Introduction
It is known that facial prostheses, such as ear prosthetics, made of wax, were used in ancient Egypt.
The first historical evidence of the use of facial prostheses dates back to the sixteenth century: the French surgeon Ambroise Paré describes the first artificial nose made of gold, silver and papier-mâché, which was attached to the face using a headband. In the second half of the 19th century, Claude Martin put forward the idea of creating an immediate denture using the tissues of the upper and lower jaws as a matrix to create complex structures. In the 20th century, with the advent of silicone materials, the quality and realism of craniofacial prostheses improved significantly, but the problem of fixation, which affects the appearance, function of the prosthesis, and patient comfort, was not completely solved. With increasing aesthetic demands, traditional fixation methods such as adhesives, pockets, loops and glasses have become unacceptable. In 1997, Brånemark installed the first bone-anchored extraoral hearing aid implant, and in 1979 the bone-anchored ear prosthetic implant. These events changed the entire concept of maxillofacial prosthetics. Since then, extraoral bone implants have been widely used to support prosthetic eyes, ears, and noses. Their use partially solves the problems of discoloration and deterioration of the prosthetic material, since these problems are often associated with adhesive materials. The skin and mucous membranes are less irritated by the mechanical effects of permanent fixatives and the chemical effects of adhesives and solvents. Implant-retained craniofacial prostheses have improved significantly from an aesthetic point of view due to their ease of installation, as well as thinner edges that blend in color with the skin. A large number of scientific and clinical studies confirm the success of their use and note an improvement in the quality of life of patients. Facial injuries and mutilations, especially after radical surgery, often lead not only to external physical disabilities, but also to functional and psychological disorders. In such cases, maxillofacial surgeons and dental prosthetists have to carry out a whole range of rehabilitation procedures. The options for reconstructive plastic surgery are often limited due to unfavorable conditions, such as damage to the vascular system of the surgical site due to radiation therapy, or insufficient volume of residual soft and hard tissue. In such cases, rehabilitation of patients with severe craniofacial defects is carried out with the help of prostheses, which represent an acceptable solution from an aesthetic point of view. A facial prosthesis is created by a craniofacial surgeon, maxillofacial orthopedist and prosthetic technologist as a good alternative to reconstructive surgery. To replace missing hard and soft facial tissues, prostheses using extraoral implants with a ball abutment, a bar design, or a choice of magnetic abutment are used. The shape of the prosthetic nose, eyes and ears, its color and texture should, as far as possible, be indistinguishable from the surrounding natural tissues. Rehabilitation can only be successful when patients are able to appear in public without attracting unwanted attention. Extraoral implants have many advantages in correcting facial defects over both adhesive prostheses and spectacle-mounted prostheses. They are characterized by ease of fixation of the prosthesis, which ensures the ability to properly install the prosthesis, thereby promoting comfort and confidence in its use. There is no skin irritation from the adhesive, and there is no need to wash off the adhesive every time after using the prosthesis. A thinner denture can be made, with thinner edges that blend into the skin, improving the overall appearance. During preoperative planning, when meeting with the patient, specialists from various fields not only show him the options for prostheses, but also teach him how to care for the abutment and prosthesis.
Implants have played a critical role in improving patient acceptance of facial prostheses. Patients enjoy the safety, comfort, and convenience of implant-supported dentures—benefits previously unattainable with older fixation methods. Over time, surgeons have noted a decrease in the number of patients requiring multiple complex surgical procedures. When correcting large defects, a combined approach combining tissue grafting and prosthetics using implants is recommended to achieve optimal results.
A three-implant facial prosthesis is the preferred method of replacing missing hard and soft orofacial tissue. Fixation on extraoral implants stimulates more confident behavior of the patient in public. Multidisciplinary treatment will require the combined efforts of several specialists. If we are talking about a defect in the eye socket, then the efforts of an ophthalmologist, a craniofacial surgeon, a maxillofacial orthopedist and a prosthetic technician are required.
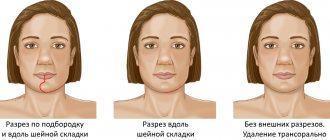
Midface defects can be divided into two broad categories: midline midface defects, which include the nose and/or upper lip, and lateral facial defects, which include the cheeks and orbit.
The choice between plastic surgery and a prosthesis for serious facial injuries remains difficult and depends on the area and etiology of the damage, as well as on the wishes of the patient. The development and use of extraoral implants for the correction of facial defects has to some extent changed the attitude of patients towards facial prostheses. Implants provide comfortable donning and reliable fastening of the prosthesis, which improves the perception of the prosthesis by patients.
We will conduct a retrospective review of patients who underwent facial prosthetic reconstruction from 2005 to 2010. Clinical reports describe step by step the materials and methods used, including the implant procedure.
There are three main diagnoses that require surgical intervention: oncological, traumatological and genetic and/or acquired diseases. The goals of surgical and prosthetic rehabilitation are to replace missing hard and soft facial structures, restore physical impairments, alleviate social problems and improve quality of life.
