Miramistin is an unremarkable bottle with a spray nozzle. But he can do so many things! If you look at the list of indications, we can say that the drug helps with literally everything. From anything that is infectious in nature. Or is about to become one. Burns, wounds, viruses, operations and much more are the scope of application of Miramistin. It relieves inflammation and has an antimicrobial effect. It is especially pleasant that the simple composition is characterized by a virtual absence of contraindications or adverse reactions, and the drug can be prescribed from birth.
Miramistin copes well with burns
Description
Miramistin is a domestic broad-spectrum antiseptic drug that is used for the prevention and treatment of bacterial, fungal and viral infections. Initially, the drug was intended to disinfect compartments on Soviet spaceships and stations. And now Miramistin has shown itself to be excellent in the prevention and therapeutic treatment of wounds, purulent-septic processes, the appearance of which accompanies surgery and traumatology. Miramistin effectively fights pathogenic microorganisms, therefore it is applicable in gynecology, urology, dentistry, otolaryngology and other branches of medicine.
But you should not think that Miramistin simply has an antimicrobial effect; it is quite strong and fights even those strains that are insensitive to other antibiotics. Miramistin interacts with ascomycetes, yeast and yeast-like fungi, dermatophytes, and some other pathogenic fungi. And what is especially important, Miramistin is able to influence human immunodeficiency viruses, herpes, etc. That is, demonstrate an antiviral effect. The medicine is also quite active against pathogens that cause sexually transmitted diseases (STDs).
Miramistin prevents infection of burns and wounds, as it accelerates the absorption of purulent secretions, stimulates the process of tissue regeneration and the manifestation of the body's protective reactions.
And all these wonderful properties practically do not cause allergic reactions or irritation to the skin. This is what it means that the product was developed for the space industry.
Causes of runny nose and cough
A cough in an infant may be due to the following reasons:
- respiratory viral infections;
- bacterial infections and complications: whooping cough, tracheitis, laryngitis, pharyngitis, bronchitis;
- allergic reaction;
- congenital heart diseases.
The cough reflex can also be physiological. For example, it may occur in response to dry air, dust entering the infant’s respiratory tract, or excessive salivation during teething. A runny nose also often occurs against the background of the appearance of the upper incisors.
Coughing after sleep with a runny nose is common: nasal discharge flows down the back wall of the throat, which provokes a spasm and a reflex release from the contents. You need to sound the alarm when the cough is barking or severe, persists for a long time after waking up, and is accompanied by a high body temperature. It is also important to get help from a doctor as soon as possible in case of green sputum or the appearance of blood streaks in the discharge. A paroxysmal, uncontrollable cough is also a reason to show the child to the doctor as soon as possible. But a rare dry cough should not be treated on its own; often it can be the only sign of incipient bronchiolitis or obstructive bronchitis.
It is important to treat a runny nose in a newborn child in a timely manner. Even slight nasal congestion can be a serious problem, as the baby cannot breathe or eat properly. This can cause moodiness, sleep disturbances and digestive problems. Impaired nasal breathing can lead to damage to the lower respiratory tract, as the baby is forced to breathe through the mouth.
Indications
The range of uses of Miramistin is quite wide. So, the attending physician may prescribe the use of Miramistin in the following cases:
- In traumatology and surgery: prevention of suppuration, treatment of purulent wounds. Used in the treatment of purulent-inflammatory diseases of the musculoskeletal system.
- In obstetrics and gynecology: treatment and prevention of suppuration of wounds and injuries received during childbirth, treatment of inflammatory and infectious processes of the genital organs (vulvovaginitis, endometritis).
- In venereology and dermatology: treatment and prevention of dermatomycosis, pyoderma, also used for mycoses of the feet, candidiasis of the skin and mucous membranes, in particular, for thrush.
- In urology: treatment of urethritis (acute and chronic forms) and urethroprostatitis.
- In dentistry: prevention of infectious and inflammatory processes occurring in the oral cavity. Treatment of stomatitis, gingivitis, periodontitis. Miramistin also carries out hygienic treatment of removable dentures.
