Matteo Trimarchi Department of ENT and Head and Neck Surgery, San Raffaele Hospital, Milan, Italy
A. Galli Department of ENT and Head and Neck Surgery, San Raffaele Hospital, Milan, Italy
Paolo Cappare Department of Dentistry, IRCCS San Raffaele Hospital, Milan, Italy
Suzan Dababou Department of Dentistry, IRCCS San Raffaele Hospital, Milan, Italy
Raffaele Vinci Department of Dentistry, IRCCS San Raffaele Hospital, Milan, Italy
M. Bussi Department of ENT and Head and Neck Surgery, San Raffaele Hospital, Milan, Italy
Enrico Gherlone Department of Dentistry, IRCCS San Raffaele Hospital, Milan, Italy
Odontogenic infections (OIs) are pathologies originating from the stomatognathic system as a result of complications of dental pathologies or dental procedures. If they are not promptly diagnosed and treated, they can quickly spread throughout the head and neck and, depending on the etiology and the area where they begin, lead to severe, life-threatening complications [1-3]. For the development of OI, not only delayed diagnosis and inadequate treatment are important, but also common comorbidities of patients: diabetes, autoimmune or lymphoproliferative disorders, renal failure, osteoporosis, malnutrition, smoking, alcohol abuse and chronic steroid use - factors that can increase the incidence of OI [12].
OI can develop in both the upper and lower parts of the head and neck. The upper includes the spaces near the upper dental arch, namely the paranasal sinuses, with the maxillary sinuses being involved in most cases [4]. Odontogenic sinusitis (OS) accounts for about 10–30% of cases of chronic antral inflammation [2] and 8% of cases leading to endoscopic nasal surgery [5]. The lower section is characterized by the proximity of the lower dental arch to the fascial cervical spaces: superficial, submental, submandibular, sublingual, parapharyngeal, masticatory, carotid, retropharyngeal, prevertebral. And also to the dangerous space, which extends from the base of the skull to the posterior mediastinum [3, 6, 7]. Odontogenic etiology underlies 57% of cases of cervical-fascial infections [8].
Diagnosis of OI can be challenging: signs and symptoms are often nonspecific or misleading (especially for OI), and the association with overt dental pathology is often not seen or underestimated. Dental symptoms (local pain or hypersensitivity), in fact, do not reliably correlate with odontogenic etiology [2, 9]. This can lead to rapid and effective treatment, symptoms and severe complications [10]. The clinical picture is different between upper and lower OI. Pain/pressure, swelling of the posterior nasal wall, copious mucous discharge from the nose, nasal congestion, decreased/absent sense of smell and an unpleasant taste in the mouth are characteristic of the upper nasal region. While sore throat, pain when swallowing, shortness of breath, enlarged cervical lymph nodes and more serious involvement of other organs and systems characterize the lower one. Fever is often present [2 – 4, 7].
Accurate and clear diagnosis allows not only to identify the complication, but also the specific cause of the infection, which allows for correct treatment and reduces the risk of relapse [10].
In the present study, we analyzed the various pathogenesis that can lead to OI and highlight the importance of collaboration between dentists and otolaryngologists for the effective management of potentially dangerous complications.
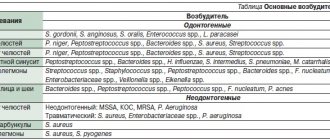
Types of infections
Dentists divide diseases based on their development:
- truly odontogenic. They are caused by a problem tooth. If caries, pulpitis, periodontitis, inflammation are not cured in time, the infection begins to spread further;
- non-odontogenic. The reason is damage to the oral mucosa;
- periodontal. Advanced problems with the gums, periosteum or soft tissues of the neck are to blame for the occurrence of such infections.
Whole groups of microorganisms can be causative agents of infection: viridans streptococci, spirochetes, non-spore-forming anaerobes.
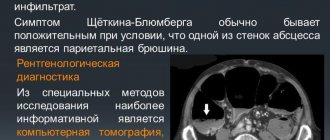
Diagnosis of maxillary sinusitis
The diagnosis is made by an otolaryngologist based on the patient’s complaints, examination (rhinoscopy), and also based on the results of:
- X-rays, linear, computer or magnetic resonance imaging, and orthopantomograms (panoramic images) of teeth.
- General blood test.