Treatment protocol
Treatment of a patient with oral cancer or after trauma is a collaborative effort between craniofacial surgeons, oncologists, radiation therapists, and prosthetic technicians.
Typically, immediately after radical surgery, a free tissue graft is performed to restore both soft and bone tissue. A large percentage of patients receive 4 to 6 weeks of radiation therapy after surgery. The total radiation dose to the tumor bed depends on the presence or absence of cancer cells at the surgical margin of the tumor. The radiation dose usually does not exceed 55 Gy, for cases with a clear pathological margin, and from 65 to 70 Gy, with a narrow pathological margin. Radiation localizers are widely used, and radiation fields are adjusted in such a way as to minimize the possibility of large salivary glands entering the area of exposure to large doses of radiation; however, intensity-modulated radiation therapy was not used. Radiation dose to bone can often be minimized in areas where implants are to be placed. Approximately 6 weeks after radical surgery, the patient was expected to undergo radiation therapy for 5 to 7 weeks. Once the patient had recovered from plastic surgery and radiation therapy, new standard prostheses were made. The implants were planned to be placed 4-6 weeks after plastic surgery, depending on the need for post-operative radiation therapy. All implants were placed based on wound healing from osteotomy and recovery from radiation therapy. Three implants were installed. The implants were installed in the existing native bone tissue and/or in the free vascularized bone tissue of the reconstructed mandible. During the operation, before installing the implants, excess plate segments were removed to connect the bone fragments.
Prosthetic options include classically anchored dentures, then implants with ball-shaped attachments, bar structures and magnets.
The long-term prognosis is important, but having a high-quality prosthesis for even a year or two can significantly improve a patient's quality of life. The advantage of installing implants and facial prostheses is that the perfect stability of the prosthesis guarantees the patient's return to social life.
Nasal prosthesis
Clinical report
A 63-year-old woman diagnosed with recurrent basal cell carcinoma of the nose was treated.
After nasal amputation, external beam radiation therapy and chemotherapy were performed. Oncological treatment was completely completed in 2007. Surgical restoration and installation of the prosthesis began a year after the end of treatment (Fig. 1, 2). Three extraoral implants were inserted along the edge of the postoperative defect. The operation was performed under general anesthesia with nasopharyngeal intubation. The main implant bed for the nasal prosthesis was a pear-shaped ridge at the base of the nose (2 implants - left and right). The other bed was the glabella; we paid special attention to the degree of pneumatization of the frontal sinus and the amount of overlying bone tissue. The operation lasted 65 minutes and went without complications. The wound healed without inflammation. Lincomycin (600 mg orally) was used as an accompanying antibiotic. Four days after the operation, the patient was discharged in good condition. Six months after the installation of the implant and the end of the healing period, prosthetics began. A control tomogram was performed. Magnetic mounts were inserted. The prosthesis was prepared as follows. A one-stage prosthetic technology was used; a nasal prosthesis with separately located abutments and magnetic fixation was chosen. It was investigated in which direction the protruding parts of the abutments are directed. It was required that the fixation elements be oriented so that the prosthesis would extend beyond the anterior edge of the maxillary bone. To achieve this and position the fixation components in a position that is easy to manipulate, cantilever abutments were chosen. An additional set of magnetic abutments was ordered to select the appropriate cantilever angle.
The defect impression is recorded as a partial alginate impression. A plaster model of the prosthetic element was made. Base wax was used to sculpt the edges of the acrylic resin base. The wax-up model was prepared, evaluated on the patient and brought to its final form.
The plaster mold is cast. The wax is melted out, and the surface of the plaster model and casting mold is coated with a release agent and auto-polymerizing acrylic plastic. Acrylic plastic is subjected to pressure treatment in a polymerizer. The shape of the prosthesis, its color and texture are finalized using special plastic. The finished prosthesis is ground and polished. A magnet is attached to the top of the support. An impression is made of the contact surface between the abutment and the fixture using single-phase silicone. Magnets connect to the abutments.
Figure 1. Nasal prosthesis: a) wax cast; b) polymerization; c) coloring; d) installation of magnets.
Figure 2. Nasal prosthesis: a) CT scan after installation of 3 implants, b) magnetic attachments; c) patient after rehabilitation.
Classification of maxillofacial apparatuses.
By function:
|
By design:
| By application method:
|
- Removable.
- Fixed.
- Combined.
Out-of-laboratory splints for the treatment of fractures.
Tigerstedt wire tires (proposed in 1916).
1. Smooth tire-bracket. (A)
2. Tire bracket with spacer
3. Tire with hook loops.
4. Tire with hook loops and an inclined plane.
Technique for making a Tigerstedt splint.
consists of an aluminum arc 1.5-2mm. It is fixed to the teeth using a ligature; bronze-aluminum wire is used as a ligature.
Tire Zbarzha.
Used to treat fractures of the upper jaw (anterior).
It consists of 1.5 mm aluminum wire, 75-80 cm long. The splint is adjusted to the dentition and fixed to the teeth with a bronze-aluminum ligature. The entire structure is attached to a head plaster cast.
Shina Vasilyeva.V.S.
Standard stainless steel belt tire with hook loops. It is fixed to the teeth using ligatures.