- In otorhinolaryngology: used for sinusitis, otitis, laryngitis, pharyngitis, chronic tonsillitis. Miramistin is prescribed for sore throat. In particular, the drug is used in complex therapy for pharyngitis, chronic tonsillitis, as well as for sore throat in children from the age of three.
- Combustiology: treatment of superficial and deep burns of II and IIIA degrees, preparation of burn wounds for dermatoplasty.
- The solution is used for individual prevention of the development of diseases that are sexually transmitted to humans (syphilis, gonorrhea, chlamydia, trichomoniasis, genital herpes, genital candidiasis, etc.).
How to use Miramistin
The use of Miramistin as an antiseptic drug is quite widespread. In addition to the areas listed in the table below, the medicine is prescribed for the treatment of acne, as a prevention of influenza and colds, and for diaper rash.
How to use Miramistin correctly
Please note that Miramistin may cause irritation of the nasal mucosa.
Any prescription of the drug, indication of the dosage and duration of the course are made by the attending physician.
| Disease | Course duration | Reception |
| Purulent sinusitis. Tonsillitis, pharyngitis and laryngitis. | From 4 to 10 days. | The maxillary sinus is washed with a sufficient amount of the drug. Gargling and/or irrigation (10-15 ml) 3-4 times a day is indicated. |
| Stomatitis, gingivitis, periodontitis. | Until remission occurs. | Rinse the mouth with 10-15 ml of the drug, 3-4 times a day. |
| Surgery, traumatology, combustiology. | 3-5 days. | 2-3 times/day. irrigate the surface of wounds and burns, loosely pack wounds and fistula tracts, fix gauze swabs soaked in the drug. |
| Prevention of postpartum infection. C-section. | 5-7 days. 7 days. | Irrigation with a gynecological nozzle is indicated before childbirth, during childbirth, after each vaginal examination and in the postpartum period, 50 ml of the drug in the form of a tampon (2 hours). Before the operation, the vagina is treated, during the operation - the uterine cavity and the incision on it, and in the postoperative period, tampons moistened with the drug are inserted into the vagina (2 hours). |
| Angina. | Until remission occurs. | Rinse 4-5 times/day. |
| Urethritis and urethroprostatitis. | 10 days. | Miramistin is injected using a urological applicator into the urethra 2-3 ml 1-2 times a day. |
| Prevention of sexually transmitted diseases. | Miramistin is used no later than 2 hours after sexual intercourse. | Using a urological applicator (gynecological attachment), insert Miramistin into the urethra for 2-3 minutes: for men (2-3 ml), for women (1-2 ml) and in the vagina (5-10 ml). Treat the skin of the inner thighs, pubis, and genitals. After the procedure, it is recommended not to urinate for 2 hours. |
| Thrush, inflammatory diseases of the genital organs. | 7-14 days. | A tampon is moistened with Miramistin and inserted intravaginally. Douching is indicated. |
| Purulent otitis. | Until remission occurs. | 2 ml of solution is injected into the external auditory canal. |
Miramistin during pregnancy and lactation
Miramistin can be used by pregnant women and nursing mothers, but, as is usually the case with this group of patients, use is possible after consulting the doctor supervising them. They can be used to gargle, rinse the nose and treat affected surfaces, since Miramistin does not enter the bloodstream. But in any case, an obstetrician-gynecologist should prescribe the drug during pregnancy and breastfeeding.
Miramistin for children
Miramistin for children
If we touch on the issue of using Miramistin in pediatrics, the drug can be prescribed by a doctor for children during an exacerbation of pharyngitis or during the exacerbation stage of chronic tonsillitis. If such conditions are diagnosed, then most likely the pediatrician will prescribe irrigation of the child’s throat with Miramistin.
- children 3-6 years old: press the head of the spray nozzle once (3-5 ml per irrigation), 3-4 times/day;
- children 7-14 years old: press twice (5-7 ml per irrigation), 3-4 times/day;
- children over 14 years old: 3-4 times pressing (10-15 ml per irrigation), 3-4 times/day.
