Oral tuberculosis is an infectious disease that, like other types of tuberculosis, is caused by mycobacteria. This pathology is classified as chronic. As a rule, the inflammation characteristic of tuberculosis, affecting the lining of the mouth and the red border around the lips, is secondary: that is, it occurs as a consequence or the most characteristic manifestation of other forms of tuberculosis. For example, these include tuberculous lesions of the lymph nodes and bones.
The mucous membrane of the oral cavity is far from the most favorable environment for the development and reproduction of mycobacteria that cause tuberculosis. As a rule, when entering this environment, mycobacteria die. However, in the presence of favorable circumstances (microtraumas, mechanical damage in the oral cavity, opening the gates for infection), bacteria penetrate inside and provoke the formation of a tuberculosis ulcer.
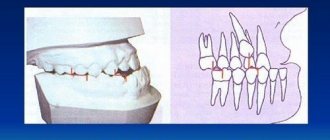
Oral tuberculosis is a relatively rare form of tuberculosis, usually diagnosed only in children. This is due to the characteristics of teething in children.
In an infant, such a disease can be extremely severe and includes the generalization of tuberculosis infection. Secondary tuberculosis infection begins to develop as tuberculous lupus or miliary ulcerative tuberculosis.
Tuberculosis is transmitted by airborne droplets. The incubation period lasts from eight to thirty days, and after this the formation of an uneven, blurred ulcer begins, which is severely painful. After a few days it begins to gradually increase. At the same time, the adjacent lymph nodes swell. There are no other signs of inflammation yet
Classification of types of oral tuberculosis
Oral tuberculosis is a disease that appears and develops mainly in patients with reduced immunity. The disease is caused by Koch's bacillus. The source of inflammation located in the patients' oral cavity is secondary in most cases. It develops as a result of the spread of infection from the main focus, and spreads through the circulatory or lymphatic systems. In the case when the patient is affected by the pulmonary form of tuberculosis, the infection spreads to the oral cavity due to the penetration of mycobacteria contained in the sputum.
There are four forms of oral tuberculosis. Among them:
- Primary tuberculosis of the oral cavity. Transmitted by the respiratory or fecal-oral route, this disease almost never occurs in adults. Most patients with this diagnosis are infants.
- Tuberculous lupus. It is the lupus form of oral tuberculosis that is most often encountered in dental practice. Erosive elements are localized on the mucous membrane of the gums. If treatment is not started on time, these tumors can develop into a malignant form.
- Miliary-ulcerative form. This form usually develops in patients who have already been weakened by tuberculosis. Along with their cough, they produce sputum, which is a source of bacteria that cause oral tuberculosis. The lesions are on the palate and tongue, in rare cases - in the area of marginal gums or on the side of the cheek.
- Scrofuloderma. This form of the disease is diagnosed in most cases in children. The clinical signs of scrofuloderma are somewhat different from those of other forms of oral tuberculosis. In the first stages - the appearance of not a tubercle, but a rather large nodule. After its softening and necrosis occurs, the stage of formation of fistula tracts begins. The healing process of the surface of the resulting ulcers takes a long time, and after it characteristic fringed scars form.
What provokes it?
Infection occurs more often by airborne droplets, less often by nutrition. After an incubation period of 8 to 30 days, an ulcer with undermined, uneven edges and a granular, dirty-gray bottom appears at the site of the entrance gate of the infection. Tuberculosis ulcers are characterized by the absence of acute inflammatory phenomena and severe pain. At the base and along the edges of the ulcer there is a small infiltrate, more pronounced when the lesion is localized on the red border of the lips. 2-4 weeks after formation, the ulcer increases in size. Regional lymph nodes also enlarge and harden, often suppurate and open. The general condition of the patients changes: low-grade fever, weakness, and increased sweating appear.
Diagnostics
Primary tuberculosis of the oral cavity is diagnosed during an external examination. Thus, it is characterized by the presence of lacerations and ulcers in the corners of the mouth with yellow, gray and bluish layers. Areas with ulcers tend to gradually enlarge.
