A salivary gland ranula (sublingual ranula) is an oral cyst located at the exit site of the salivary gland ducts, although it can occur anywhere in the sublingual region. According to the classification, it belongs to retention cysts; its formation is caused by blockage of the sublingual or submental salivary gland. There is no consensus on the nature of this pathology; many doctors associate the appearance of ranulas with the influence of some pathogenic factor on the gland ducts: mechanical damage or inflammation with subsequent blockage.
Causes
The mucous membrane of the mouth is a fairly resistant surface to various influences. But when it is injured, or an imbalance occurs in the body due to diseases, an inflammatory process can occur, which leads to the formation of a bubble under the tongue. Other problems can also be the main causes of pathology.
Injury
Mechanical disruption of the salivary duct of the gland leads to the thickening of the connective tissue and this causes the appearance of a ball under the tongue. A toothbrush with rough bristles, fish bones, a chipped tooth, a toothpick, breaking the cover, activates inflammation.
Antihygiene
In this case, a blister under the tongue appears due to failure to observe basic oral hygiene. This could be someone else's toothbrush, spoons, forks, or rare care.
Syphilis
This disease tends to negatively affect the condition of the mucous membranes, causing tumors.
Complications after illness
The bubble occurs after suffering from mumps, sore throat, or influenza. The salivary gland swells, and against the background of this, stagnation of secretion occurs.
Infection
Microtraumas that occur on the mucous membrane can be infected with bacteria and microbes, fungus, which leads to the formation of an inflamed blister.
Oncology
The disease provokes the formation of a tumor that puts pressure on the area under the tongue. In the early stages, the disease goes unnoticed, but over time, saliva production decreases and a transparent cyst appears, which eventually grows to 3 centimeters.
Food and medicine
A blood ball under the tongue appears for the following reasons:
- Injury that occurs from biting the mucous membrane while eating.
- Chemical burn.
- Hot food or drink.
- Medicines.
- Spicy and salty foods.
- Blocking the duct with a stone.
Ranula
A ball under the tongue can cause ranula. It appears against the background of an inflammatory process in the sublingual area or when the normal functioning of the salivary gland is disrupted. Initially, the disease manifests itself as a bluish discoloration in the oral cavity. After which a bubble appears, which after some time bursts and is observed again in the same place.
On this topic
Find out what to do if a pimple on your tongue hurts
- Olga Alexandrovna Novikova
- August 30, 2022
Experts still cannot establish the causes of this disease. Some believe that the pathology arose against the background of an inflammatory process, while others suggest that these are epithelial inclusions of germinal origin. That is, the tumor is a cystic epithelial neoplasm.
The pathology develops against the background of blockage of the salivary gland duct and does not allow saliva to be released into the oral area. This leads to the fact that it accumulates in the gland, which increases to 5 cm in diameter. After which the formation is ruptured on its own or opened by a surgeon using a scalpel.
The ranula looks like a bubble with a clear liquid, which does not cause pain, but brings discomfort to the patient in the oral mucosa.
Aphthous stomatitis
Aphthous stomatitis is also one of the causes of a bubble under the tongue. This is an inflammatory process that occurs in the area of the oral mucosa, which is manifested by the appearance of aphthae. Aphthous stomatitis is a common disease and can be treated by a dentist. The main factors in the occurrence of pathology are:
- disruptions in the functioning of the immune system;
- viruses;
- hormonal fluctuations;
- heredity;
- allergic reactions;
- diseases of the digestive tract;
- diseases of the gums and teeth;
- injuries;
- lack of nutrition;
- hypovitaminosis;
- stress, depression, nervous tension;
- accompanying illnesses;
- violation of personal hygiene rules.
Aphthous stomatitis is very common in young children, especially during teething. At this point, you should definitely consult a doctor.
NORMAL ULTRASONIC ANATOMY
Parotid glands
The parotid glands, which are the largest of the salivary glands, are enclosed in a separate fascia, which penetrates the glands, forming various lobules. In cross-section, the parotid gland is a sharply defined, homogeneous organ with intermediate echogenicity (Fig. 1).
Rice. 1. Normal parotid gland.
The gland can be clearly distinguished from subcutaneous adipose tissue. The anterior part of the gland sits on the masticatory muscle and can be differentiated from the buccal adipose tissue, which has lower echogenicity, by contraction and relaxation of the masticatory muscles. The posterior part of the gland is located in the retromandibular fossa and is clearly delimited anteriorly by the ascending ramus of the mandible, and posteriorly by the sternocleidomastoid muscle and the mastoid process. Mediocaudal to the inferior pole of the parotid gland, the posterior belly of the digastric muscle and the internal carotid artery can be distinguished. It is important to remember that a small portion of the parotid gland may be hidden by the acoustic shadow of the mandible.
In and around the gland, the internal jugular vein and the retromandibular vein can be found, which are located in the glandular parenchyma and can be visualized, especially in the longitudinal projection. In transverse views, distal to the retromandibular vein, the styloid process is projected onto the glandular parenchyma, which should not be confused with sialolithiasis. The facial nerve is usually not visible. However, with the use of modern high-resolution transducers, it is sometimes possible to obtain a sonographic image of the main outflow canal.