Shina Gordashnikova
Universal plastic dental splint with mushroom-shaped processes.
Sheena Marey.
For the treatment of fractures of the lower part. The teeth are tied together in pairs with a nylon ligature, the ligature is cut so that the ends remain, 4-5 mm long. Self-hardening plastic is placed into a pre-prepared aluminum groove (made of foil), greased from the inside with Vaseline, and the groove is pressed against the vestibular surface of the teeth. The ends of the ligatures enter the plastic and, thanks to them, the splint is fixed to the teeth.
Vasiliev G.A. proposed threading the fishing line into plastic beads and placing them on the vestibular surface of the teeth, which ensures a more rigid fixation of the splint on the teeth.
Weber tire.
Used for linear fractures without displacement, and for post-treatment of fractures, with a sufficient number of teeth on the fragments with sufficient height of the tooth crowns.
It consists of a wire frame (0.8 mm) with bridges in the area of premolars and molars. The frame is strengthened with a wax base (the lower border of the base does not reach the transition fold of 3 mm). The wax is replaced with plastic, and the ends of the jumpers are removed.
Vankevich modified the Weber splint, proposed to manufacture it for the high-grade area, added inclined planes to it for the treatment of low-level fractures with displaced fragments. This splint is used in combination with a chin sling.
Vankevich apparatus.
Vankevich modified the splint and proposed making it for the upper jaw by adding inclined planes to it for the treatment of fractures of the lower jaw with displaced fragments.
Brazed Limberg ring bus.
It is used when there is an insufficient number of teeth and when the crown part of the teeth is low.
It consists of stamped crowns or rings (usually for canines and first premolars) and a vestibular arch (wire 1.2-1.5 mm). Arcs are soldered with crowns. In case of vertical displacement of fragments, a splint is made for both jaws with hooking loops.
Ocular prosthesis
The absence of an eye may be a birth defect. Eye loss may also result from trauma, tumor, ophthalmia migrans, removal of a painful blind eye, or the need for histological confirmation of a suspected diagnosis. Eye diseases are relatively rare, but given the anatomy of the surrounding structures, they are very serious diseases. Tumors in the eye area account for 0.2 to 0.5% of the total. Tumors of the eye and adjacent organs manifest themselves in the following symptoms: dystopia, impaired mobility of the eyeball, exophthalmos and diplopia. Depending on the severity of the disease, surgery may follow one of the following three approaches: evisceration, enucleation, or exenteration. Evisceration
is a surgical operation during which the internal contents of the eyeball are removed, the sclera, Tenon's capsule, conjunctiva, external muscles of the eyeball and the optic nerve are preserved; the cornea of the eye can be preserved or excised.
Enucleation
is a surgical operation to remove the eyeball and part of the optic nerve from the socket.
Exenteration of the orbit
– this is the complete removal of the eye socket, often accompanied by partial or complete removal of the eyelids; produced primarily for malignant ocular tumors.
In particular, the diagnosis is made by an ophthalmologist; An examination by an otolaryngologist and a dentist is recommended. Radiation diagnostic methods are an integral part of the diagnostic procedure. They include radiography of the skull in frontal, semiaxial and lateral projections. In addition, ultrasound, computed tomography, and very often nuclear magnetic resonance imaging are used. In accordance with the details of the diagnosis, it is possible to accurately determine the extent of damage to the eye and surrounding structures of the orbit and choose a treatment method. In the treatment of solid tumors, radical surgery is used in most cases, despite the risk of functional and appearance defects.
Losing an eye is a disability that can lead to serious physical and emotional problems. Replacing a lost eye as quickly as possible is essential for the patient's physical and psychological recovery and helps improve the patient's perception of others.
Restoring facial defects using prosthetics improves the capabilities and level of self-esteem of patients. However, when using facial prostheses, difficulties may arise due to the moving tissue bed, the quality of fixation of the prostheses and reactions when interacting with adhesives. The use of extraoral implants in the craniofacial region reduces the limitations associated with the use of adhesives and is a treatment method with high long-term success. A three-implant facial prosthesis is the preferred method of replacing missing hard and soft orofacial tissue. The shape of the prosthesis, color and texture should, as far as possible, be indistinguishable from the surrounding natural tissues. Rehabilitation can only be successful when patients are able to appear in public without attracting unwanted attention. An important prerequisite for successful treatment of patients with such physical defects is healthy bone tissue at the edges of the defect. The following clinical report follows the step-by-step process of making an ocular prosthesis.
Clinical report
The patient, aged 21 years, was referred to the Clinic of Dentistry and Maxillofacial Surgery in Prague.
At age 2, he underwent surgery to remove retinoblastoma in his left eye. (Enucleation was followed by external beam radiation therapy and six cycles of chemotherapy (etoposide and cisplatin (cDDP). Cancer treatment was completed in 1983. Most cases of retinoblastoma are discovered in early childhood (80%), the incidence rate is 1:18,000 newborns The age of onset of the disease is mainly from 1 to 2 years. The etiology is unknown. A genetic predisposition associated with the Rb 1 mutation is possible.
