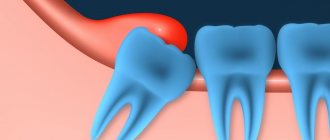
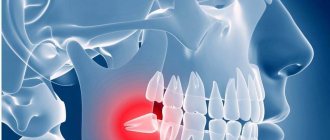
Pericoronitis is an inflammation of the soft tissues surrounding the crown of a partially erupted tooth. It affects the gums, tissues around the tooth and can spread to the immediate environment. The most typical place for pericoronitis to occur is wisdom teeth, third molars. Not only do they erupt later than everyone else (and sometimes do not appear above the surface at all), but they also have a special structure. A long stay in a “sleeping” form, the influence of neighboring teeth change the position of the third molar, and it begins to erupt sideways, at an angle, further damaging the gum from the inside, which provokes pericoronitis of the wisdom tooth.
Causes and factors contributing to the occurrence of pericoronitis
Inflammation of the mucous membrane and gums above the wisdom tooth, as well as associated with the formation of the so-called hood - folds of the mucous membrane - is the main cause of the disease. Pieces of food accumulate inside this hood, which are a good substrate for the growth of pathogenic bacteria. The combination of inflammation due to tooth eruption (often long, difficult, with injuries to the mucous membranes) and the hood with altered microflora leads to the formation of a focus of infection in this place.
Other common causes of pericoronitis
- Gingivitis and periodontitis as background processes for the formation of inflammation, the formation of a periodontal pocket, in which bacteria also accumulate. After this, the process moves on to the surrounding tissue.
- Local injuries. A typical phenomenon: an incorrectly filled or partially broken tooth digs into the gum opposite or next to it, constantly injuring it. This leads to inflammation. Sometimes pericoronitis occurs in people wearing orthodontic appliances, which can injure the mucous membrane.
- Polyodontia, or teeth in excess of a set.
What to do if you have a bad breath
The principles of treating halitosis are based on the causes of its occurrence. If the source of bad breath is a source of infection or a carious cavity, the unpleasant symptom will disappear after a course of professional hygiene with the removal of supragingival and subgingival dental plaque, treatment of caries, removal of decayed teeth that cannot be restored by orthopedic methods.
Antiseptic solutions will help deal with the problem faster. Rinsing your mouth with an antiseptic inhibits the growth of pathogenic microorganisms and prevents relapse of inflammation. The rinse is selected based on the dentist’s recommendations. The doctor will decide how to treat bad breath after a comprehensive diagnosis.
If the root cause of halitosis is an inflammatory-infectious process of the gums and oral mucosa, local treatment with antibacterial, antiviral, and antifungal drugs is prescribed. Combined products contain components to relieve itching, redness, burning, pain, and eliminate unpleasant odor. In case of severe inflammation, systemic antibiotic therapy, immunomodulators, and vitamins are prescribed. In situations where halitosis is caused by installed orthodontic or orthopedic structures, measures are taken to correct and replace them. Or they select an alternative method of prosthetics and bite correction.
Symptoms of the disease
Symptoms of pericoronitis depend on the intensity and severity of the inflammatory process and the patient’s physical health. Signs of the disease can also be constant or periodically subside and be replaced by other complaints.
Possible general symptoms:
- Pain. It can intensify when you press on the source of inflammation, or it can be constant, pronounced or low-intensity. Sometimes it radiates to the ear, throat, nose, jaw.
- Redness or redness with an area of whitish skin.
- Swelling around the pericoronitis area.
- Unpleasant odor that gets worse after a night's sleep.
- Change in the taste of food, the appearance of a taste of blood or pus.
- Formation of a purulent sac on the gum.
- Difficulty opening the mouth, talking, chewing.
- Increased body temperature.
- General malaise.
- Difficulty sleeping.
- Enlargement of the cheek due to swelling of the jaw.
When is it time to sound the alarm? Symptoms and stages of tooth decay
There are a number of signs that should alert you. Having noticed one or two of them, a person should become concerned and see a specialist. This:
- 1. Accumulation of plaque on tooth enamel. Barely noticeable yellowish spots.
- 2. Bad breath, even the smell of rotten breath. With severe caries, the smell will be very noticeable.
- 3. Dark spots on the enamel. Painful sensations when eating hot or cold, sweet foods.
- 4. If you ignore the above-mentioned manifestations of ill health, the situation gets worse. Next, black areas appear in the area of the neck of the tooth or on the root itself, but the latter can only be detected during an X-ray examination.
- 5. Frequent aching painful sensations appear, and even if you regularly rinse your mouth with herbal infusions and take painkillers, the destructive processes are in full swing.