Submandibular gland
The submandibular gland extends cranial to the mandible and the geniohyoid muscle and has a close connection with the anterior belly of the digastric muscle. The submandibular gland forms an arch around the posterior border of the geniohyoid muscle and often reaches ventromedial to the submandibular gland. Echogenic structures with an element of acoustic shadowing are often projected in the area of the gate of the submandibular gland. In this area, it is necessary to carry out differential diagnosis between the elements of the hyoid bone and the sialoliths of the submandibular gland, which may have comparable characteristics on imaging [2,7]. Sonographic imaging characteristics of the submandibular gland include an intermediate echogenic structure with a regular echo pattern corresponding to the echo pattern of the parotid gland parenchyma (Fig. 2).
Rice. 2. Normal submandibular gland.
In and around the gland, the facial artery and facial vein, which pass through the gland, are easily distinguished sonographically. The path of the efferent duct can sometimes be visualized using high-resolution ultrasound probes, even in the absence of duct obstruction. If we are talking about differentiation of the elements of the hyoid bone, then during swallowing movements its displacements are observed.
Sublingual gland
Visualization of the sublingual gland can sometimes be problematic. The sublingual gland is located under the mucous membrane in the oral cavity, lower in the projection of the tip of the tongue, next to the frenulum of the tongue. The dorsal part of the glands often touches the surface of the submandibular gland.
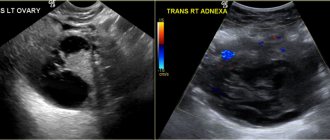
The gland is bounded ventrally and medially by the geniohyoid and genioglossus muscles, and caudally by the mandible. Short excretory ducts usually cannot be visualized. Accumulation of saliva may be found in and around the sublingual gland, which forms the ranula (Figure 3).
Rice. 3. Sublingual ranula.
Symptoms
Symptoms of the pathology depend on the reason for which it arose.
With injuries in the tongue area, blisters may appear not only under the tongue, but also on the side. It is mainly pink in color or engorged with blood, which is visible to the naked eye.
If any blood manifestations are absent, then this indicates the superficial nature of the pathology; most often, such a bubble goes away on its own and does not cause noticeable harm to health. When a blood clot appears, the hematoma is very deep and can become a breeding ground for pathogenic bacteria, most often this leads to an inflammatory process.
On this topic
How to quickly get rid of a pimple on the gum
- Maria Konstantinovna Tevs
- July 29, 2022
A small bubble that has popped up may be the cause of vitamin deficiency. In this case, the patient feels almost no discomfort. Such manifestations disappear within a few days. To prevent the bubble from appearing again, you need to reconsider your diet and enrich your diet with vegetables, fruits, meat and dairy products. It is also recommended to undergo a course of treatment with vitamins.
Why does it occur
Due to various life situations, suppuration may appear, which is expressed in the form of a popping up ball or a water bubble under the tongue or above it. This may be directly related to both internal and external changes in the body.
Damage to the tongue, or rather to its joint, is the most common cause. This injury can have completely different consequences.
Below we will talk about the three most popular reasons:
- Thermal. If there is a sudden change in temperature while eating or drinking liquid, the tongue may become damaged. Eating food that is too cold or hot will cause irritation. Subsequently, a small bubble or bump may appear on the tongue. Often, it will go away on its own within a few days.
- Mechanical impact. When the mucous surface of the tongue is damaged. This often happens when eating fish meat, which contains quite a lot of sharp bones. It happens that you won’t notice much damage right away, but after a few days a ball will form at the site of the wound. This also includes independent tongue bites.
- Chemical exposure. Increased consumption of salt or various spicy seasonings can also lead to inflammation. The result is inflammation.
The resulting ball can be of completely different consistency. The severity of the injury directly affects this. Often on the first day after damage, a small bump of a light shade or bright red appears.
During the examination, the doctor spends a lot of time on pain, inflammatory tone, its shape and, of course, location. When the gastrointestinal tract is disrupted, the body causes a reaction that can affect the rash of small bubbles on the surface of the tongue.
Ranula
At an early stage, a bubble may appear, which will not bother you at first. This bubble can easily be accidentally burst using your teeth. It contains a clear liquid inside. If you accidentally pierced it, this does not mean that the problem is solved.
Ranula is a chronic pathology and must be carefully treated. This disease is also called a sublingual cyst, and is popularly called a frog tumor. One of the unpleasant aspects is that ranula has relapses.
Today there are many different creams and gels in the pharmacy that can be used to get rid of ranula. But this will only relieve the symptoms, and the real problem must be solved with a specialist. The doctor will prescribe a course and method of treatment.
Hematoma
When you get an injury to a cyst, a red lump forms at this place, which has a painful effect. The obvious sign of a hematoma is redness, because the redness is the result of a blood clot in the injured area. Due to the resulting injury, the cheek may also be damaged.
After damage to the vessels, the hematoma stage begins. At first, only a transparent blister may appear, since the blood has not yet had time to collect inside it or the damage is not significant. If this is the second option, then within a couple of days it should go away on its own. Otherwise, you will need to be examined by a doctor.
The most important thing is to establish the causes of your disease, and then draw some conclusions and begin treatment.