As for the nose, care should be taken here, since Miramistin can have an irritating effect on the mucous membrane. Also, Miramistin is prescribed to young patients if they have chickenpox. The skin is treated with Miramistin in order to disinfect it. If the drug is prescribed to an infant, it is most likely for the treatment of surfaces that require disinfection. Miramistin, due to its composition, accelerates the regeneration of the epithelium. After the drug has dried naturally, you can use diaper rash cream or a special powder containing talc.
The instructions for use stipulate the age of the child from which the use of Miramistin is permissible. Thus, children under one year of age undergo therapy with Miramistin only under the supervision of a specialist; children up to three years of age can be prescribed the drug solely for indications. Remember that children's bodies are sensitive, and even such a safe drug as Miramistin can cause allergic reactions.
Analogs
Analogs
At the moment, one structural analogue of the drug Miramistin has been released on the pharmacological market:
- Okomistin (eye drops).
If you do not take into account the composition, then in terms of therapeutic action the antiseptic Chlorhexidine is closest to the drug Miramistin. You can also note Octenisept.
Miramistin or Chlorhexidine?
Most often, when they talk about replacing the drug Miramistin, Chlorhexidine is cited as an example. What is the significant difference between these drugs? If you focus on the indications for use, they are almost identical. True, it is believed that Chlorhexidine has more side effects and is generally toxic. But this disadvantage has a downside. This “aggressiveness” is directed against microbes. Miramistin is a more gentle remedy, it is safe, so it is prescribed for the treatment even of infants. The drug Miramistin does not monitor negative reactions of the body to its use; it is less likely to cause a burning sensation and unpleasant consequences in the form of dysbacteriosis.
Local anti-inflammatory therapy for acute pharyngitis
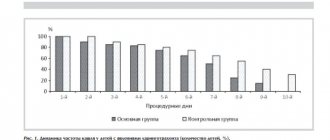
According to the etiological factor, OF is usually divided into viral, bacterial, fungal, allergic, traumatic (due to foreign body entry or surgical intervention) and caused by exposure to irritating factors (hot liquid or steam, acids, alkalis, radiation, etc.) [10, 12] . The causative agents of OF are presented in Table 1. It is known that approximately 70% of pharyngitis is caused by viruses, among which are rhino-, coronaviruses, respiratory syncytial virus, adenovirus, influenza and parainfluenza viruses. It is believed that among the bacterial pathogens of OF, the leading role belongs to β-hemolytic streptococcus of group A - it causes 15-30% of cases of the disease in children and 5-17% in adults. Relatively rarely (<6%, Fig. 1), tonsillopharyngitis can be caused by streptococci of groups C and G [17, 20]. In 90% of cases, the bacterial flora of the posterior pharyngeal wall is represented by associations of 2–3 types of microbes [11]. Medicines used for local treatment of pharyngitis can be divided into 6 groups: local antibiotics and antiseptics, local antimycotics, immunocorrectors, local anesthetic and anti-inflammatory drugs, homeopathic remedies [11]. Uncomplicated pharyngitis usually does not require systemic antibiotics [2].
The prescription of systemic antibacterial therapy is still considered, if not mandatory, then at least justified in most acute respiratory infections. Thus, in Europe and the Russian Federation, doctors prescribe antibacterial agents to 70% of patients at their first visit with complaints of sore throat (GG) as the main symptom of acute catarrhal pharyngitis and tonsillitis. The use of these drugs can have adverse consequences in the form of the development of direct and cross-resistance of bacteria to antibiotics, which leads to further ineffectiveness of antibiotic therapy. The upper respiratory tract is colonized by a wide range of gram-positive and gram-negative flora, aerobes lacking cell walls, as well as anaerobic microorganisms. This diversity of microorganisms provides optimal opportunities for the transmission of resistance determinants, and the reservoir in this case is the normal human microflora. The use of both systemic and topical antibiotics in cases where they are not indicated contributes to the spread of antibiotic-resistant microorganisms in the population. These undesirable consequences apply not only to systemic, but also to topical antibiotics [3, 10]. In Russia, the problem of irrational use of antibiotics for upper respiratory tract infections is complicated by the possibility of their acquisition by patients over the counter. The benefit of using antibiotics for pharyngitis is negligible. According to the results of a meta-analysis, in 90% of patients with pharyngitis, symptoms disappear within a week, regardless of the use of antibacterial agents [4, 12]. In this case, antibiotics can reduce the duration of symptoms of pharyngitis and tonsillitis by less than 1 day. Moreover, the likelihood of returning to a medical facility for pharyngitis in people who received antibiotics is even higher than in those who did not take them [10].