- 6. The pain intensifies (especially when a stream of cold air hits the tooth), and the pulp begins to die.
- 7. The nerve bundle is affected, the pain becomes especially severe.
- 8. Then, if the person never went to the hospital, he notices with surprise and relief that the pain goes away. However, in reality, the inflammatory process does not stop - the disease spreads to the root area.
The course of the disease in different types of pericoronitis
Pericoronitis is divided into acute and chronic. Acute begins, as a rule, suddenly, is accompanied by inflammation of varying degrees of intensity, which affects the dental hood, spreads to surrounding tissues and, with severe inflammation, can cause complications from the body. This type of pericoronitis can occur as catarrhal and purulent.
In the case of catarrhal type, the disease occurs at normal body temperature and general satisfactory condition. Patients complain of pain when chewing or biting in the area of an erupting molar (or other cause of pericoronitis). With a long-term process, the lymph nodes under the lower jaw may become enlarged and painful.
If you look at the affected tooth, you can see that the hood or edge of the gum is red, there is swelling, in which the erupting tooth sometimes appears. Touching the source of inflammation is very painful, and when you press on it, serous fluid may be released. This form responds well to treatment. If the catarrhal form is not treated, then the inflammation can turn into a purulent form of acute pericoronitis.
In the purulent form of acute pericoronitis, the condition and well-being quickly deteriorate, the temperature rises to 38 ° C, the general condition, sleep, and appetite suffer. The pain becomes constant and severe. It radiates into the ear, into the back of the head, into the temple. Due to significant swelling, it becomes painful to swallow, open your mouth, and talk. The submandibular lymph nodes enlarge, sometimes so much that it becomes difficult to turn or tilt the head.
When you try to examine the source of inflammation, you can see that not only the hood of the wisdom tooth is swollen, but also the gums around the tooth. The swelling can also cover the inner surface of the cheek, the palate, and can spread all the way to the entrance to the oropharynx. If you touch this hood, the patient will experience sharp pain, and pus will be released from the lesion, sometimes smelling bad. Purulent pericoronitis responds well to treatment, however, it is possible that in an advanced case or with improperly selected treatment, the purulent process spreads to the jaw with the formation of phlegmon [1].
Chronic pericoronitis occurs if the acute one was not noticed, the inflammation on its own or with the help of medications went away or subsided. But since the actual cause is not eliminated, it periodically worsens and produces symptoms.
Most often, the process occurs at normal body temperature and satisfactory general condition. In this case, there is an aching, constant, rather pronounced pain, which can interfere with chewing and talking. Enlarged, mobile, painful submandibular lymph nodes can interfere with head movements. Soreness can radiate to the ear, temple, jaw, and throat. An unpleasant odor appears from the mouth; touching the area of inflammation with the tongue or accidentally pressing it is painful. If you look at the area of inflammation, you can see that the gums above the hood begin to lag behind the tooth. Chronic pericoronitis requires treatment. Otherwise, complications may develop, including the formation of ulcers and phlegmon.
Three ways to check if you have bad breath
- Lick your wrist and smell it. This is what the front part of the tongue smells like, and at the root of the tongue the “aroma” is usually much more intense.
- Take a spoon, lick it a few times and smell it. There will be saliva on it and it will smell just like your breath.
- Exhale into the mirror and immediately inhale deeply through your nose. The smell that you smelled is felt by others when communicating with you.
If your breath is bad, contact your dentist for help. Your doctor will help you find out the cause of bad breath and get rid of it.
Treatment of pericoronitis
Treatment of pericoronitis has several tasks:
- Eliminate pain.
- Combating the pathological process, preventing its further spread and preventing complications.
Typically, both acute and chronic pericoronitis are treated on an outpatient basis [1]. Elimination of pain is carried out simultaneously with the fight against acute inflammation. In case of catarrhal form, the doctor cleans and treats the gums and hood with an antiseptic and applies a special bandage, which simultaneously treats with medicinal impregnation and lifts the hood [1]. In this way, conditions are created for the process to subside and, if necessary, for the eruption of the third molar.
For purulent pericoronitis, surgical treatment may be required, which is also carried out in a dental clinic. The hood is excised, the wound is treated with special therapeutic bandages and the resulting pocket is lifted so that it does not again begin to interfere with the tooth and does not provoke inflammation.
Anti-inflammatory drugs, antihistamines and antibiotics may be prescribed. After the pain has subsided and the inflammation has subsided, the dentist evaluates the possibility of saving the tooth or the need to remove it. For this purpose, a complex of studies is carried out, including examination, laboratory tests, and x-rays. Based on the results of this examination, the tooth is either removed or given the opportunity and “space” to erupt.