At the same time, the lymph nodes begin to enlarge.
Diagnosis is carried out on the basis of the collected anamnesis, as well as using histological and bacterioscopic studies. During examination, dense painful lumps or ulcers are found on the mucous membrane, depending on the severity of the condition.
There is minor inflammation. The process of formation of adhesions begins between the lymph nodes and the surrounding surface.
Miliary tuberculosis in old age
T
tuberculosis (TBK) in elderly and senile patients continues to be one of the important clinical problems for general practitioners in non-specialized departments and hospitals. According to numerous data, the highest percentage of errors in the diagnosis of TBC in the clinic of internal diseases is observed in the elderly and elderly. It is noteworthy that over time the situation remains virtually unchanged, despite the improvement of diagnostic methods for TBC and the advent of modern radiation, endoscopic and microbiological research methods. According to A.E. Rabukhin, dating back to 1975, about 80% of patients who died from tuberculosis in therapeutic and infectious diseases departments and who were not registered in anti-tuberculosis dispensaries were over 50 years old [1]. According to later data [2], in 37 of 60 deaths in geriatric hospitals, TBC was diagnosed only at autopsy, and in a third, malignant tumors of various localizations were misdiagnosed intravitally. If we take into account the current widespread trend towards a decrease in the number of pathological autopsies of deceased elderly people, there is reason to believe that the true frequency of unrecognized TBC in non-specialized hospitals may be higher.
The main reasons for the difficulty of diagnosing TBC and related errors in the elderly and elderly are
are the following:
• atypical course of the disease and its pathomorphosis at a given age;
• frequent presence of concomitant pathology (multimorbidity) with syndrome-like manifestations;
• long-term torpid course of a chronic (“old”) process under the guise of other respiratory diseases;
• the severity of the patient’s condition (decompensation of concomitant pathology, etc.), which does not allow adequate examination;
• insufficient alertness of general practitioners regarding the reality of TBC in the elderly.
To illustrate the features of the course and difficulties of diagnosing TBC in old age, we present an observation.
Patient L., 78 years old,
was admitted to the 7th City Clinical Hospital in Moscow with
complaints
of an increase in body temperature to 38–39°C for 3 weeks, resistant to gentamicin, pain in the lower spine, and weakness.
History:
chronic bronchitis, coronary heart disease, duodenal ulcer.
Objective
the patient's condition is serious, the patient is adynamic, respiratory rate 28 per 1 min, hard breathing, dry scattered wheezing, single moist wheezing in the lower parts of the lungs, heart rate 105 per minute, blood pressure 160/90 mm Hg. Heart sounds are rhythmic, systolic murmur in the aorta. The liver protrudes from the hypochondrium by 3 cm, the spleen is enlarged. Peripheral lymph nodes are not enlarged. Pain on palpation of the lumbar spine. The patient's mobility is limited due to back pain.
Blood tests:
Нb 90 g/l, er. 2.7x1012/l, tr. 95000, lake. 9200: p. 7%, p. 70%, l. 10%, m. 13%. ESR 65 mm/h. Total protein 60 g/l. Electrophoretic examination of serum showed no monoclonal immunoglobulin, cholesterol 4.6 mmol/l, fibrinogen 5 g/l, urea 7 mmol/l.
Analysis of urine:
specific gravity 1015, protein 0.65%
°
, erythrocytes 2–3 per field of view, leukocytes – 3–4 per field of view.
Chest X-ray
: small-focal dissemination in both lungs, mainly in the upper parts against the background of strengthening and deformation of the pulmonary pattern.
Ultrasound of the abdominal organs:
an increase in the size of the liver with the presence of diffuse changes in it. The size of the kidneys is not changed, moderate expansion of the pyelocaliceal system on both sides. Mass in the upper pole of the right kidney (cyst?).
