Causes and pathogenesis of abscesses and phlegmons
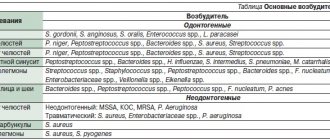
Most purulent lesions of the maxillofacial area are odontogenic in nature. This means that the disease is formed due to the spread of infection from the inflamed root or periodontium. In such cases, streptococci and staphylococci from the primary lesion penetrate through the lymphatic vessels into the deep layers of the soft tissues of the face.
The state of immunity is of great importance in the development of the purulent process. A decrease in the body's protective abilities is a powerful predisposing factor for tissue suppuration.
Stages of development and classification of gum abscess
A gum abscess most often has an acute course, characterized by a clear clinical picture with increasing pain and swelling. Sometimes, in the absence of treatment, the process may subside, the clinic becomes weakly expressed and erased. This means that the abscess has become chronic.
Depending on the location of the purulent focus, several types of pathology are distinguished:
- Periodontal abscess. Localized inside the hypertrophied periodontal pocket (between the alveolar process and the gum). The cause of the pathology is subgingival deposits, which are a breeding ground for the proliferation of bacteria.
- Periapical (root). The leading cause of occurrence is inadequate root canal treatment, leading to periodontal inflammation. Granulations form near the root apex. Progressive inflammation spreads to the periosteum and periodontal tissue. A connective tissue capsule with purulent contents is formed. Over time, a fistula forms with pus coming to the surface in the form of a lump.
- Desnevoy. The purulent cavity is located near the papillae between the segments. A possible cause is an injection into the gum.
Clinical picture of the disease
In the initial stages, abscesses and phlegmons adjacent to the lower jaw are manifested by compaction and progressive swelling of the soft tissues of the face. The skin over the purulent focus is often hyperemic. The key symptom of suppuration is fluctuation - the feeling of fluid in a confined space.
The course of phlegmon is accompanied by general intoxication, in which the patient presents the following complaints:
malaise and feeling of chronic fatigue; increase in body temperature; fatigue and joint pain.
Abscesses, as a rule, do not cause such symptoms due to the limited nature of the pathological process.
Abscess, phlegmon of the maxillofacial area in children is characterized by an acute and severe course of the disease. Diffuse purulent lesions of soft tissues are formed as a result of the imperfection of the children's immune system.
Flux and abscess: causes, diagnosis, treatment methods
Flux and abscess: causes, diagnosis, treatment methods
In modern medicine, the term “flux” as such no longer exists. The once popular word has now been replaced by “odontogenic periostitis.” However, for many, the words “tooth flux” is a more understandable term and means severe pain, swelling and something serious that urgently needs to be addressed to a doctor, and rightly so.
There are different degrees of purulent inflammatory diseases of the maxillofacial area - periostitis (flux), abscess, phlegmon.
Most often they appear against the background of advanced caries.
The first stage of inflammation is periostitis (flux) of the jaw - this is an acute inflammation of the periosteum. The cause of flux is the activation of pathogenic flora: streptococci, staphylococci and other pathogenic, often putrefactive bacteria, which were in a dormant state, under certain factors begin to actively multiply and spread, triggering an acute reaction of the body aimed at eliminating the source of inflammation.
Periostitis occurs as a complication of acute or chronic, but aggravated periodontitis, which in turn appears as a result of advanced caries. Previously treated pulpitis may also be a prerequisite. Much less often, the inflammatory process can develop with difficulty in teething, injuries, as well as periodontal diseases in the presence of periodontal pockets.
Flux can also occur after tooth extraction, due to traumatic removal or incomplete extraction of roots. Sensitization and general factors play a certain role in the development of the disease: cold, overwork, stressful situations that reduce the body’s defense reactions.
Regardless of the cause, the clinical picture develops the same
Flux and its symptoms:
- constant toothache, aggravated by pressing or tapping on the tooth;
- redness and hyperemia of the gum mucosa in the area of the causative tooth
- the formation of a significant tumor in the area of the tooth, upper or lower jaw, depending on its location.