Thus, systemic antibacterial therapy is indicated only for confirmed bacterial etiology of pharyngitis. According to international recommendations, the clinical criteria for the bacterial etiology of pharyngitis are as follows [14]: – inflammation of the tonsils; – enlarged cervical lymph nodes; – fever; – absence of cough. If the patient has all 4 criteria, then antibiotic therapy can be prescribed empirically. The presence of 2 or 3 of the listed criteria, as well as a positive test for group A streptococcus, are indications for prescribing antibiotics. Patients who have one of these criteria or none do not require a test for streptococcal antigen and antibiotic therapy [1, 2, 13].
The clinical picture of OF is characterized by soreness, dryness, discomfort and GD when swallowing (especially with an empty throat), and less commonly - general malaise and a rise in temperature. When the tubopharyngeal ridges become inflamed, the pain usually radiates to the ears. On palpation, tenderness and enlargement of the upper cervical lymph nodes may be noted. Pharyngoscopy reveals hyperemia of the posterior wall of the pharynx and palatine arches, individual inflamed lymphoid granules, but there are no signs of inflammation of the tonsils characteristic of angina. OF may be the first manifestation of some infectious diseases: measles, scarlet fever, rubella measles. Symptoms of pharyngitis may be present with the so-called postnasal drip [8]. Treatment of OF is aimed at eliminating the causative agent of the disease, eliminating inflammation and pain. A group of local and systemic antibiotics, as well as antiseptics, are used as etiotropic therapy. Anti-inflammatory drugs are used as pathogenetic therapy. Symptomatic treatment mainly involves the use of local anesthetics. As is known, inflammation is a local protective-adaptive reaction of the mucous membrane of the paranasal sinuses, aimed at destroying viruses and bacteria. The main components of inflammation: alteration with the release of mediators; vascular reaction with exudation; proliferation.
After phagocytosis of a bacterial antigen by a macrophage, it is destroyed with the release of free radicals and their tissue damage. In response to this, inflammatory mediators are released, causing proliferation of leukocytes, activation of T-lymphocytes and further intensification of inflammation. The main mediators of inflammation include histamine, prostaglandins, leukotrienes and cytokines. Prostaglandins and leukotrienes are the end products of the metabolism of phospholipids in the cell membrane. Hyperfunction of prostaglandins is caused by activation of the enzyme cyclooxygenase (COX). COX-1 has the functional activity of a structural enzyme, is expressed in most cells, and regulates the production of prostaglandins involved in ensuring the normal functional activity of cells. COX-2 is normally absent in most tissues, but its expression increases significantly during inflammation.
To relieve inflammation, it is customary to prescribe non-steroidal anti-inflammatory drugs (NSAIDs), which according to their mechanism of action are divided into 2 groups: 1. Active inhibitors of prostaglandin synthesis (ibuprofen, flurbiprofen, diclofenac) - most active in acute inflammation. 2. Relatively weak inhibitors of prostaglandin synthesis (indomethacin, piroxicam, phenylbutazone) are inactive in acute inflammation, but are very effective in chronic inflammation. When treating OF, preference is undoubtedly given to drugs of group 1. Flurbiprofen, which is the active ingredient, in particular, of the drug Strepsils® Intensive (formerly Strepfen), inhibits the COX enzyme and reduces the synthesis of prostaglandins from arachidonic acid. Flurbiprofen is active against COX-1 and COX-2, which provides a more rapid onset of anti-inflammatory and analgesic effect than selective NSAIDs.