- Diagnostic puncture. In the laboratory, the obtained material is examined, identifying the infectious causative agent of the disease.
- Video endoscopic examination. An endoscope is inserted through the puncture, with which the doctor looks at what is happening inside.
Causes of development of odontogenic infections
More often, diseases spread and develop due to patients’ inattention to their health. The reasons are:
- infrequent visits to the dentist. Even if nothing worries you, you need to undergo medical examinations every six months. Professional oral hygiene in a dental clinic removes plaque, tartar, restores the natural shade of enamel and prevents the occurrence of caries and gum problems;
- poor hygiene and bad habits. When a patient does not spend enough time brushing his teeth, does not use dental floss, and self-medicates instead of visiting a specialist, the condition of the oral cavity worsens. Smoking and drinking alcohol have a bad effect on the gums: the tissue becomes thinner, becomes inflamed and begins to bleed;
- unsuccessful dental operations. Serious problems can result from an incorrectly placed filling, traumatic tooth extraction, incompletely cured caries or other disease.
Your dentist will help determine the cause. The specialist will also give recommendations on how to avoid problems in the future.
Hospitalization
The day hospital at our Center is a post-operative support service for patients. Necessary if the patient has concomitant cardiac issues, such as hypertension, arrhythmia, AOS, etc.
Gentle ultrasound surgical protocols for low-impact PiezoSurgery operations in combination with microscopic surgery performed by operating teams consisting of pairs of the most experienced surgeons at our Center allow you to carry out treatment so delicately that you will not need mandatory hospitalization, which is so popular in Moscow hospitals.
All operations are performed only in medicated sleep, without pain or nervous overload.
The treatment will be carried out with respect for your personal time, in a short time and at a comfortable time, the operating teams and anesthesiology department work seven days a week and holidays.
Signs of infection and patients at risk
Main symptoms:
- I constantly have a high temperature and a headache. These are signs of intoxication of the body;
- notice a purulent focus. Redness appears around, the affected area swells and hurts.
Problems also begin in the neck area: the throat hurts, the tongue swells, it becomes difficult to breathe and speech is distorted. Often with such complaints they go to a general surgeon. The doctor helps eliminate the consequences of the infection, but the outbreak still remains, and the disease continues to spread through the vessels and affect the tissues.
People with weak immunity are considered the most vulnerable to odontogenic infections: patients with oncology, hepatitis, HIV, diabetes. By age group, children and patients over 60 years of age are at greatest risk. Chemotherapy and drugs that suppress the immune system also weaken the body.
Clinical case
A 53-year-old patient came to the clinic with complaints of an unpleasant odor from the nose, a strong sensation of cold air in the cold season through the right half of the nose, a burning sensation, and discomfort in the nasal cavity on the right. Headaches on the right.
These complaints have been bothering me for the last 6 months. An MRI of the brain did not reveal any brain pathology; a total darkening of the right maxillary sinus was determined.
The patient consulted ENT doctors several times. She refused the puncture.
During a routine examination of the nasal cavity, the otolaryngologist noted only moderate swelling of the nasal mucosa on the right. The patient was offered an endoscopic examination of the nasal cavity.
An endoscopic examination of the nasal cavity on the right revealed a foreign body - a large conglomerate, putty-like consistency with black (fungal) inclusions, with an unpleasant odor. The volume of the foreign body is 3 cm cubic. Most of the foreign body is located in the deep parts of the nasal cavity and is covered by a deviated nasal septum. There is destruction of the wall of the maxillary sinus with the formation of a wide connection with the nasal cavity. In everyday language, a fairly large hole has formed in the wall of the maxillary maxillary sinus, open into the nasal cavity.
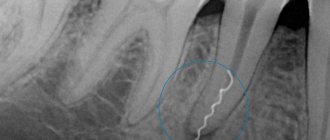
The patient was prescribed an additional examination: computed tomography of the paranasal sinuses. Tomography revealed: the presence of a foreign body in the maxillary sinus on the right (filling material), the sinus is completely filled with dense contents. Extensive defect in the medial wall of the maxillary sinus on the right.
The patient was diagnosed with chronic odontogenic maxillary sinusitis on the right. Foreign body of the right maxillary sinus. Mycetoma (fungal body) of the right maxillary sinus. Surgical treatment is recommended.