X-ray of the spine
(Fig. 1): deformation of the body of the IV lumbar vertebra, heterogeneous structure, destruction of the upper endplate.
Rice.
1. X-ray of the spine of patient L. Echocardiography:
left ventricular hypertrophy, sclerosis and calcification of the aortic valve. ECG – diffuse changes in the myocardium.
Gastroscopy:
cardia failure, reflux esophagitis, erosive gastritis.
The patient's condition continued to be serious. The severity of the condition was due to severe intoxication with the probable development of disseminated intravascular coagulation (single skin hemorrhages, mucosal erosions, thrombocytopenia).
The final diagnosis remained unclear. The available clinical and radiological symptoms - bilateral pulmonary dissemination, radiological changes in the lumbar vertebra, fever resistant to antibiotics, anemia, increased ESR, the presence of a mass in the kidney - gave reason to suspect a tumor of the right kidney with metastases to the lungs and spine. At the same time, hematogenously disseminated tuberculosis could not be completely excluded. Multiple myeloma was excluded in this patient based on the absence of monoclonal immunoglobulin in the blood.
Treatment
The patient included antibiotics: cefoperazone, ciprofloxacin, infusion therapy (fresh frozen plasma, hemodez), antiplatelet agents (pentoxifylline), analgesics. Despite the therapy, the patient's condition progressively worsened: signs of heart failure appeared, gastric bleeding occurred, which resulted in death.
Clinical diagnosis:
right kidney cancer with metastases to the lumbar spine and lungs, chronic pyelonephritis. Acute gastric erosions, gastric bleeding, pulmonary edema. IHD: atherosclerotic cardiosclerosis, aortic atherosclerosis, stage II circulatory failure. Chronic bronchitis without exacerbation, pulmonary emphysema.
During pathological examination
a destructive process was discovered in the IV lumbar vertebra with the presence of yellowish masses; multiple whitish millet-like tubercles in both lungs, more intense in the infero-posterior regions; narrowing of the lumen of the left coronary artery by 70%; fibrous plaques and calcification of the aorta; multiple erosions of the gastric mucosa with “melena”-type contents in the small and ascending colon.
Histological examination of internal organs:
lungs - multiple granulomas with epithelioid cells and Pirogov-Langhans cells, areas of caseous necrosis. In some visual fields around the tubercles there is pronounced emphysema (Fig. 2). Heart – fatty degeneration of myocardiocytes, diffuse fields of connective tissue. Liver – multiple tuberculous granulomas (Fig. 3) with a typical structure. IV lumbar vertebra – pronounced caseous necrosis, tuberculous granulomas. Paratracheal lymph nodes - the pattern is erased due to a large number of tuberculous tubercles with Pirogov-Langhans cells. Duodenum - superficial necrosis of the epithelium, hemorrhages in the surface layer. Kidneys – a picture of chronic pyelonephritis.
Rice. 2. Pulmonary enphysema
Rice. 3. Tuberculous granulomas in the liver
Thus, in a 78-year-old patient who was diagnosed intravitally with kidney cancer with distant metastases,
acute miliary TBC with damage to the lungs, liver, lymph nodes, and tuberculous spondylitis of the IV lumbar vertebra were posthumously identified.
The morphological picture in the form of foci of caseous necrosis in the affected organs indicated the activity of the process, which was manifested by clinical and laboratory signs. The source of hematogenous dissemination of tuberculosis infection was, in all likelihood, tuberculous spondylitis of the IV lumbar vertebra, in which an acute destructive process with significant destruction and the presence of massive caseous areas was identified.
Discussion
Diagnosis of tuberculous spondylitis in the elderly presents considerable difficulties. The existing pain syndrome is usually regarded as a manifestation of senile osteoporosis, spondylosis, or osteochondrosis. Detected x-ray changes in the spine with a corresponding clinical picture force the doctor to first conduct an oncological search (myeloma, cancer metastases), which is burdensome for the elderly and often does not confirm the presence of a primary tumor focus. However, even in such situations, the likelihood of tuberculous spondylitis is not taken into account.