Such drugs are designed to help avoid the systemic effect of NSAIDs by ensuring direct contact of the drug with the mucous membrane of the mouth and pharynx [5]. Drugs that deliver analgesics directly to the pharyngeal mucosa have a number of advantages over systemic analgesics. The patient will feel additional relief due to the physical coating effect of the throat, moreover, the required dose of the active substance taken with local analgesics is lower than when taking systemic analgesics, and the effect occurs quickly [15]. The English company Reckitt Benckiser Healthcare, which has been successfully creating drugs to eliminate HD for more than 50 years, produces flurbiprofen in the form of Strepsils® Intensive lozenges, which allows minimizing the systemic effect of NSAIDs and at the same time ensuring direct contact of the drug with the mucous membrane of the oral cavity and pharynx. Strepsils® Intensive is available in the form of lozenges containing 8.75 mg of flurbiprofen, which has strong anti-inflammatory and analgesic properties due to local inhibition of prostaglandin synthesis. The study results clearly demonstrated that this single dose of the drug is optimal for achieving clinical efficacy while maintaining a good safety profile [16]. The maximum concentration of flurbiprofen in the blood plasma is observed 30–40 minutes after the tablet is dissolved in the oral cavity. The drug is actively metabolized by methylation and hydroxylation, followed by elimination by the kidneys. The main metabolites of the drug are 4-hydroxy-flurbiprofen and 3-hydroxy-4-methoxy-flurbiprofen. Approximately 70% of the dose is excreted in the urine after 24 hours. The half-life is 3–6 hours. The drug is indicated as a symptomatic remedy for reducing GD, including severe GD, in infectious and inflammatory diseases of the oral cavity and pharynx. Clinical trials and large-scale post-marketing studies have established the high effectiveness of the drug, as well as its good tolerability and safety. An additional feature of the drug is the possibility of combined use with antibiotics [11]. Strepsils® Intensive is recommended for adults and children over 12 years of age, 1 tablet every 3–6 hours, but not more than 5 tablets/day. The tablets must be dissolved in the mouth until completely dissolved. The drug begins to act within 2 minutes and is effective for at least 3 hours [13].
Adverse reactions when using Strepsils® Intensive are manifested mainly by a decrease in taste sensations and paresthesia in the form of burning, tingling or tingling. Possible irritation of the oral mucosa. There is a potential, although insignificant, risk of developing adverse reactions that are inherent in NSAID drugs from the gastrointestinal tract, blood-forming organs, and urinary system. Contraindications to the use of Strepsils® Intensive: hypersensitivity to any of the components of the drug; gastric ulcer in the acute phase; bronchial asthma and rhinitis while taking acetylsalicylic acid or other NSAIDs; age under 12 years; pregnancy. The period of breastfeeding is not a contraindication due to the low concentration of flurbiprofen in breast milk when using the drug. Interaction with other drugs: when used together, flurbiprofen may enhance the effect of anticoagulants and weaken the effect of diuretics (furosemide).
To date, the effectiveness and safety of Strepsils® Intensive in patients with GD have not only been demonstrated in clinical studies (CTs), but also confirmed as a result of post-marketing studies. Using a model of severe HD in patients with OF, which is the most sensitive way to assess the effects of local analgesics, BP Schachtel et al. [19] studied the effectiveness of Strepsils® Intensive. The maximum antinociceptive result was observed when using the drug at a dose of 5.0–12.5 mg in another CT (n=301), conducted by N. Watson et al. [15]. The superiority of flurbiprofen at a dose of 8.75 mg compared to placebo was proven in all parameters of assessing the effectiveness of pharmacotherapy, especially regarding the intensity of GD, which decreased within 15 minutes after taking the drug, and the analgesic effect persisted for more than 2 hours. Repeated administration of flurbiprofen reduced or completely eliminated GD throughout the entire 4-day treatment period. The drug was well tolerated. M. Blagden et al. (2002) conducted a clinical trial to study the effectiveness and safety of Strepsils® Intensive in the treatment of patients with HD caused by tonsillopharyngitis in general medical practice, i.e., with repeated administration of the drug, including in combination with antibiotics and other drugs . In contrast to placebo, when using flurbiprofen (8.75 mg) in lozenges, the severity of pain was statistically significantly reduced, both as a result of a single dose of the drug and throughout the study period. A significant advantage of flurbiprofen was also found in patients additionally receiving antibiotics [18].