- severe pain that can only go away after taking a painkiller;
- limited mouth opening;
- signs of intoxication of the body in the form of a sharp rise in body temperature, headaches, general malaise and a feeling of chronic fatigue
Abscess – second stage of inflammation
An abscess is a purulent inflammation of tissues with their melting and the formation of a purulent cavity; functionally it is practically no different from periostitis; it forms within a day or two from the onset of the disease. The symptoms in this case are the same, but at the same time more intense. Pus, as with flux, is limited to the periosteum, but can penetrate deeper into the tissue.
Sometimes during the disease a fistulous tract may appear, through which pus will come out. An effect of imaginary well-being is created, because along with the outflow, the signs of inflammation subside. However, with this type of development, the disease becomes chronic; if the infection is not stopped, it can spread to neighboring tissues and cause a complication in the form of osteomyelitis (necrotizing inflammation of the bone).
If the abscess was not drained and the fistula never formed, purulent inflammation begins to spread to the surrounding tissues - phlegmon appears.
Phlegmon is a dangerous omission
Cellulitis is the third, most severe stage of purulent inflammation in the tissues around the tooth. In this case, the pus is not limited to the periosteum alone, but wanders freely through the tissues.
Further spread of the infectious-inflammatory process in the perimaxillary soft tissues usually occurs along the fiber of the interfascial and intermuscular spaces, the fiber surrounding the vessels, nerves, and salivary glands. In this case, tissue compaction occurs, often accompanied by the appearance of asymmetry of the face and neck in the form of swelling. The pain moves beyond the jaw and becomes less localized. Chewing function may be impaired due to pain and limited mouth opening. External breathing may be impaired, and signs of intoxication may increase.
Purulent lesions of the head and neck carry the risk of further spread of purulent infection into the facial muscles, cervical regions, and beyond them into the trachea and chest cavity, into the esophagus, into the heart, and can penetrate into the lymphatic system and brain tissue.
IMPORTANT! If phlegmon is not treated in time, it can be fatal!
Treatment of periostitis, abscess
The first and most important step in treating flux is visiting a doctor.
Treatment is complex: surgical - opening and draining the inflammation, and conservative drug therapy.
Stages of treatment:
- Examination, examination, including x-ray diagnostics, determination of indications for surgical treatment.
- Local anesthesia.
- An incision is made in the gums next to the gumboil so that the purulent contents come out, observing all the rules of asepsis and antiseptics.
- Installation of drainage for further outflow of pus - otherwise the exit from the periostitis site will close faster than it will be completely cleared.
- Removal of the affected tooth, if it is not possible to cure it, or removal of the root remaining in the hole, if we are talking about flux after removal.
- Prescription of antibiotics, anti-inflammatory, painkillers.
- Control inspection and removal of drainage.
- Recommendations for home oral care.
All procedures are performed on an outpatient basis under local anesthesia. After the examination has been carried out and the cause of inflammation has been established, an incision is first made in the area of the flux to release the accumulated pus, after which a so-called drainage - a rubber strip - is inserted into the wound. Treatment of an abscess differs from the elimination of periostitis only in the duration of wearing the drainage.
Next, the indications for tooth extraction or preservation are determined. If the tooth that was the source of infection is destroyed and has no functional or aesthetic value, then it is removed simultaneously with the opening of the abscess. This will improve the emptying of the purulent focus and will contribute to a faster elimination of inflammatory phenomena.
Tooth extraction is sometimes postponed due to perceived technical difficulties or the unsatisfactory condition of the patient.
In other cases, the tooth is preserved: its cavity is opened, the root canal is freed from decay products, and then conservative treatment of chronic periodontitis is carried out. All this is determined by the doctor and depends on the specific situation in the oral cavity. Treatment does not end there, but continues at home with the help of prescribed antibacterial and anti-inflammatory drugs. A repeat examination is scheduled on the 2nd day after surgery, the degree of subsidence of inflammatory phenomena is determined and, depending on this, additional treatment is prescribed. During dressing, local wound treatment is carried out. Around day 3-4, the drainage is removed, but conservative treatment continues.
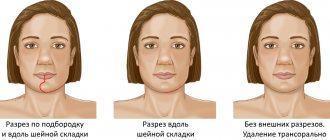
Treatment of phlegmon is carried out in a hospital setting.