Below we have outlined several main points that your doctor will first pay attention to:
- The exact location of the tumor;
- What color and density is the cone;
- Size;
A tumor can occur as a result of a protective reflex of the body. A blood bubble forms in its place. In the best case, it will pass without surgical intervention, but if five days is not enough to solve this problem, then do not waste time and contact a specialist. He will examine and make the correct diagnosis to avoid dangerous pathology.
For this disease, doctors recommend taking a preventive course, which includes taking minerals and vitamins. You need this to strengthen your blood vessels. The lump is only pierced if it interferes with your eating. Otherwise, this is not recommended.
Why does a rash appear on the oral mucosa in children? The answer is here.
Stomatitis
There are a lot of reasons for the appearance of stomatitis. Often due to your neglect of the oral cavity and teeth. The human mouth is like a bait for bacteria; many different infections get there, to which the body can respond in the form of stomatitis.
It should be noted that the main weapon against this disease is personal hygiene. If you are okay with this, then in most cases this problem will bypass you.
Young children suffer the most because of this, when they put everything they see in their mouths. If we take the statistics of this disease, then every fifth person suffers from this disease.
Below are a number of other reasons why stomatitis may appear:
- Sharp teeth that rub the tongue and cause irritation;
- Intestinal function is disrupted;
- Women have an unstable metabolism during pregnancy;
- Having a cold or flu;
- The appearance of worms in the body;
- Lack of vitamins in the body;
- Excessive consumption of alcohol and tobacco products.
Diagnostics
If a bubble appears in the sublingual area, you should definitely consult a doctor, as this may signal disturbances in the functioning of the body and dangerous diseases. The specialist is obliged to carry out diagnostic measures that will help find the causes of the pathology:
- Study of all symptoms and complaints.
- Determining the presence of chronic diseases and injuries in the oral cavity.
- External examination of the tongue.
- Laboratory tests of blood and saliva.
- Puncture of the contents of the bladder under the tongue.
- Examination by a dentist.
The specialist analyzes the results and prescribes the correct treatment, in some cases surgery.
Other signs
The most common reasons for the appearance of a lump on the surface of the tongue are the above diseases: hematoma, stomatitis and ranula, but in addition to these diseases there are a number of others.
Below we list the main reasons:
- Lipoma. A rounded flat shape appears on the tongue. Often located slightly further than the middle of the tongue. Quite a rare disease. At the beginning there are no painful effects, but over time the lump can grow several times larger and discomfort in the oral cavity will be felt. You won't be able to remove a lipoma on your own. This will require the help of a specialist.
- Papilloma. A lump that appears on absolutely any part of the tongue and has a grayish light gray tint. This disease is transmitted through sexual intercourse, excessive consumption of alcohol, tobacco products, and also due to stress.
- True pemphigus. Not uncommon in infants. The main symptom of this serious disease is many small blisters on the surface of the mucous membrane of the tongue. This disease can be transmitted from mother to child, as well as due to disorders of the autoimmune system.
Drug treatment
Therapy for a bubble under the tongue is prescribed depending on the causes of its occurrence:
- For aphthous stomatitis, a number of antiseptic drugs are used; physiotherapy and mouth rinsing using decoctions of medicinal herbs such as calendula and chamomile are also recommended. The affected area is periodically treated with sea buckthorn oil.
- In case of infectious diseases, the cause of the disease is initially eliminated: herpes - Acyclovir; candidiasis - antifungal medications Clotrimazole, Fluconazole, Flucostat; glossitis - anti-inflammatory drugs, antibiotics; syphilis - antibacterial therapy: Tetracycline, Macrolide, Penicillin.
- In case of vitamin deficiency , the diet changes and a number of vitamin complexes are prescribed.
- For endocrine diseases and disorders, hormones are prescribed, after special tests have been carried out.
- Neoplasms and cysts are removed surgically. After removing the blisters, a course of treatment with antibacterial and anti-inflammatory medications is carried out.
The following medications are also used:
- Lorgexidine is an antimicrobial agent used to irrigate the oral cavity.
- Miramistin has an antiseptic effect.
- Stomatophyte is an anti-inflammatory agent.
- Proposol relieves pain.
- Cholisal-gel – reduces pain, fights inflammation.
- Metrogyl denta is an antimicrobial and antiseptic agent.
- Actovegin-gel – accelerates the healing process.
Causes of a lump under the tongue
A tumor can occur for various reasons. Usually this is mechanical damage to the mucous membrane and inflammation during chewing of hard foods. In this case, the lump will disappear on its own after some time.
On this topic
What could be a growth on the gum?
- Olga Alexandrovna Novikova
- September 3, 2022
Other reasons for the formation of tumors under the tongue include:
- Wearing low-quality dentures. Sharp edges can injure the surface of the mucous membrane.
- Infections. They get into microcracks formed as a result of injury and become the cause of inflammation. If left untreated, the process affects the deep layers of the mucosa, and a tumor begins to form.
- Salivary stone disease. The lump occurs in the area where the stone is formed.
- Genetic predisposition.
- The first stage of syphilis. A ball forms under the tongue, which causes pain when pressed or during conversation. After a while he disappears.
A tumor under the tongue can form against the background of the development of oncological pathologies. That is why it is important to promptly contact a specialist who will determine the cause and nature of the disease.