The patient had no other chronic illnesses, was in good health, had no serious injuries, had suffered no illnesses other than common childhood illnesses during childhood, and had no allergies. The patient did not use a prosthetic eyeball and was very distressed by his injury. Routine preoperative examination was performed, as well as semiaxial cranial radiography and magnetic resonance imaging. According to the treatment plan, 3 implants were installed. After engraftment, the implants were equipped with ball attachments, and an ocular prosthesis was made with a system of clip fixation of males on matrices. The operation was performed under general anesthesia with nasopharyngeal intubation. In March 2004, 2 implants were implanted in the upper edge and 1 implant in the lower edge of the left orbit. The operation lasted 65 minutes and went without complications. The wound healed without an inflammatory process. Lincomycin (600 mg orally) was used as an accompanying antibiotic. On the fourth day after surgery, the patient was discharged in good condition. Six months after the installation of the implant and the recovery period, the production of the prosthesis began. A control semiaxial X-ray and magnetic resonance imaging study was performed. Three ball attachments were fixed to the implants. An impression of the anophthalmic orbit was then made using a standard impression tray specifically designed for orbital impressions (tray material: acrylic plastic). A working model was made, and a prefabricated plate with 3 male clips was also prepared.
Figure 3. Ocular prosthesis: a) CT scan before treatment; b) eye socket; c) installation of implants.
Figure 4. Ocular prosthesis: a) installation of implants, b) taking an impression; c) ball attachments and ocular prosthesis; d) prosthesis; e) patient after rehabilitation.
The wax-up model was prepared, evaluated on the patient and brought to its final form. The shape of the model corresponded to the contours of the eye socket and the configuration of the eyelids. After individualization, the manufacturing process of the prosthetic eye with the eyeball was completed. The shape of the prosthesis, color and texture should, as far as possible, be indistinguishable from the surrounding natural tissues. The finished prosthesis was ground and polished and inserted into the orbit of the eye. Glasses help to achieve a symmetrical position relative to the second eye and the face as a whole (Fig. 3, 4).
Chapter 2. Devices used in maxillofacial orthopedics. Classification.
Chapter 1. Subject of maxillofacial orthopedics. Goals and objectives of the subject. History of the subject. The role of domestic scientists in the development of this area of dentistry.
Indications and contraindications for reconstructive operations and the use of orthopedic treatment methods for congenital and acquired defects and deformities of the maxillofacial area.
Maxillofacial orthopedics
– a section of orthopedic dentistry, including the diagnosis and treatment of injuries to the maxillofacial area and their complications, congenital and acquired defects of soft and hard tissues of the maxillofacial area (MFA), the consequences of surgical interventions for wounds, inflammatory processes and neoplasms, as well as diseases of the temporomandibular joint (TMJ), masticatory muscles, etc.
Maxillofacial orthopedics is conventionally divided into maxillofacial prosthetics (replacement of dentofacial defects and elimination of deformations of the maxillofacial area with maximum aesthetic and functional effect) and maxillofacial traumatology (orthopedic methods of treating injuries of the maxillofacial area and their complications).
Despite the fact that the emergence of many innovative surgical techniques has partially replaced orthopedic methods of treatment, maxillofacial orthopedics still does not lose its relevance, and an integrated approach remains more effective than isolated surgical or orthopedic methods of treatment and rehabilitation of the above-mentioned group of patients.
Objectives of maxillofacial orthopedics:
1) orthopedic treatment of jaw fractures and their consequences; 2) elimination of deformations of the dentofacial system using orthopedic methods; 3) prosthetics for congenital and acquired defects of the face and jaws; 4) orthopedic measures for reconstructive surgery of the face and jaws; 5) orthopedic treatment of diseases of the masticatory muscles and temporomandibular joints.
Indications for orthopedic treatment methods
can be different, most often it is: the impossibility of performing surgical intervention due to the presence of contraindications or the patient’s refusal; ineffectiveness of surgical treatment methods; the use of orthopedic techniques as part of complex treatment or as temporary measures during the stages of surgical treatment.
Contraindications to restorative and reconstructive operations.
There are local and general contraindications.
Local include a minor degree of defect or deformation (in the absence of significant functional impairments and in cases where the cosmetic factor is not important, especially in elderly and senile people); facial skin pyoderma, ulcerative stomatitis, gingivitis, glossitis; inflammatory processes in the regional lymph nodes, maxillary sinuses, jaws, nose, nasal pharynx and other organs located adjacent to the operation site.
General contraindications include various acute and chronic infectious diseases; severe disorders of the digestive system; mental disorders; pustular lesions of the skin of the trunk, limbs and scalp; low-grade fever of unknown etiology; general malaise and poor health of the patient; reluctance of the patient (patient) or the child’s parents for the operation to be performed.
Presumably, the history of maxillofacial orthopedics goes back to ancient times. Even Hippocrates proposed the first similarities to a sling-shaped bandage for jaw fractures and the first methods of ligature binding of dentition. Also, attempts to immobilize jaw injuries with sling-shaped bandages and tying teeth were made by Cornelius Celsus (1st century AD) and Galen (2nd century AD).