The high safety profile of Strepsils® Intensive was also confirmed by a study conducted in the UK involving more than 7 thousand patients with GD, which, along with national and international data on monitoring its safety, made it possible to transfer the drug to the group of over-the-counter drugs [19]. The most revealing results are the double-blind, placebo-controlled randomized studies of SI Benrimoj et al. (2001), as well as N. Watson et al. (2000): after taking the first dose, a statistically significant analgesic effect occurred within 15 minutes, lasting at least 2 hours. Subsequent administration of the drug made it possible to achieve a pronounced reduction in symptoms (pain and swelling in the throat on days 2–3) in most patients , and in the group of patients receiving placebo, these manifestations of the disease disappeared at a later date [15, 16]. The trend in world otorhinolaryngology towards the use of topical drugs for the relief of inflammatory diseases is due to the increase in allergenicity in the population of most countries, the high percentage of side effects of systemic drugs and their low effect on inflammatory diseases of the pharynx [7].
Extensive experience in using Strepsils® Intensive has been accumulated in Russia. The drug is highly effective in acute and chronic infectious and inflammatory diseases of the pharynx and, in terms of the totality of symptoms, is at least not inferior to the systemic analgesic paracetamol (500–1000 mg 3–4 times/day, no more than 3000 mg/day), which was confirmed in a study involving 60 patients aged from 18 to 65 years [5]. The analgesic effect of Strepsils® Intensive occurred within 5–15 minutes and lasted about 3 hours, while paracetamol began to act only after 30–45 minutes. Adverse events such as changes in taste and slight tingling sensations that did not require discontinuation of the drug were recorded in only 7 patients. No serious side effects were noted. Considering the high effectiveness and safety of Strepsils® Intensive, A.A. Sedinkin recommends its use to eliminate both severe GD and pharyngeal discomfort and paresthesia in patients with acute and chronic pharyngitis and tonsillitis [5].
R.M. Balabanova, O.V. Stepanets (2004), when comparing groups of patients receiving Strepsils® Intensive or paracetamol, noted that the severity of GD and throat hyperemia on the 4th day of the study, as well as difficulties in swallowing on the 3rd and 4th days of the study were significantly greater among patients receiving paracetamol, which indicates its lower effectiveness against the local inflammatory process in the oropharynx. At the end of the course of treatment, complete recovery occurred in 18 (60%) patients receiving Strepsils® Intensive; in 6 cases (20% of patients), the condition was regarded as incomplete recovery, which, however, did not require additional therapy. In 2 people with ARVI, while taking Strepsils® Intensive, the symptoms of AF were relieved, but catarrhal symptoms persisted, which required the prescription of symptomatic therapy. Antibacterial therapy was required in 4 (13%) patients. In the paracetamol group, recovery was achieved in only 43% of patients, and incomplete relief of symptoms in 47% [6].
Thus, Strepsils® Intensive is an over-the-counter drug used in the complex treatment of acute phases of any etiology. The drug has a powerful anti-inflammatory and analgesic effect, and is well tolerated and demonstrates high clinical efficacy: the therapeutic effect occurs within 15 minutes after taking the first dose and lasts for at least 2–3 hours; a pronounced reduction in symptoms - pain and swelling in the pharynx - is achieved already on the 2-3rd day of treatment. Strepsils® Intensive lozenges (8.75 mg) can be used to treat OF: it is necessary to dissolve the tablet in the mouth until completely dissolved, moving it evenly throughout the entire oral cavity. Adults and children over 12 years of age are recommended to take 1 tablet no more than 5 times within 24 hours, no more than 3 days in a row. Due to local application and the active substance (flurbiprofen), the likelihood of developing side effects characteristic of non-selective NSAIDs is reduced.