Frog bladder - ranula under the tongue: what is it and how to treat it?
Ranula (lat. ranula; from rana - frog) under the tongue, sublingual retention cyst - a tumor-like formation of the anterior floor of the mouth.
The name has been preserved since ancient times due to its similarity in appearance to the pharyngeal bladder of a frog.
A salivary gland ranula (sublingual ranula) is a cyst in the oral cavity, located at the exit of the salivary gland ducts, although it can occur in any part of the sublingual region.
According to the classification, it belongs to retention cysts; its formation is caused by blockage of the sublingual or submental salivary gland.
There is no consensus on the nature of this pathology; many doctors associate the appearance of ranulas with the influence of some pathogenic factor on the gland ducts: mechanical damage or inflammation with subsequent blockage. When it reaches a large size, it interferes with eating (especially in children).
Symptoms of a ball appearing under the tongue
Below are the symptoms by which you can independently determine whether a given lump (under or above the tongue) is a cyst:
- The area under the tongue is inflamed;
- Noticed a transparent water bubble;
- Also, this bubble may have a tint of blue;
- It is easy to burst or crush;
- After it bursts, another one appears in the same place.
Causes of ranula formation
Among all diseases of the oral cavity, a cyst under the tongue is considered one of the most problematic and common, as it progresses quite quickly and causes severe discomfort. It is not advisable to ignore this problem, because the larger the cyst, the higher the risk of its spontaneous rupture with subsequent relapse of the disease.
The mechanism by which ranula occurs is that a blockage of the salivary gland duct (usually Bartholin's or Wharton's duct) prevents the resulting saliva from entering the oral cavity. It begins to accumulate in the gland, which gradually increases in size, at times reaching five centimeters in diameter.
Summary
Ultrasonography has established itself as the primary imaging technique in the diagnosis of salivary gland diseases. Sonographic examination is usually sufficient to diagnose sialolithiasis. If chronic sialoadenitis or sialoadenosis is suspected, and sonographic data are insufficient, standard sialography may be required in some cases. A histological examination is necessary as soon as the diagnosis of a neoplasm is established. If the tumor's enlargement and connection with surrounding tissues cannot be determined sonographically, subsequent computed tomography or magnetic resonance imaging should be performed. To conduct research, we recommend using a device from GE Voluson E8 .
Classification
Based on their location, ranulas are divided into superficial and diving.
- Superficial ranulae form directly on the oral mucosa, forming characteristic bulges (bubbles) under the tongue.
- Diving ranulas are called that way because they are located a little deeper, hiding behind the mylohyoid muscle. This type of ranula cannot be detected by visual examination of the oral cavity; patients with this pathology experience a swelling or lump under the chin, which is sometimes confused with an enlarged lymph node.
Ranulas are also divided according to their structure: true (retention) cyst, false (post-traumatic) and mucocele.
- A true, or retention cyst, occurs due to a violation of the outflow of secretions and various pathologies of the glands.
- False (post-traumatic) most often forms after soft tissue injury.
- A mucocele is a cavity-like cyst-like formation containing mucus.
Few people think about the fact that the salivary glands are extremely susceptible to various inflammatory and other pathologies.
Salivary gland cyst - a detailed analysis of the disease. You can read about the reasons for the formation of stones in the salivary glands here.
Do you know what sialolithiasis is? If interested, read the information at the link.
PATHOLOGICAL RESULTS
Box 4 contains a short list of variants of salivary gland pathology.
| Box 4 Variants of pathology of the salivary glands
|
Acute sialadenitis
Since we have to deal with paired organs, it is important to compare both glands in one picture. Characteristic findings are explained by inflammatory edema and an increase in fluid content in the parenchyma, which is transformed during inflammation. Typically we see the following:
- Diffuse expansion of the entire affected gland.
- The organ can be clearly demarcated from adjacent structures.
- The structure of the parenchyma appears loose, heterogeneous, coarsely textured and more hypoechoic.
- Limited hypoechoic formations can be detected as a concomitant inflammatory reaction of the intraglandular lymph nodes.
- Zones of liquefaction (as signs of abscess formation) are visualized as hypoechoic with a hyperechoic surrounding wall and pronounced distal signal enhancement.
- Coarsely structured hyperechoic echoes at the center of such liquefaction lesions may correspond to areas of necrotic tissue.
Chronic sialadenitis
Sonographic imaging is highly dependent on the duration and degree of inflammation of the glandular parenchyma. As in the case of acute sialadenitis, a conclusive differential diagnosis between the various pathogenic forms of chronic sialadenitis cannot be made using sonography alone. Typically we see the following:
- A clear increase in the unevenness of the echo texture.
- The internal structure has a heterogeneous pattern, most likely due to fibrotic changes in the parenchyma.
- Small cystic echo lesions are formed, which correspond to limited ductal ectasia (Fig. 4).
- Sometimes stones within the gland are identified as echogenic structures with a distal acoustic shadow.
Rice. 4. (A) Chronic sialadenitis of the parotid gland. (B) Sialocele of the parotid gland. (C) Dilatation of Stenson's duct (arrows).