In 1575, the first palatal obturator was described by the French surgeon Ambroise Paré. Pierre Fauchard, who improved Pare's obturator in 1730, also proposed a method of ligature binding of teeth on both sides of the fracture. In 1880, Kingsley proposed prosthetics to replace defects of the palate, nose and orbit. Claude Martin published publications in 1889 that laid the foundation for post-resection prosthetics.
In the USSR, maxillofacial orthopedics received its greatest development in the 40-60s of the 20th century, mainly by military surgeons. A significant contribution to the development of this specialty was the designs and techniques of A.A. Limberg, S.S. Tigerstedt, A.I. Betelman, I.M. Oksman, V.Yu. Kurlyandsky, Ya.M. Zbarzha, Z.Ya. Shura, B.K. Kostur, M.M. Vankevich, Z.N. Pomerantseva-Urbanskaya, V.A. Minyaeva, A.L. Grozovsky and others.
Chapter 2. Devices used in maxillofacial orthopedics. Classification.
Auricular prosthesis
Indications for autoplastic reconstruction of the auricle in comparison with a prosthesis with fixation on an extraoral implant were described in the work “Plastic and Reconstructive Surgery” in 1994. The choice between the two existing methods, autoplasty and prosthesis, depends more on the surgeon's training and tradition than on an analysis of the indications for a particular procedure in a specific clinical situation. For example, most children with microtia in the United States undergo plastic surgery. In Sweden, on the contrary, the same defect is corrected with the help of a prosthesis. Patients with post-traumatic defects of the auricle or after radical operations are usually adults. There are some differences between physical disabilities in adults and those in children. First, skin loss and scarring from trauma or previous surgery can make standard plastic reconstruction difficult. Second, the auricular tragus is often preserved in postoperative and trauma patients, which significantly improves the impression of the prosthesis. The presence of a tragus allows the leading edge of the prosthesis to be hidden, a great advantage in terms of appearance. It has long been noted that the area of the auricle is the most reliable place for an implant. All potential patients undergo a preoperative tomographic scan with radiographic stent markers installed. This procedure allows you to evaluate the intended implantation site in order to be able to maximize the length of the implant. In particularly difficult cases, the mastoid cells of the temporal bone make it difficult to select a site for implantation, and sometimes the choice has to be made again. There is no evidence that opening the mastoid cells during implant placement has a negative effect. If the bone is sufficient to ensure reliable fixation, the implant is left in the same place, otherwise, it is necessary to look for another area. Thickening of the bone along the edge is a feature favorable for implant placement. The use of three implants in the ear area reduces the need for hanging mounting and creates a tripod effect with mechanical strengthening. All implants are connected using a tissue beam structure, and fixation is achieved using clips.
Clinical report
The patient, a 45-year-old man, lost his left ear during a car accident and was referred for prosthetic replacement (Fig. 5, 6).
The patient received three implants in a two-stage surgical procedure. Titanium implants were inserted into the temporal bone using a gentle surgical technique, and once the implants had healed, it was possible to go deeper into the skin to create a non-contact channel. During the first stage of the procedure, implants were inserted into the bone tissue in the area of the craniofacial defect. Previously, bone thickness in the mastoid region was measured (minimum 6 mm) using a frontal, axial and three-dimensional model based on computed tomography scanning. Implantation was performed under general anesthesia. A 4 mm longitudinal incision was made behind the external auditory canal and the temporal bone was exposed. The estimated time for osseointegration of implants inserted into the temporal bone is 6 months. The second stage consisted of thinning the subcutaneous tissue, opening the implant and attaching the abutments to the implants. This procedure involved removing some of the subcutaneous tissue to minimize movement of the skin around the implant. Healing caps were placed on the abutments and wrapped in gauze soaked in ointment to improve skin-bone contact and prevent hematoma and swelling. The postoperative treatment plan included instructions for caring for the operated site. The sutures were removed after 10 days, and during this period the patient did not complain of pain or complications. Four weeks after the end of the second stage, the prosthesis was manufactured and attached to the implants. Fabrication of the implant-retained prosthesis began three weeks after attachment of the abutments, following routine clinical and laboratory procedures. Fixation was carried out using a beam structure with a clamp.
The auricle prosthesis was made according to the shape and size of the patient's healthy ear. A plaster model and image of the right ear were made, and a cast of the beam structure and auricle prosthesis was made. The wax-up model was prepared, evaluated on the patient and brought to its final form. The shape of the model corresponded to the contours and configuration of the ear. After individual selection, an ear prosthesis was made from silicone and acrylic plastic. The finished prosthesis was ground and polished. Hair helps to achieve a symmetrical position of the prosthesis relative to the face as a whole.
Figure 5. Auricular prosthesis: a) healthy ear; b) plaster model; c) calculation of the symmetrical position of the ears, d) polyester impression; e) beam structure with consoles, f) beam structure; g) preparation of the beam structure.
Figure 6. Auricular prosthesis: a) position of the future ear; b) production of a prosthesis; c) staining; d) beam structure with clamps; e) clamps; f) auricle prosthesis; g) patient after rehabilitation.
conclusions
Extraoral implants provide an effective treatment alternative for patients requiring facial prostheses.