What happens after treatment?
After opening the abscess, if no complications arise, the disease enters the subacute stage. In most cases, inflammatory phenomena quickly (after 2-3 days) subside. There is a subsidence of the local inflammatory process: tissue infiltration decreases, the amount of purulent discharge from the wound decreases. As the wound is cleansed, granulation tissue appears, scarring and epithelization occur. At the same time, the severity of the general reactions of the body weakens, and health improves.
Usually, discomfort persists for the first 2 days, although the body temperature gradually begins to decrease, and the pain is no longer so obvious. A sharp improvement in condition and appearance occurs on the third day. Infiltration—tissue compaction at the site of inflammation—can persist for quite a long time. Gradually the “bump” should resolve.
The drainage - a rubber strip - should remain in the wound for some time after the procedure. It prevents the incision from closing prematurely, leaving an open path for pus to escape. It is strictly forbidden to loosen, push out, or adjust the drainage in any way. If a strip falls out, consult a doctor immediately. You should also contact your doctor if you do not feel better 12 hours after opening the flux.
The prognosis of periostitis with timely radical intervention is predominantly positive. Isolated deaths are associated with late seeking of dental care.
Self-medication of flux can lead to further spread of purulent inflammation in the tissues and such serious complications as osteomyelitis of the jaw or phlegmon of the soft tissues of the face and neck.
Prohibited for inflammation:
- try to open the abscess yourself;
- apply warm compresses and dressings;
- independently prescribe antibiotics and other medications;
- take painkillers before visiting a doctor;
- drink aspirin (before and after opening).
Finally, I would like to say one thing: please do not be afraid to consult a doctor for help in a timely manner. The sooner treatment is started, the better the outcome. Take care of yourself!
Diagnosis of the disease
Establishing a diagnosis for acute odontogenic infections includes the following measures:
Collection of medical history. The doctor finds out the patient’s complaints and the general condition of the patient. External examination of the maxillofacial area and palpation of regional lymph nodes. Most inflammatory and purulent processes cause enlargement and pain of the lymph nodes. Instrumental examination of the oral cavity, during which the doctor detects chronic foci of odontogenic infection. X-ray in frontal and lateral projection. Laboratory blood test, in which there is an increase in SOE, leukocytes and a decrease in the concentration of red blood cells and hemoglobin.
Diagnostics
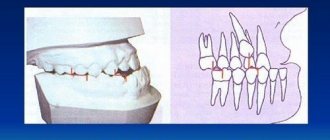
To diagnose a tooth abscess, the dentist must conduct an examination of the oral cavity and take an x-ray of the tooth. An X-ray image reveals signs of an inflammatory process (widening of the periodontal fissure, thinning of the spongy substance of the alveolar process).
A visual examination reveals swollen, bright red areas of the gum mucosa and increased tooth mobility. With periodontal abscess, periodontal pockets up to 6 mm deep and higher, filled with purulent discharge and granulation tissue, are noticeable.
The purpose of diagnostic measures for a tooth abscess is to differentiate the pathology from an exacerbation of chronic periodontitis, cysts, periostitis, osteomyelitis.
General principles of treatment of the disease
The doctor who treats phlegmon of the maxillofacial area is an oral and maxillofacial surgeon.
Each doctor, when starting to treat an odontogenic process in the maxillofacial area, is guided in his actions by the following principles:
The tooth that caused the development of phlegmon is removed. Timely diagnosis is very important due to the characteristics of this area, from where the infection can spread, causing severe consequences (in particular, mediastinitis). It is necessary to eliminate the spread of the infection, that is, promptly open the lesion and eliminate the inflammatory exudate, relieve tissue tension. The rate of subsidence of inflammation depends on the quality of evacuation of all decay products from the wound, that is, careful postoperative treatment of the wound is necessary. Comprehensive treatment of pathology using all means and methods available in this medical institution. Friendly management of the patient with colleagues from other areas, timely appointment of consultations with all specialists for combined lesions. Visible external changes often occur, which are not always pleasant for the patient, which is especially painful in the face area. Therefore, there is an urgent need to organize work with patients by a medical psychologist in the early stages after surgery, especially if there is a significant visible defect. Correct stage-by-stage treatment, organization of medical rehabilitation, referral to the appropriate department with complete information about the patient. Fully informing relatives and the patient about the violation of significant functions of the maxillofacial area, if any. Upon leaving the hospital, the patient should have clear further recommendations, especially if it is necessary to continue treatment on an outpatient basis.