Differential diagnosis is important in the following situations:
- Patients suffering from Gougerot-Sjögren syndrome have sonographic signs of enlarged, heterogeneously structured, hypoechoic salivary glands. Numerous limited hypoechoic formations are found inside the parenchyma, which may be associated with cystic dilatation of the ducts, on the one hand, or with enlargement of intraglandular lymph nodes, on the other hand. Sonographically, the structure of the salivary glands looks like a “cloud”.
- Sialadenitis of epithelioid cells (Heerford syndrome) is sonographically characterized by a rich echo pattern interrupted by numerous enlarged lymph nodes that appear as hypoechoic masses.
- Kütner's tumor of the submandibular gland is visualized as a formation with an indistinct echo signal in a certain part of the submandibular gland, which is easily mistaken for an adenoma.
- Ultrasound helps detect changes after radiation therapy. The echohomogeneous pattern disappears after irradiation, with a more hypoechoic and sometimes irregular pattern being a sign of loss of function.
- Other secondary pathological changes (edema, infections and soft tissue tumors) around the salivary glands are easily distinguished from primary salivary gland pathology.
Parotid abscess
The evolution of the inflammatory process is characterized by a hypo-, anechoic lesion with irregular edges. Typically we see the following:
- Hypo-, anechoic lesion with irregular edges.
- Peripheral hypervascularization, which is determined by color Doppler scanning.
- In the case of partial necrotic changes, lymph nodes with anechoic areas of necrosis are identified.
- In the case of fistula formation, a fistula is defined that reaches the skin surrounded by edematous tissue.
An important initial sign of an abscess is the appearance of vessels with a linear and fairly regular direction, which subsequently changes to a more irregular one, and is characterized by numerous anastomoses, which can be determined by an increase in the intensity of the color Doppler signal. In abscesses, the color Doppler signal has a peripheral structure because in this case the vessels are intertwined along the periphery of the abscess.
Enlarged lymph nodes
Lymph nodes may be found inside the parotid gland. However, only around the submandibular gland, due to the characteristics of embryological development. In the parotid gland, a group of small lymph nodes (3-5 mm) is located along the retromandibular vein. These lymph nodes carry out lymph drainage from the Eustachian tube, external auditory canal and deep areas of the face. Intraglandular and extraglandular lymph nodes normally do not exceed 9 mm in diameter.
Ultrasound imaging of otherwise unremarkable glandular parenchyma may reveal predominantly multiple hypoechoic lesions that often lack any distal signal enhancement. Sonographically, as a rule, it is impossible to obtain reliable signs that would allow a definitive differential diagnosis between benign and malignant enlarged lymph nodes.
Reliable differential diagnosis between reactive lymphadenitis (Fig. 5), non-Hodgkin's lymphoma (Fig. 6), MALT lymphoma, or intraglandular metastatic spread is not possible on the basis of sonographic findings alone.
Rice. 5. Pathological lymph node.
Rice. 6. Primary lymphoma of the parotid gland.
Clinical signs, number, location, and sometimes texture of nodes can lead to diagnosis, but do not replace histological analysis. As with enlarged lymph nodes of the neck, some authors mention the so-called “hilus” (gate) as a sign of reactive lymphadenitis.
Cystic tumors
Congenital or acquired salivary gland cysts are usually filled with clear fluid. We usually see an echo-negative tumor with clear borders and distal signal enhancement (Fig. 7).
Rice. 7. Salivary gland cyst (arrows indicate parotid gland, arrowheads indicate cyst).
It is important to note that if cystic tumors are detected sonographically in both parotid glands, and if there is a relevant medical history, then lymphoepithelial cysts caused by HIV infection should be suspected.
Sialolithiasis
Although the sign of a distal acoustic shadow is usually detected, the signal reflection can sometimes be unclear or insufficient. This phenomenon is the result of a reflected ultrasonic component that does not reach the transducer but is scattered out of the image plane. Typically, we see an echo-opaque object with a clear sign of a distal acoustic shadow (Fig. 8) and dilatation of the excretory ducts.
Fig.8. Intraglandular sialolithiasis of the submandibular gland.
Parotid duct stones contain organic components and are visualized with great effort. Sometimes only a distinct echo-opaque object without a distal acoustic shadow may be detected. However, in many of these cases, dilatation of the efferent ducts of the salivary glands can be considered as another indirect sign of the development of sialolithiasis, if the stone cannot be clearly identified. However, dilation of the duct can also be caused by scar changes in the connective tissue (for example, the situation after an inadequately performed incision of the duct or after acute inflammation). Stones with a diameter of 1.5 to 2 mm or more, located in the area of the large salivary glands, can be reliably detected during sonography.
It is important to note that the precise determination of the position of sialoliths (intraglandular, extraglandular and intraductal) is of great importance. Differential diagnosis is important both in the presence of air inside the ducts and in the case of pneumoparotitis, foreign bodies, angiolithiasis and calcified lymph nodes or arteriovenous malformations (Fig. 9).
Rice. 9. Arteriovenous malformation of the salivary glands.
Remember, because of its limited sensitivity and limited negative predictive value, sonography does not reliably exclude small salivary gland calculi. Further diagnostic studies are needed to identify stones in patients with normal sonographic findings and suspected lithiasis.