Implants can help overcome many of the difficulties encountered when fixing large facial prostheses. Our data indicate a predicted high percentage of implant survival in the auricle area; pyriform/nasal region and orbital region. The following advantages of installing magnetic implants and facial prostheses can be noted. Optimal stability of the prosthesis guarantees the patient's return to social life. Three magnetic attachments are used in the design, placed in the jaw, glabella, etc. Extraoral implants provide a wider surface for osseointegration. Magnetic attachments provide better surface stability than ball-shaped attachments, and at the same time do not interfere with the patient or make handling of the prosthesis difficult. For auricular prostheses, a beam design is much more convenient due to the load from the surrounding muscles. Facial prostheses using three implants are the most preferred method of replacing missing hard and soft orofacial tissue. The shape of the prosthesis, color and texture should, as far as possible, be indistinguishable from the surrounding natural tissues. Rehabilitation can only be successful when patients are able to appear in public without attracting unwanted attention. The use of implant-retained dentures gives the patient confidence in social life.
Tatiana Dostalova (Charles University, 1st and 2nd Faculty of Medicine, Prague, Czech Republic), Jiri Kozak, Milan Hubacek, Jiri Golakowski, Pavel Kriz, Jakub Strnad and Michaela Seidlova
Medical Internet conferences
Relevance: Prosthetics for patients with acquired jaw defects is one of the most difficult tasks in dentistry. Due to the complexity of the relief of the prosthetic bed, and the variety of clinical cases, it is necessary to have a clear understanding of the technique of prosthetics for such defects and the design of dentoalveolar prostheses.
Goals and objectives : To become familiar with the technique of prosthetics for patients with acquired defects of the upper and lower jaws. As well as the design features of dentures.
Article: Prosthetic designs used to treat patients with jaw defects, depending on the topography of the defect of the face and jaws, are classified into intraoral dentofacial ones, as well as combined ones, combined with extraoral facial epitheses.
Orthopedic structures are divided into preoperative and postoperative (post-resection) jaw prostheses.
The designs of ectoprostheses used at different stages of prosthetics have significant design differences, which is associated with their functional purpose.
Goals and objectives of direct prosthetics:
— formation of the future prosthetic bed.
- prevention of the formation of keloid scars.
— reposition and fixation of the fragments of the lower jaw remaining after the operation.
- restoration of speech and chewing disorders.
- prevention of severe facial deformations and changes in appearance.
- awareness of the therapeutic and protective regime.
Technique of prosthetics for patients with jaw defects.
The existing principles of providing orthopedic dental care to patients with acquired jaw defects are based on the use of effective design solutions when creating prostheses and methods for their manufacture, and improved dental materials. This concept and model of complex rehabilitation is multi-stage and for almost every stage of treatment of patients with acquired defects of the upper or lower jaw requires the manufacture of several medical devices using special and auxiliary materials and technologies.
Design features of dentures.
Features of fixation.
The effectiveness of orthopedic treatment of patients with facial and jaw defects largely depends on the reliability of fixation of replacement prostheses, which is optimally ensured in the presence of teeth.
When choosing a design and planning treatment stages, you must:
— Make maximum use of remaining teeth, even mobile ones, by splinting them first.
— Take into account the conditions that have formed after surgical intervention, and to improve the fixation of the prosthesis, make maximum use of the retention properties of the alveolar processes, bone fragments, soft tissues, and cartilage that limit the defect.
In the early postoperative period, in the complete absence of teeth and difficult anatomical and topographic conditions of prosthetics, when it is impossible to achieve high-quality fixation of the structure using conservative methods, surgical methods are used to strengthen the disconnecting prostheses.
The number of fixing elements of a dentoalveolar prosthesis should increase as the volume of the structure increases.
Methods aimed at increasing retention and stabilization of dentures are very diverse. As a rule, clasps (retaining and support-retaining), artificial crowns, magnetic retainers, telescopic, locking and beam systems are used as fixing elements of dentures. It is especially important, taking into account the basics of biomechanics, to use indirect fixators (kipmakers), which protect the prosthetic structure from tipping over.
The correct choice of fixation method is determined not only by the fixation characteristics of the device, but also by the ability to redistribute functional loads, which reduces the risk of overloading the periodontal tissues of abutment teeth. The rational use of fixation methods, taking into account existing individual characteristics and anatomical conditions, ensures the restoration of the basic functions of the dental system, facial aesthetics and improvement of the psychological state of patients.
In the case of complete absence of teeth, the structure of the jaw prosthesis is fixed using the remaining anatomical formations. In most clinical cases, fixation of jaw prostheses in the complete absence of teeth is difficult and sometimes impossible, so it is advisable to use dental intraosseous or magnetic implants. Along with this, it is necessary to take into account that creating reliable fixation using artificial supports is not always possible in cancer patients, especially those who have received radiation therapy and chemotherapy, since relatively often they need surgical correction due to the progression of the underlying disease. In addition, the formation of scars and the loss of a large mass of the bone skeleton of the upper jaw do not always allow the use of dental implants in patients with defects of the upper jaw caused by trauma and benign neoplasms. In such cases, the obturating part of the jaw prosthesis can be used as a retainer.