No less difficulties arise when diagnosing miliary pulmonary tuberculosis in the presence of radiological signs of pulmonary dissemination. One of the objective sources of errors in the diagnosis of pulmonary tuberculosis in old people is diseases that often occur at this age with a syndrome-like picture. These diseases (eg, tumors, nonspecific inflammatory diseases) are targeted by clinicians in large part because of their frequency and recognized reality in late life. Miliary TBC of the lungs was the most common form in postmortem examinations of deceased patients (average age 84.5 years) who were diagnosed with tumor diseases during their lifetime [3]. In another study [2], of 85 deceased patients in whom active TBC was diagnosed during postmortem examination, 12 patients with a mean age of 79.5 years were diagnosed with cancer antemortem, and radiological changes were detected in half of the patients.
The difficulties of timely recognition of TBC in the elderly are aggravated by the severity of the patients’ condition due to the advanced process
, as well as decompensation of concomitant diseases (heart and respiratory failure, anemia, etc.). The latter often come to the fore in the clinical picture of the disease. On the other hand, the severity of the patients’ condition and often the short duration of their hospital stay (due to death) do not always allow for a detailed and targeted examination.
The pathogenetic background for the development of TBC in late age can be involutional T-cell immunodeficiency, disturbances in the local protection of the lungs [4], as well as immunodeficiency states caused by serious diseases (tumors, diabetes mellitus, treatment with antibiotics, glucocorticoids, unbalanced nutrition).
Literature:
1. Rabukhin A.E. Tuberculosis yesterday and today. Ter. arch. 1978; 3:3–10.
2. Mac Gee W. Z Gerontol. 1989; 22 (6): 311–4.
3. Chastonay Ph. Schweiz med W. schr. 1988; 118(44):1612–5.
4. Adambekov D.A., Salov V.F., Litvinov V.I. Aging, anti-tuberculosis immunity, immunocorrection. Prob. tuberk. 1993; 12:52–55.
Treatment of oral tuberculosis
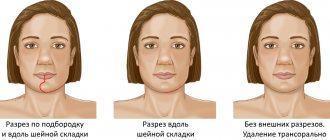
Treatment of this form, like all others, is carried out in specialized institutions - tuberculosis dispensaries. First of all, the underlying disease is treated. To prevent the bacterial infection from spreading further, antiseptic baths are prescribed.
After the acute condition has been relieved, it is necessary to take care of timely and high-quality sanitation of the oral cavity. It is important to promptly consult a specialist at the first symptoms: advanced oral tuberculosis leads to serious consequences for the patient’s health.
Causes
Koch's bacillus has a shell that is resistant to acidic environments. It is able to survive freezing, drying, exposure to alkalis, and much more. etc. Characterized by the ability to form so-called L-forms with increased adaptability. The most pathogenic microbacteria for humans are:
- Mycobacterium tuberculosis humans;
- Mycobacterium bovis.
Microbacteria enter the body through contact, air, mixed and other routes. This is how the first inflammatory focus is formed. A child can also be infected during the mother's pregnancy - through the placenta or during childbirth, if it swallows amniotic fluid. Source: https://www.ncbi.nlm.nih.gov/pubmed/24548085 Marais BJ Tuberculosis in children J Paediatr Child Health . 2014 Oct;50(10):759-67. doi: 10.1111/jpc.12503. Epub 2014 Feb 19
Children at risk include:
- not vaccinated with BCG;
- long-term treatment with antibiotics, hormonal or cytostatic agents;
- having HIV status;
- living in unfavorable conditions (social and/or sanitary);
- having diabetes mellitus;
- with weakened immunity;
- under 2 years of age;
- and etc.
Methods of transmission
- Airborne - through the sneezing, coughing of a patient with an open form of the disease, and even when drying out, the bacillus retains its pathogenicity.