Stages of development of gum abscess
| Disease stage | Description |
| Initial | The beginning of inflammation. If the immune system is functioning well, the process may stop on its own. Symptoms are absent or mild. If the immune defense is insufficient, bone or soft tissue begins to melt. Hyperemia of the mucous membrane and discomfort appear. |
| Subacute | The inflammatory process intensifies. Pus accumulates in the pathological area (near the root, inside the periodontal pocket, near the gingival papilla). The pain intensifies. The tooth reacts to irritation. |
| Acute | Progression leads to abscess formation: a cavity with pus forms in the central zone of infiltration. The clinical picture is clearly expressed: the pain is constant, sharp, swelling appears. A lump appears on the surface of the gum, inside of which there is purulent exudate. Inflammation spreads to the submandibular lymph nodes. |
| Chronic | The abscess on the gum spontaneously opens and the contents of the cavity come out. Signs of acute inflammation subside. |
Complications of abscesses and phlegmon
Purulent lesions of the maxillofacial area can be complicated by the following pathologies:
Sepsis is a serious condition of the body that is caused by the penetration of a bacterial infection into the circulatory system. Treatment of such a complication is difficult due to the development of body resistance to antibiotic therapy. Sepsis is often the cause of death. Mediastenitis in the form of purulent inflammation of the tissue of the mediastinum, where the heart, lungs and bronchi are located. Meningitis . Inflammatory damage to the meninges develops as a result of the spread of purulent infection through the lymphatic and blood vessels of the head.
What is a gum abscess, definition of the disease
Let us consider in more detail what an abscess on the gum is and the mechanism of its occurrence. A purulent focus occurs as a result of long-term untreated inflammation of periodontal tissues. The pathogenesis of the disease is associated with the penetration of pathogenic microorganisms (mainly Bacteroides forsythus and Porphyromonas gingivalis) into the periodontal tissues. Possible routes of penetration of microbes:
- from the outside: through a carious cavity, chips, cracks on the surface of the segment;
- from the inside (hematogenously, lymphogenously): in the presence of other septic foci in the body.
During their life, bacteria produce toxic substances that lyse tissue cells, resulting in the formation of a cavity filled with pus. The abscess under the tooth is surrounded by a connective tissue capsule, which separates it from the intact periodontal tissues.
Microbial metabolic products have a neurotoxic effect on nerve receptors located in the pulp of the segment, which causes pain. In addition, they increase the permeability of the capillary walls, resulting in swelling of the surrounding tissues.
Forecast and prevention of the disease
The prognosis of odontogenic abscesses and phlegmons is usually favorable. A positive treatment result is observed with timely indication of full surgical care. In such cases, the patient must be hospitalized in a specialized medical hospital.
Lethal outcomes from purulent lesions of the soft tissues of the maxillofacial area are associated with late presentation of the patient and systemic suppression of his immunity.
Prevention of the disease is achieved in the following ways:
sanitation of the oral cavity, during which the dentist treats all carious, pulpitic and periodontitis teeth; strict adherence by patients to the rules of personal hygiene and regular brushing of teeth; undergoing regular preventive examinations at the dentist, at least twice a year; timely consultation with a doctor if symptoms of dental diseases are detected. Every person should remember that the cost of prevention is much lower than the cost of treatment. And in some cases, sanitation of the oral cavity can prevent the development of severe complications, which are accompanied by high mortality in patients.
Symptoms
A developing tooth abscess causes the following symptoms:
- throbbing pain in the area of the affected tooth, aggravated by chewing;
- inability to fully open the mouth (if the process occurs in the lower jaw);
- exposure of tooth roots;
- pathological mobility of teeth (typical of periodontal abscess);
- painful swelling of the gums and cheeks;
- enlargement of the submandibular lymph nodes;
- increased body temperature;
- headache;
- weakness.