Arutyunov A.S. in 2012, a model of the defect of the upper jaw with different thickness and compliance of the free edge of the mucous membrane of the prosthetic bed for the obturating part of the dentoalveolar prosthesis was proposed, the advantages of one or another configuration of the obturator holding the maxillary prosthesis on the upper jaw with partial and complete absence of teeth were determined. Based on the established dependence of the forces of insertion and removal of the obturator of the jaw prosthesis on the properties of the elastic base materials and in accordance with the individual characteristics of the geometry of the defect of the upper jaw, it is possible to calculate the optimal design parameters of the obturator. This approach makes it possible to design an obturator of a dentofacial prosthesis in the presence of teeth of the “lid” type, without penetrating into the space of the anastomosis between the oral and nasal cavities, and in the absence of teeth of the “plug” type, which increases the efficiency of the jaw prosthesis due to the optimal design parameters of the obturator.
This is especially effective when a rigid base polymer is combined in the design of a prosthesis with an elastic polymer of acrylic nature or a special silicone material.
Often, the clinical situation of a postoperative defect in the complete absence of teeth does not allow the use of obturators made of rigid structural materials due to the thinned mucous membrane lining the anastomosis, to ensure sufficient fixation of the structure of the maxillary prosthetic obturator on the upper jaw. To eliminate this problem, it is recommended to use a jaw prosthetic obturator, the base of which is made of a rigid material, and the full obturator is made of an elastic structural material.
This design allows for retention and stabilization of the jaw prosthetic obturator, taking into account the elasticity of the mucous membrane of the edge of the defect (fibrous ring of the anastomosis) of the upper jaw and the structural material of the obturator.
Along with this, to improve the fixation of jaw prostheses in the complete absence of teeth, the use of fixatives of a chemical nature is indicated - films, adhesive gels, powders that swell in the oral cavity and provide stickiness and adhesiveness, anti-inflammatory and wound-healing effects, capable of compensating for the lack of congruence between the inner surface of the prosthesis base and relief of the mucous membrane of the prosthetic bed. These products are widely used by patients with large plate dentures and complete absence of teeth.
In case of jaw defects, there is often a need for combined prosthetics, when fixed dentures are used to splint teeth and provide fixation of removable dentures.
Features of the manufacture of dentoalveolar and maxillary prostheses for both the lower and upper jaws are that at the first stage it is necessary to make a construction base (metal and plastic) with support-fixing elements, which is carefully fitted in the mouth and used in determining the central occlusion and positioning of teeth and checking the design of the prosthesis. This approach makes it possible to facilitate clinical stages and accurately adjust the boundaries of the prosthesis, especially in the area of scar tissue.
However, in a number of cases, experienced orthopedic dentists make dentures without the fitting stage, if there are antagonizing pairs of teeth that make it possible to fix the height of the lower part of the face and the position of the lower jaw in the usual occlusion.
The objectives of maxillofacial prosthetics, the choice of a replacement structure and the planning of prosthetic features are determined by the volume of surgical intervention:
- on the upper jaw - during resection of the alveolar process, unilateral and bilateral resection of the body of the upper jaw.
- on the lower jaw - during resection of the alveolar part, the chin with loss of continuity of the bone, while maintaining the continuity of its body, half of the jaw and its complete removal.
Prosthetics of defects of the upper jaw.
Resection of the alveolar process, one- and two-sided resection of the body of the upper jaw are the main surgical interventions on the upper jaw, leading to the formation of defects of the same name.
Before taking an impression of the upper jaw, which has an oronasal anastomosis, it is necessary to replace the defect with a long gauze swab, previously soaked in a glycerin mixture. The tampon is placed sequentially in continuous layers, taking into account the remaining anatomical formations, and carefully so as not to push it into the nasopharynx, the defect is completely isolated. With a correctly placed tampon, the impression material does not penetrate into the undercuts of the nasal cavity and maxillary sinus. Otherwise, when removing the impression, part of the impression mass may come off, it may be retained in the niches formed after surgical intervention, which subsequently threatens inflammation, the etiology of which doctors do not immediately and not always recognize. Sometimes only surgical revision allows one to identify the cause of inflammation and stop it.
Using a thermoplastic mass, a standard tray is adapted to the oral cavity, active and passive movements are used, and the edge of the impression is formed along the border of the transitional fold and in the area of the defect. The spoon is inserted into the mouth and pressed all the way to the jaw. Active and passive movements are used to form the edge of the impression along the border of the transitional fold and in the area of the defect. The spoon is removed until the mass has completely hardened and the outer gauze is removed. An impression mass is applied to the surface of the preliminary impression, covered with an inner layer of gauze. The spoon is inserted into the mouth and pressed against the jaw. After structuring the impression mass, the impression is removed from the oral cavity and a plaster model is made from it, on which the areas to be isolated, as well as the remaining teeth, are covered with adhesive plaster or lead foil. If the model has a complex defect relief, then use a parallelometer to fill in the undercut areas. An individual spoon is prepared according to traditional methods
An individual spoon is fitted, the edges are formed with thermoplastic mass. Functional tests are performed under the pressure of the forces of the masticatory muscles and under the supervision of a physician. The impression is made using impression material. After its structuring, the impression is removed from the oral cavity along with a tampon, a fragment of which connected to the impression is cut off. The remaining part of the tampon is removed with tweezers. The upper jaw defect is washed with an antiseptic solution.