After your wisdom tooth is removed, you will need to come back the next day for an examination.
This will allow you to assess the condition of the hole and mucosa. If the tooth is saved, it will need to be shown to a doctor once every 6 months. Clinical guidelines (treatment protocols) for the diagnosis of pericoronitis [1]
How to get rid of bad breath
Halitosis is not masked by the scent of bubble gum or mint candy. To get rid of an unpleasant odor, you need to reduce the number of bacteria. This can be done only by removing tartar and plaque.
How to eliminate bad breath
- Use floss and irrigator to clean the interdental spaces.
- Use a special brush to clean your tongue, paying special attention to its root.
- Drink at least 2 liters of clean water per day.
- Visit your dentist regularly.
- Once every six months, undergo a professional hygiene procedure.
If you urgently need to freshen your breath, you can use special rinses or infusions of peppermint, string and cumin. There are also aerosol fresheners and special lollipops. True, the effect will be temporary and the smell will return very quickly.
Recommendations for patients
If an incision or excision of the hood was performed in the treatment of pericoronitis, it will be necessary to follow several preparatory and postoperative measures that will speed up healing and reduce the risk of complications.
- For two to three hours after the intervention, do not take food, hot drinks, or alcoholic drinks.
- On the day of the operation, do not go to the bathhouse, sauna, take a hot bath, or be in the sun or in a hot room.
- Limit physical activity the day before and on the day of treatment.
- During these days and the next three days, it is recommended to follow a diet, exclude alcohol, spicy, very hot foods.
- Before the intervention, you should not eat foods with a strong smell.
- Smokers should quit cigarettes the day before the hood excision, on the day of surgery, and two days after.
- For sanitation (cleaning and disinfection), you can use a mouth rinse with antiseptic solutions.
- After the intervention, the doctor will prescribe medications that accelerate healing.
- Do not apply warm compresses or ointments containing bee, snake, etc. venom.
- If after excision of the hood or placement of therapeutic turundas there is pain, severe swelling, increased discomfort, pain in the area of the submandibular lymph nodes, you need to consult a doctor to identify the cause and take action.
Why does the smell appear?
A putrid odor accompanies the destruction of tooth tissue. It can be triggered by various reasons, but all of them can be divided into two large groups: medical error and poor oral hygiene.
The most common medical errors:
- Installing a crown with a small gap. Visually, such a gap is usually invisible, but food debris easily penetrates through it under the crown. There they begin to rot, causing an unpleasant odor. The rotting mass is a favorable environment for the proliferation of microorganisms. They begin to develop quickly, which further aggravates the problem and can cause an inflammatory process.
- Incorrect installation of the crown or use of low-quality materials. The crown is fixed with dental cement. High-quality material has a long service life. But when the clinic uses low-quality consumables, the cement gradually crumbles. The prosthetic structure loses the necessary tightness, gaps appear, and the crown begins to wobble. Food debris clogged into the cavity begins to rot and creates a favorable environment for the proliferation of bacteria. It’s easy to avoid such a problem - get prosthetics done in a good clinic. Our dentistry employs experienced doctors and dental technicians, and we use high-quality consumables. Therefore, the likelihood of cement destruction and depressurization of the structure is reduced to almost zero.
- Oxidation of metal elements of the crown. Such problems arise when using cermets. The metal frame begins to oxidize, and the resulting oxides affect the supporting tooth. As a result of chemical reactions, the tooth is destroyed. All these processes are accompanied by a smell and an unpleasant taste in the mouth.
- Installing a crown on a weak tooth. The supporting tooth on which the crown is installed must be healthy. The weak one will continue to deteriorate under the prosthesis. Rotting processes are accompanied by an unpleasant odor.
When contacting the ARDC clinic, you do not have to worry about medical errors. Before prosthetics, you will be given a full examination and diagnosis. A strong support will be selected to install the crown. Weak units are removed. If necessary, the doctor will recommend implantation and install the implant in place of the extracted tooth.
The tooth is ground down for the crown, so during the period when the dentures are made, it remains unprotected. To avoid destruction after grinding, temporary prostheses are installed in our clinic. These are inexpensive acrylic structures that allow you to lead a normal lifestyle. This approach reduces the risk of developing secondary deep caries under the crown.
Poor hygiene can lead to dire consequences. After prosthetics, the doctor gives recommendations on caring for the oral cavity, implants, and dentures. The dentist will recommend you a suitable toothbrush and toothpaste, and special devices that will allow you to thoroughly remove plaque.
Dentistry for those who love to smile
+7
Make an appointment