A change in general condition is usually associated with an acute course of the abscess. At the same time, the process can be chronic. For example, with a periapical abscess, a fistula can form - a canal lined with granulation tissue. As a rule, the fistula opens on the mucous membrane of the gums - in the projection of the apex of the tooth root. Less commonly, the fistula opens into the nasal cavity or maxillary sinuses. The fistula serves to remove purulent discharge, therefore, with chronic abscesses, the clinical picture of the disease can be blurred.
Pediatric dentists are faced with abscesses of primary teeth. Its symptoms are the formation of a lump on the gum filled with pus, aching pain in the tooth.
The appearance of symptoms of a purulent abscess requires an emergency visit to a dental surgeon. Otherwise, the risk of complications increases - for example, phlegmon. This is the name of the purulent process in the subcutaneous fat. Unlike an abscess, it is diffuse, i.e. has no clear boundaries. Cellulitis leads to necrotic damage to the jaw bones, and then to infection of the entire body. This process is life-threatening.
Complications that a gum abscess can cause
Without treatment of the disease and inadequate medical care, complications may develop. Adverse consequences arise due to the spread of inflammation to neighboring organs and tissues, as well as the spread of infection throughout the body with the formation of secondary septic foci. The most common pathological conditions that occur are:
- lymphadenitis - infection of the lymph nodes;
- sinusitis - infection in the maxillary sinuses;
- periostitis of the jaw (inflammation of the periosteum);
- osteomyelitis of the jaw bones (destruction of bone tissue due to purulent-necrotic melting of osteocytes);
- phlegmon - diffuse odontogenic inflammation of soft tissues, accompanied by progressive swelling of the face;
- destruction of the alveolar processes with significant loosening of teeth or their loss;
- peri-implantitis with implant rejection;
- sepsis.
Purulent lesions of soft periodontal tissues are always accompanied by general intoxication of the body. The temperature rises and chills appear. There is a headache, tachycardia, and the pulse quickens. Pain relief with medications brings short-term relief, but symptoms return after the medication wears off.
Reasons for formation
Due to their development, there are two types of perimaxillary abscesses:
- Odontogenic. The cause of development is damaged dental elements.
- Non-odontogenic. Not caused by the condition of the dentofacial apparatus.
The most common causes of anomalies are dental diseases:
- Advanced carious lesions of units, pulpitis.
- Deep periodontal pockets.
- Periodontitis.
- Pericoronitis.
- Infected and impacted molars and premolars.
- Root cyst.
The development of a lesion can be triggered by penetration of infection under the periosteum from a diseased unit.
Reasons for the development of non-odontogenic foci of pus:
- Traumatic lesions of the jaws, elements or soft membranes of the oral cavity with infection.
- Nasopharyngeal and ear infections.
- Complications of unqualified dental treatment.
- Spread of infection to the jaw from other organs and systems.
The development of an abscess depends critically on the general health and immunity of the patient.
Treatment of gum abscess
Treatment of the disease is aimed at solving two main problems:
| Type of treatment | Methods |
| Symptomatic treatment of inflammation and pain syndrome | removal of an abscess on the gum (dissection, installation of drainage for the outflow of pus); antibiotic therapy (penicillins, fluoroquinolones, macrolides). Prescribed to stop the infectious process; NSAIDs (Diclofenac, Indomethacin, Ibuprofen, etc.). Eliminate pain and inflammation; antiseptics (Chlorhexidine, Miramistin). Used in the form of rinses and gum baths for antiseptic treatment of the oral cavity. |
| Etiotropic treatment (elimination of the cause of pathology) | tooth extraction. Carry out when it is impossible to implement tooth-preserving measures; repeated endodontic treatment (opening of canals and their refilling); professional teeth cleaning to remove mineral and soft plaque; removal of the artificial root (for peri-implantitis). |
An abscess on the gum is a serious dental pathology. If treatment is not started in time, the process continues to develop and leads to adverse consequences. To avoid complications, at the first signs of inflammation you should make an appointment with the dentist. ]dentistry in Otradnoye[/anchor] offers assistance in eliminating problems with diseased teeth and periodontal disease.