- Alimentary – through the digestive tract. The infection enters the body due to poor hand hygiene or poorly washed and unprocessed food.
- Contact – the infection enters a person through the conjunctiva of the eyes, through kissing, sexual contact, through contact of contaminated objects with human blood, or the use of other people’s hygiene items.
Types and forms of pathology
According to the period of occurrence in medicine, stages are distinguished:
- infiltration;
- decay;
- contamination;
- resorption;
- seals;
- the appearance of scars;
- calcification.
| Form | Peculiarities |
| Chronic and early | It occurs against a background of body temperature up to 40℃, cough, pain in the lungs, uneven breathing, wheezing, decreased appetite, and loss of strength. |
| Respiratory damage | Includes pathologies:
|
| Other localizations | There may be lesions:
|
How to treat tuberculosis?
Treatment of the pathology depends on its type, but most often a course of antibiotics is prescribed. Tuberculosis is a dangerous disease that requires immediate treatment. This allows the person to return to their normal lifestyle.
Antibacterial therapy is aimed at suppressing the proliferation of the tuberculosis pathogen.
Treatment takes place in 2 phases: in the first, several drugs are used at once to reduce the population of microbacteria, the second phase is maintenance therapy. Antibiotics stop the proliferation of bacteria and their release into the environment, the inflammatory process.
After taking such potent medications, a person needs additional supportive therapy that will strengthen the body and reduce the toxic effect. For this, immunostimulants (restore liver function), sorbents (remove toxic breakdown products of chemotherapy drugs) and vitamin complexes are prescribed.
After taking the drugs for two weeks, most people are no longer contagious and feel much better. However, it is very important to continue taking your medications as directed by your doctor and complete your entire course of antibiotics.
Prices
| Name of service (price list incomplete) | Price |
| Appointment (examination, consultation) with a pulmonologist, primary, therapeutic and diagnostic, outpatient | 1950 rub. |
| Consultation with a candidate of medical sciences | 2500 rub. |
| Professor consultation | 4500 rub. |
| Consultation (interpretation) with analyzes from third parties | 2250 rub. |
| Prescription of treatment regimen (for up to 1 month) | 1800 rub. |
| Study of external respiratory function (RPF) with drug tests | 1800 rub. |
| X-ray of the chest organs (survey) | 1900 rub. |
| X-ray of the chest organs in 2 projections | 2900 rub. |
Types of tuberculosis
- Open form - the disease is clearly expressed, bacteria are easily detected in sputum and feces. The patient himself poses a danger to others, since the infection is transmitted by airborne droplets. Microbacteria can be found in sputum, urine, and feces.
- Closed form - not dangerous to others. Characterized by the difficulty of detecting infection in sputum. The most common tuberculosis is pulmonary tuberculosis, but this infection can also affect bones, joints, genitourinary system, intestines, peritoneum, meninges, central nervous system, peripheral lymph nodes, skin
How is tuberculosis diagnosed?
To diagnose the disease, you must first consult with your primary care physician, who, if tuberculosis is suspected, will refer you to a phthisiatrician (tuberculosis specialist) for further diagnosis and treatment. Diagnosis will depend on the type of disease.
Diagnosis of pulmonary tuberculosis
An X-ray of the chest is required, which provides an image of the lungs. For pulmonary TB, the scan should show changes in the appearance of the lungs, such as scarring.
To confirm the diagnosis, samples of mucus and sputum are taken and analyzed under a microscope for the presence of tuberculosis bacteria.
Examination for extrapulmonary tuberculosis
- CT scan
- magnetic resonance imaging (MRI)
- ultrasound examination (ultrasound)
- blood tests
- Analysis of urine
- biopsy - a tissue sample is taken from the affected area to be tested for the presence of tuberculosis
Examination for latent tuberculosis
To prevent the disease, every person is required to undergo fluorography and an X-ray of the lungs at least once every two years.