There is another method of taking an impression, when the alginate impression mass is applied to a standard tray and then covered with two layers of gauze. The tray is placed on the upper jaw and, after structuring the impression mass, removed from the oral cavity. Despite the simplicity of the method, the orthopedic dentist must have extensive experience in order to avoid the complications described above.
Arutyunov proposed a method for obtaining an anatomical impression with an alginate mass using a standard spoon, according to which a plaster model is made. An obturator is modeled on it by lining the positive image of the palate defect with wax while simultaneously modeling the resected alveolar ridge. The resulting composition is placed in the oral cavity and adjusted by filling any gaps with wax. An impression is obtained from which an individual spoon is made. The resulting spoon is adapted to the oral cavity using functional tests. Retention metal staples are installed in a wax obturator fixed in the jaw defect. A corrective layer of silicone impression mass is applied to the resulting composition, after which an impression is obtained using a previously made individual tray with a base layer of the same mass added to it.
Prosthetics for mandibular defects.
The effectiveness of prosthetics for patients with acquired defects of the lower jaw largely depends on the etiology, topography and extent of the defect in the lower jaw, as well as changes in the mucous membrane.
In the modern world, the approach to replacing defects of the lower jaw has changed significantly. Successfully performed osteoplastic operations make it possible to obtain an optimal prosthetic bed for prosthetics.
However, traditional orthopedic treatment of patients with dentures with polymer bases is not always effective, this is due to the occurrence of functional overloads of the tissues of the prosthetic bed when biting and chewing food. The load falls through the artificial teeth onto the base or frame of the prosthesis, which leads to the appearance of a deflection zone under the saddle or base. In the zone of concentrated load, tension occurs not only in the soft tissues, but also in the bone around the graft or implant, which leads to disruption of tissue trophism and their subsequent atrophy, as well as scarring of the mucosa.
To avoid the above complications, Astashina proposed an alternative method of prosthetics for patients using dentoalveolar prostheses with multi-thickness solid titanium frames after plastic preparation of the prosthetic bed. The use of such a design prevents the occurrence of functional tissue overload.
The technique for making such a design consists of taking an impression, making and analyzing diagnostic models, planning the design of the prosthesis in accordance with the recommendations of the maxillofacial surgeon. Next, a plaster working model is made, and an individual tray is made from it, and it is fitted in the oral cavity. The boundaries of the spoon are clarified visually, and then fixation is achieved using functional tests. The functional impression is obtained using alginate or silicone impression materials, the choice of which is based on the pliability of the mucous membrane. To create volume, the edges of the working print are edged.
Subsequent stages include obtaining a functional impression from the lower jaw and an anatomical impression from the upper jaw, making working models from superplaster, determining the central occlusion or central relationship of the jaws. For microstomia, it is necessary to use wax templates with rigid bases. The dentofacial prosthesis is constructed in an articulator, and the spatial arrangement of the jaws is determined by the upper jaw and transferred using a face bow.
The main difference between creating prostheses of different thicknesses with titanium frames is the peculiarities of the stage of formation of the wax composition. According to standards, the thickness of the saddle part is 0.5 mm, and the dimensions of the arc are 4.0x2.0 in diameter, while the edge of the base is edged with a wax blank in the form of a cord with a diameter of 0.8 mm.
When modeling the frame or base of a prosthesis to replace a defect, it is rational to increase their thickness to 2.0-2.5 mm in the following areas: in the area of the saddle located above the graft or implant, as well as in the zone of transition of the structure’s saddle into the arch. The edge of the base stop must be edged with a wax blank with a diameter of 1.0-1.2 mm. This approach ensures a reduction in the level of developing functional stresses in the area of the graft or implant. Since titanium alloy has a low specific gravity, such an increase in the volume of the structure frame does not negatively affect the functions of the dentofacial system.
After the wax reproduction modeling stage, the frame of the removable structure is cast on a fireproof model. Minor casting defects (cracks, pores) are eliminated using solid-state laser welding and titanium powder.
Next comes the fitting of the frame on the model and in the mouth. Installation of artificial teeth. It is better to carry out this stage in the articulator. When checking the denture in the oral cavity, you should pay attention to the articulation of the lower jaw. Next, the wax is replaced with plastic. Before handing over the work, the prosthesis must be carefully ground and polished.
Conclusion: We examined the technique of prosthetics of jaw defects with dentoalveolar prostheses. The advantage of orthopedic treatment of patients using dentofacial prosthetic structures made on the basis of titanium alloys is their durability, the possibility of reusing frames in case of loss of supporting teeth and correction of the structure in order to reduce the adaptive period.