Unfortunately, there are more such patients with a similar clinical picture every year.
How are odontogenic infections treated?
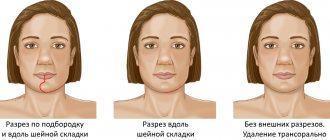
The dentist begins with sanitation of the oral cavity, then carefully opens the abscess. Treatment of dental infections is carried out using different methods depending on the degree of complexity and location of the outbreak. One of the principles is to provide air flow, which will kill pathogens.
If the abscess is too deep in the tissues, the process is monitored using ultrasound. Patients are required to be given antibiotics. Then they are combined with antimicrobial drugs. General strengthening therapy is also used.
If the infection is not treated in time, you may encounter complications:
- purulent inflammations,
- blockage of veins,
- sinusitis,
- damage to the lymph nodes,
- sepsis.
To avoid odontogenic infections, visit your dentist regularly, do not delay treatment, and carefully monitor your oral health.
Why you should entrust your treatment to the ENT Department of Dentistry
ENT dentistry combines two areas of medical services and treatment options - otolaryngology and dentistry . This is a modern format for the clinic’s work on comprehensive rehabilitation in the treatment of traumatic and inflammatory processes in the upper jaw, penetrating into the maxillary sinus or passing along its borders.
The Center for Private Dentistry “Doctor Levin” has been specializing in providing care to patients with combined ENT and dental pathology for many years. Medical and surgical treatment programs are carried out by candidates of medical sciences, maxillofacial surgeons with ENT training.
Recovery after surgery
No hospitalization
A hospital stay for 2-3 days after surgery (as happens in city hospitals) is not required.
Gentle surgical protocols, the use of modern functional equipment and a microscope allow treatment to be carried out as delicately as possible .
All operations are performed in a controlled, drug-induced sleep - this is not general anesthesia ! Recovery from the state is easy, without dizziness, memory loss or clouding of consciousness. The drugs are absolutely safe for the body and are eliminated naturally 40 minutes after stopping the supply.
For patients with vascular and cardiac problems, a day hospital , where you can calmly recover and recover under the supervision of our anesthesiologist-resuscitator.
Accelerated rehabilitation
Recovery after the intervention occurs within a week. For those who want to speed up the process, our Center provides a set of procedures to reduce pain, resolve hematomas and swelling - carried out on the day of surgery.
Home care
Medications are prescribed - antibiotics, painkillers and decongestants. To prevent the patient from running to pharmacies in a postoperative state and to avoid purchasing counterfeit products “on the side,” the entire package of drugs is collected and given out free of charge .
The package contains all the necessary medications for taking and caring for the surgical area.
Please follow the recommendations and do not skip taking medications to avoid complications. The instructions are in the medicine package.
If you suspect a worsening condition, contact the clinic immediately. The telephone number for the 24-hour patient support service is listed in the memo.
Complications
With odontogenic sinusitis, a chronic inflammatory process occurs. Dental microflora appears in the sinus, not typical for the upper respiratory tract, which can destroy bone tissue. Due to the fact that the paranasal sinuses have contact with the orbit and brain, odontogenic sinusitis can lead to severe complications:
- intraorbital (orbital phlegmon, ophthalmitis, optic nerve neuritis);
- intracranial (meningitis, encephalitis, brain abscess).
Therefore, at the slightest suspicion of this disease, you should consult a doctor.
Symptoms of the disease
The symptoms of the disease are similar to classic inflammation of the maxillary sinuses. Only a highly qualified otolaryngologist will be able to distinguish odontogenic sinusitis from ordinary sinusitis.
Signs of odontogenic sinusitis are:
- constant nasal congestion;
- purulent nasal discharge with a characteristic odor;
- the appearance of odor from the patient’s mouth;
- pain in the cheek area under the eyes;
- acute toothache in the upper jaw;
- elevated body temperature.
Symptoms also include a general deterioration in well-being, a persistent feeling of fatigue, and problems sleeping.
Specific symptoms of purulent odontogenic sinusitis are pain when lightly pressing on one of the cheeks or when lightly tapping on the teeth located in the area of the inflamed sinus.
Chronic odontogenic sinusitis is manifested by discomfort in the affected sinus area. In general, the patient feels satisfactory until a period of exacerbation occurs.