Literature 1. Ovchinnikov A.Yu. Acute and chronic pharyngitis // Vestn. otorhinol. 1991. No. 4. pp. 8–10. 2. Lopatin A.S. Treatment of acute and chronic pharyngitis // RMJ. 2001. T. 9. No. 16–17. pp. 58–61. 3. Strachunsky L.S., Kamanin E.I., Tarasov A.A. The influence of antibiotic resistance on the choice of antimicrobial drugs in otorhinolaryngology // Consilium Medicum. 2002. T. 3. No. 8. pp. 352–357. 4. Kryukov A.I., Sedinkin A.A. Materials of the Russian Conference of Otorhinolaryngologists. M., 2002. pp. 362–363. 5. Sedinkin A.A., Balandin A.V., Dimova A.D. Results of an open prospective controlled randomized comparative study of the effectiveness and tolerability of flurbiprofen (strepfen) lozenges and paracetamol in patients with sore throat in acute infectious and inflammatory diseases of the upper respiratory tract // Bulletin of Otorhinolaryngology. 2004. No. 5. P. 52–54. 6. Balabanova R.M., Stepanets O.V. Study of the effectiveness and safety of Strepfen (flurbiprofen) for sore throat in comparison with paracetamol // Consilium provisorum. 2004. No. 4. pp. 40–42. 7. Egorova O.A. The feasibility of using local antimicrobial drugs in the treatment of upper respiratory tract infections // Farmateka. 2006. No. 5. pp. 107–109. 8. Pluzhnikov M.S., Panova N.V., Levin M.Ya., Lavrenova G.V., Afanasyeva I.A. Pharyngitis (clinical and morphological aspects and cryosurgery) / ed. M.S. Pluzhnikov. St. Petersburg: Dialog, 2006. 120 p. 9. Shpynev K.V., Krechikov V.A. Modern approaches to the diagnosis of streptococcal pharyngitis // KMAH. 2007. T. 9 (1). pp. 20–33. 10. Ryazantsev S.V. Etiopathogenetic therapy of acute pharyngitis. Guidelines. St. Petersburg, 2007. 40 p. 11. Luchsheva Yu.V., Izotova G.N. Local therapy for pharyngitis // Breast cancer. 2011. T. 19. No. 6. P. 420–426. 12. Dagnelie CF Sore Throat in General Practice. A Diagnostic and Therapeutic Study. // Thesis. Rotterdam, 1994. 13. Gwaltney JM Pharyngitis // In: Mandell GL, Bennet JE, Dolin R., editors. Principles and Practice of Infectious Diseases. 4th Edition. NY: Churchill Livingstone. 1996, pp. 566–569. 14. Cowan DL Acute and chronic infection of the pharynx and tonsils / DL Cowan, J. Hibbert / Scott–Brown's Otolaryngology, Sixth edition. Oxford, 1997. Vol. 5. Chapter 4. P. 1–24. 15. Watson N., Nimmo WS, Christian J.E.A. Relief lozenge flurbiprofen 8.75mg: randomized, double-blind, placebo-controlled stage of efficacy and safety // Int J Clin Pract. 2000. Vol. 54 (8). R. 490–496. 16. Benrimoj SI, Langford JH, Christian J. et al. Efficacy and tolerability of the anti-inflammatory throat lozenge Flurbiprofen 8.75 mg in the treatment of sore throat // Clin Drug Invest. 2001. Vol. 21(3). R. 183–193. 17. Bisno AL et al. Practice guidelines for the diagnosis and management of group A streptococcal pharyngitis. Infectious Diseases Society of America // Clin Infect Dis. 2002. Vol. 35. R. 113–125. 18. Blagden M., Christian J., Miller K., Charlesworth A. Multidoseflurbiprofen 8.75 mg lozenges in the treatment of sore throat: a randomized, double-blind, placebo-controlled study in UK general practice centers // Int J Clin Pract . 2002. Vol. 56(2). R. 95–100. 19. Schachtel BP, Homan HD, Gibb JA, Christian J. Demonstration of dose response of flur-biprofen lozenges with the sore throat pain model // Clin Pharmacol Ther. 2002 May. Vol. 71. (5). R. 375–380. 20. Bloomington MN Acute pharyngitis // Institute for Clinical Systems Improvement (SCSI). 2005. R. 33–50.