Sialadenosis (sialosis)
All large salivary glands can be simultaneously affected by sialoadenosis. Sialadenosis is a non-inflammatory condition characterized by bilateral enlargement of the salivary glands, most commonly the parotid glands. Usually we see that the glands look indistinctly enlarged, are difficult to differentiate from surrounding structures, their echo structure looks homogeneously hyperechoic, and with sialoadenosis tumor-like lesions are not detected. In some cases, the parotid gland is so enlarged that ultrasound requires a low-frequency transducer to evaluate the deep part.
Benign epithelial tumors of the salivary glands
A well-defined boundary between the surrounding salivary gland tissue and the tumor itself is a characteristic feature of a benign salivary gland tumor. Because ultrasound is unable to visualize nerves, the relationship of parotid tumors to the facial nerve cannot be reliably determined.
Pleomorphic adenomas have a homogeneous/hypoechoic texture. However, sometimes heterogeneous structures with hard and cystic inclusions may be noticeable. In these cases, a characteristic feature is distal signal enhancement (Fig. 10).
Rice. 10. Pleomorphic adenoma of the parotid gland.
Monomorphic adenomas (adenolymphomas) may also appear sonographically homogeneous and hypoechoic, as is the case with pleomorphic adenomas. If the proportion of cystic structures is high, adenolymphoma may also present completely without echo with extensive distal enhancement. Occasionally, septae may be identified within the tumor.
The remaining less common types of benign salivary gland tumors (eg, basal cell adenomas, oncocytomas, lymphoepithelial lesions) also have similar nonspecific sonomorphological features.
Definitive sonographic identification and differential diagnosis between different types of benign salivary gland tumors is currently impossible, although significant cystic portions in the mass tend to indicate adenolymphoma, and the absence of cystic areas indicates pleomorphic adenoma. To a certain extent, parotid tumors can be classified as either the "superficial" or "deep" part of the gland.
Benign nonepithelial tumors of the salivary glands
Lymphangiomas and hemangiomas (Fig. 11 and 12) have similar sonomorphological characteristics, which makes differential diagnosis between them impossible.
Rice. 11. Intraglandular lymphangioma.
Rice. 12. Submandibular hemangioma.
During the study, loosely connected alveolar structural components, consisting partly of hypoechoic and hypergeogenic areas, can be detected. Sonographic examination allows us to assess the depth of penetration and spread of this tumor into the corresponding salivary gland and into the area of surrounding soft tissue.
Intraglandular and extraglandular lipomas (Fig. 13) appear as sharply demarcated, ovoid formations, with a hypoechoic and homogeneous signal reflection pattern.
Rice. 13. Well-defined lipoma.
Lipoma has a more characteristic hypoechoic reflection pattern than the rest of the salivary gland parenchyma, but its echo texture is more hyperechoic than other types of intraglandular tumors, and it also has a linear hyperechoic feathery texture.
Malignant tumors of the salivary glands
We typically see a fuzzy edge and a patchy echo texture. It is possible to describe the relationship between invasive tumor growth and surrounding tissue. It is impossible to detect involvement of the facial nerve in the malignant process. The most common malignant tumors of the salivary glands are mucoepidermoid carcinoma, adenoid cystic carcinoma, carcinoma arising in pleomorphic adenoma, and distant metastases (Fig. 14).
Rice. 14. Metastatic melanoma in the parotid gland (arrows indicate parotid glands, arrowheads indicate metastases).
Indications for sonographic examination are sometimes absent, since at the preoperative stage it is impossible to identify with complete certainty the benign or malignant nature of tumor development. If a malignant process is suspected, ultrasound-guided fine-needle aspiration biopsy can be a useful tool to more accurately classify the tumor at a preoperative stage.
It is important to note that if tumor margins cannot be accurately imaged by sonographic examination, especially when the tumor extends to osseous or deep structures, the patient's diagnostic imaging should be extended in any case to computed tomography and/or magnetic resonance imaging.
Gougerot-Sjögren syndrome
Gougerot-Sjögren syndrome occurs when lymphocytes invade and destroy the exocrine gland. It is the second most common autoimmune syndrome after rheumatoid arthritis, affecting the salivary glands in 40-80% of cases. This results in a higher incidence of parotid lymphomas and salivary stone disease. Typically we see the following:
- At an early stage, sonography is normal.
- Later, the glands become enlarged and large-scale structural damage occurs.
- The gland is heterogeneous.
- At a later stage, sonographic examination reveals sialoectasia and marked hypervascularization on color Doppler ultrasonography of the salivary glands.
The intraoperative role of sonography has become important since the introduction of minimally invasive surgical techniques in salivary gland surgery. During surgery, if endoscopic observation of the surgical field is not possible, sonographic guidance can be used to:
|
Rice. 15. Minimally invasive procedures under ultrasound guidance.
Rice. 16. Therapeutic intraglandular injection of Botox.
Color Doppler ultrasonography of the salivary glands
The standard B-scan is a well-established tool for diagnosing salivary gland diseases. For tumors located in the salivary glands, there is increasing interest in non-invasive collection of clinical information such as growth and invasiveness, as well as making an accurate diagnosis before surgery. Before the benefits of sophisticated ultrasonography became available, standard testing was performed by correlating simple sonomorphological criteria, such as anechoic areas, with specific histological features. This can be easily achieved even if you buy a portable ultrasound machine .
