occurs when excessive preparation with a bur during the search for the mouths of the root canals. This is especially the case when re-treating a tooth previously treated with the resorcinol-formalin method, since the search for the mouths of the canals is complicated by the changed color and structure of the dentin of the bottom of the tooth cavity. The prerequisites for the occurrence of perforations of the bottom and walls of the tooth cavity are:
- displacement of the tooth axis in the lingual or buccal direction;
- reduction in the height of the tooth crown due to significant abrasion of the chewing surface or deposition of a large amount of replacement dentin;
- endodontic treatment of a tooth through an artificial crown.
Clinically, perforations of the bottom or walls of the tooth manifest themselves in the form of a characteristic “sinking” of the instrument, bleeding and a sharp pain in the patient during treatment without anesthesia. Touching the site of a fresh perforation with a probe also causes acute pain. In case of doubt, an x-ray is taken with the inserted gutta-percha pin or file. It should be emphasized that when treating perforations of the bottom of the tooth cavity, the most important factors are the localization of the perforation and the time elapsed from its formation to closure. The best prognosis is observed in cases where the perforation is closed immediately, which minimizes trauma and infection of surrounding tissues. In addition, the size of the perforation is an important factor. Effective filling of perforations is possible with small sizes (1-2 mm). With perforations of significant size, the filling material is inevitably pushed out into the periodontal tissue in combination with infection, as a result of which chronic destructive forms of periodontitis often develop.
The most unfavorable localization of perforation is in the area of root furcation. Almost any perforation in this area leads to periodontal destruction. Perforation of the wall of the tooth cavity in most cases does not pose a problem when filling with modern matrix systems and filling materials. To close perforations, silver amalgam and glass ionomer cements, which have optimal biocompatibility with tooth tissues, are widely used. An important advantage of these materials is the absence of the stage of etching of hard tissues, high adhesion to dentin and tooth cement, moisture resistance and the ability to long-term release of fluorides.
When identifying perforation, it is important to locate the mouth of the canal, and if it cannot be found, then you should not simply fill the perforation, since in the future you will have to remove either the root or the tooth. When channels are found, they are cleaned and expanded. The tooth cavity and canals are washed with sodium hypochlorite solution. The canals are temporarily filled with calcium hydroxide and large size files No. 30 or 35 are inserted into each canal so that it obstructs the orifice. The perforation is closed using modern matrix systems and biocompatible filling materials, which are introduced into the cavity in small portions and compacted with light movements. It should be noted that the material should not be removed into the periodontium, since otherwise a process may develop in the tissues leading to the destruction of the supporting apparatus of the tooth. After the material has hardened, the files are removed from the canal and the tooth cavity is closed with a light-curing temporary material.
Currently, one of the most effective new materials used in the treatment of perforation of the bottom of the tooth cavity and root canals is a mineral trioxide aggregate or MTA (MTA), developed in the USA at Loma Linda University more than 10 years ago. The MTA material is biocompatible with periodontal tissues and is perceived by them as an inert substance, similar to bone tissue; in addition, it is radiopaque due to the content of bismuth oxide. MTA is used for direct dental pulp coating, endodontic treatment of teeth with incomplete root growth, filling of tooth perforations, retrograde filling during root apex resection surgery, as well as for apexification in wide roots. It is currently produced by Dentsplay under the name Pro Root: it comes with one packet of powder, which consists of small hydrophilic particles of calcium oxide and silicon dioxide and a capsule with water in the amount necessary for optimal mixing with the powder. When moistened, this powder turns into a gel, which then hardens to create an impenetrable barrier. MTA hardens within 4-6 hours even in the presence of moisture. To optimize the process of applying the material to the desired area of the tooth, special applicators (endodontic or surgical) can be used. Method of using ProRoot. The contents of the Pro Root sachet are poured onto a mixing pad, the capsule with water is opened and mixed with the powder. If the mixture turns out thick, you can add 1-2 drops of distilled water. Pro Root material is applied with a special tool to the perforation area, then compacted with a plugger, a moistened swab is inserted into the tooth cavity and covered with a temporary light-curing filling material. Excess material is removed with an excavator. After Pro Root has hardened, at the next visit, we begin filling the canals or cavity of the tooth. In case of ineffective filling or the development of chronic destructive forms of periodontitis in combination with the removal of filling material or a metal fragment into the periodontium, surgical treatment is necessary. In this case, both traditional surgical methods of treatment (hemisection, coronary-radicular separation, deliberate replantation) and tooth-preserving methods of sealing perforations can be performed, depending on the level of preserved bone.
Possible complications
- swelling of the gums in the area of the diseased tooth;
- feeling of discomfort, severe pain;
- perforation of the tooth root wall;
- poor canal filling;
- root fracture.
The main cause of complications is poor-quality filling and the inability to monitor the intermediate results of treatment. The attitude of patients towards their health is also of great importance; if they do not follow the doctor’s recommendations, the risk of complications increases. In modern clinics, microscopes are used during endodontic treatment, thanks to which it is possible to significantly improve the quality and predictability of treatment.
annotation
Anatomical abnormalities of the root canal system are common in endodontic practice and present a challenge that must be approached with skill and care, beginning with a thorough diagnostic phase and consideration of the most appropriate treatment plan. Fortunately, significant progress has been made in endodontics due to technological advances and the development of instruments with greater efficiency that now allow even very complex cases to be treated with relative ease. Below, along with the description of several cases in which patients, due to the peculiar morphology of the tooth, had numerous difficulties, which were successfully overcome thanks to the use of modern instruments and the consolidation of clinical experience in this field, the characteristic features of the latest progress in endodontics are described.
Key words: complex endodontic treatment, endodontic anatomy, endodontic diagnostics, nickel-titanium instruments, tooth morphology.
Advice and recommendations from a specialist after treatment
- Immediately after the procedure, it is not recommended to eat hard and tough foods, too hot and cold dishes.
- During the first days, while brushing your teeth, the treated area should not be touched.
- Moderate toothache may continue for 48 hours; painkillers must be taken to relieve it. If after 48 hours the pain in the tooth does not subside or swelling appears, you must come for a consultation with an endodontist.
- In order to keep your teeth healthy for as long as possible, you need to visit a dental hygienist 2-4 times a year to remove tartar and plaque.