Over the past few years, color Doppler sonography has become well established as an integral part of head and neck, ENT and maxillofacial surgery, especially as part of the preoperative evaluation of tumors and cervical lymph nodes.
Color duplex sonography
Color duplex sonography (Box 5) is a combination of B-mode sonography, pulsed Doppler sonography, and color coding of perfusion areas. The basic principle of color duplex sonography is the frequency shift of the transmitted signal, which is caused by reflection from moving red blood cells. The speed and direction in which red blood cells approach and move away from the transducer provide the information needed to perform duplex sonography.
| Box 5 Color duplex sonography
|
The ability to use Doppler signal amplifiers to achieve improved visualization of tumor vascularization has provided new opportunities for tumor characterization. Analysis of microvascularization and time-dependent changes after Doppler amplifier insertion, as well as elastography, are promising new tools for identifying features that help determine whether specific changes are typical for certain types of salivary gland tumors (Fig. 17).
Rice. 17. Study of the salivary glands using power Dopplerography.
The diagnostician should know the following:
|
Treatment of ranula with folk remedies
The traditional treatment method is surgical removal of the ranula.
A dentist or maxillofacial surgeon, using a scalpel under local anesthesia, first drains the ranula (releases fluid) and then removes it from the bed.
This is necessary to prevent recurrence of the cyst.
Sutures are placed on the edges of the wound, which dissolve after a few days. The whole procedure takes a little more than half an hour. The question of whether the ranula needs to be removed is decided individually together with the attending physician.
Ranula can only be eliminated surgically. It is preferable to remove the cyst after making an incision in the oral mucosa. In cases where it is impossible to completely remove the cyst, only its anterior wall is excised, the cyst cavity is lubricated with tincture of iodine and tamponed for 5-7 days.
The timing of the operation depends on the size of the cyst. If there is difficulty swallowing or breathing, surgical intervention is carried out immediately upon diagnosis, including in infants. In the postoperative period, oral toilet is prescribed.
Like any cyst, a ranula can be removed surgically.
But this is not always necessary. To get started, you can try a few folk remedies.
Mix two tablespoons of eucalyptus essential oil and 200 ml of boiled water. Rinse your mouth with the resulting solution 3-4 times a day.
Also, eryngium herb is often used to rinse the mouth. Pour 200 ml of boiling water over a tablespoon of the mixture and leave for about 2 hours. Afterwards, the broth needs to be cooled and strained.
Baking soda solution
Mix ½ teaspoon of soda and 200 ml of warm boiled water, add the same amount of iodized salt. You can also use a weak solution of potassium permanganate or furatsilin for rinsing.
Healing decoction of pine needles
Boil a liter of water, add 5 tablespoons of young pine needles to it and boil for about 30 minutes. Then cool, strain and take orally 2 times a day.
The main feature of salivary gland cysts is that they can be asymptomatic for a very long time. Parotid salivary gland cyst - the clinical picture of the pathology is described in the article.
The anatomy of the salivary gland is described in detail in this material.
Oak bark decoction
Pour 300 g of dried oak bark with a glass of boiling water.
Leave in a water bath for half an hour, strain the resulting broth and bring with boiled water to a volume of 300 ml.
Rinse your mouth 3-4 times a day, store the broth for no more than two days.
Lemon juice rinse
Squeeze the juice from three lemons and leave in the refrigerator for 48 hours. Grind the remaining zest with 33 cloves of garlic. Pour the resulting mixture with two liters of boiled water and place in a warm place for a day. Then strain and add lemon juice. Rinse your mouth five or more times a day.
What does the appearance of a lump under the tongue mean, and how to deal with such a problem
The oral cavity is a complex structure and functioning of the human body. It contains different structures that closely interact with each other. Therefore, a lump under the tongue will be detected immediately - as a foreign body in the oral cavity. Making a diagnosis and choosing the optimal treatment is the prerogative of the dentist. It is this doctor who should deal with diseases of the sublingual area. Self-medication can lead to serious complications.
Rehabilitation, prevention and prognosis
In the postoperative period, special attention is paid to oral hygiene. Teeth brushing is done with the utmost care. Do not damage the mucous membrane with a toothbrush. At first, you should follow a diet: sour, spicy, carbonated foods are prohibited.
Excessively cold and hot foods should be avoided.
During rehabilitation, alcohol and nicotine are prohibited.
For pain and swelling after opening the ranula, Ibuprofen or Ketanov is prescribed.
Adequate dental care will help prevent recurrence.
If the problem lies in an incorrectly selected denture or chipped teeth, then dental care cannot be avoided.
During the healing stage and in order to prevent cyst formation, rinse your mouth with a soda solution. For a glass of warm boiled water, take 1/2 spoon of soda and the same amount of iodized salt. It is useful to rinse with decoctions of herbs such as chamomile, sage, immortelle, and calendula.
What is
A lump is a formation of varying size, formed from the upper layers of the mucous membrane. The neoplasm may be white or red, as well as a bluish tint. Inside the cavity there is content consisting of lymph, blood clots, pus or pathologically altered cells.
There may be several reasons for the formation of a tumor. Most often this is damage to the mucous membrane or the development of other diseases. That is why it is important to promptly establish the cause of its occurrence, before the pathological process spreads to other tissues of the oral cavity.
Treatment is carried out after diagnostic testing and exclusion of malignancy, since a lump in the sublingual area may appear as a result of the development of oncology.
Physiological reasons
The appearance of a lump under the tongue is not always a sign of a pathological process. In some cases, such a symptom appears for completely physiological reasons:
- causing injury to the oral mucosa - for example, when brushing your teeth with a brush with too hard bristles;
- ingestion of foods with hard, sharp edges - nut shells, fish bones;
- poor-quality dental services – tissue injury from sharp edges of dentures and implants.
Local swelling under the tongue - a lump - can also appear as a result of an individual reaction to any chemical substance that has entered the mouth, for example, a chemical gas. Less commonly, tissue inflammation resembling a lump can form for no apparent reason.
Establishing a full diagnosis is facilitated by a thorough history taking, laboratory and instrumental studies.
Diagnosis and treatment tactics
Differential diagnosis of a lump located in the space under the tongue involves a specialist conducting various laboratory and instrumental examinations:
- examining the tumor with a magnifying glass;
- collection of biomaterial for cell examination under a microscope;
- feeling the defect with your fingers - establishing the size of the lump, involving neighboring tissues in the pathological process;
- Ultrasound – examination of the formation using ultrasonic waves, which allows you to determine the true size of the tissue damage under the tongue;
- radiography - involvement of bone structures in the neoplasm;
- according to individual needs - in complex cases of lesions, CT or MRI are performed.
Treatment regimens for lumps in the tissues under the tongue directly depend on the true cause of the tumor. To eliminate the disease it is recommended:
- the use of rinses and anti-inflammatory drugs for mucosal injuries;
- vitamin therapy;
- physiotherapy;
- antitumor agents - for a benign or malignant process at the initial stage of the appearance of a lump.
The question of surgical removal of the lump under the tongue is considered by the doctor on an individual basis. However, most often such tactics of dealing with cones are justified - the resumption of the pathological process rarely occurs.
Saliva gland cyst
A tumor located directly under the tongue is a cyst. Inside, it is usually filled with serous fluid.
Based on the type and structure of the tissues, the lump can be:
- dermoid - looks like a kind of pimple under the tongue of a whitish or grayish tint, which causes anxiety to a person when swallowing food, as well as pronouncing words; the formation can only be removed surgically;
- mucous membrane - under the tongue a lump is no more than a centimeter in diameter, has a bluish tint, is almost always painless, and in most cases disappears on its own;
- ranula - reaches a significant size, is prone to repeated appearances after surgical excision.
Any type of cyst under the tongue requires observation and treatment by a doctor. Attempts to remove a lump on your own are dangerous due to infection and serious complications, including sepsis - blood poisoning, as well as gangrene - purulent inflammation of tissues.
Malignant sublingual tumor
Rapid and uncontrolled cell division in the sublingual area are the main signs of a cancerous tumor. In this case, the lump can reach enormous sizes and proceed in three directions:
- infiltrative - with expansion of the tumor inside the tissues under the tongue;
- papillary - along the surface of the oral mucosa;
- ulcerative - with the formation of a crate-shaped ulcerative defect on the surface of the cone.
At the initial stage of the appearance of a lump under the tongue, the tumor may not have any pronounced symptoms. The person continues to live in his usual way. However, as the size of the tumor increases and cancerous changes in the tissues intensify, the lump causes more and more discomfort to the patient.
Gradually, the tumor covers more and more areas of tissue under the tongue, spreading in thickness and depth. Then it spreads beyond one area and metastasizes - cancer cells move to the nearest lymph nodes and neighboring organs.
The treatment strategy for a malignant tumor under the tongue consists of surgical excision of the primary focus - the lump, followed by radiation and chemotherapy.
The prognosis is favorable only at the initial stage of a malignant tumor - if it is small in size, there are no metastases, and timely and comprehensive treatment is performed. Otherwise, due to late treatment, poor-quality treatment, or the patient’s failure to comply with the doctor’s recommendations, the lump comes out from under the tongue and occupies the entire oral cavity. A person dies from cancer intoxication.
Conditionally benign tumors
The formation of a growth under the tongue from tissues other than mucous can also be called a lump. Dentists distinguish the following types of conditionally benign tumors.
Lipoma - formed from adipose tissue cells located under the tongue. Education is benign. The cone has a dense capsule, inside of which there is soft tissue separated by bridges.
Papilloma is formed from epithelial cells. Visually it resembles an oval or round bump of a pale pink hue. Sometimes not one, but several similar formations form under the tongue. If injured, it can transform into a cancerous tumor.
Hemangioma - grows from blood vessels under the tongue. The lump appears to be a cavernous type of formation - convex in shape and size. However, it does not rise above the surrounding tissues under the tongue.
Lyphangioma is the formation of a warty structure with vesicles. Often inflamed when injured by pieces of food.
The fight against benign formations consists of their timely identification and surgical excision. The optimal methods of surgical intervention are determined by the doctor after analyzing all the information obtained on the basis of diagnostic procedures.