Alveoloplasty methods
Correction of the alveolar process
It is used before the start of rational prosthetics, for the convenience of the patient while wearing a removable denture.
Relocation of the inferior alveolar nerve
The operation is performed when there is not enough space to place an implant; this situation often occurs in the lower jaw.
Graft transplant
Transplantation - increasing the volume of the mucous membrane or bone tissue. The need for this method arises after the removal of teeth or anatomical features of the body in order to comply with the conditions for implantation.
Gingivosteoplasty
This method is used for periodontal diseases with varying degrees of severity. Gingivosteoplasty is intended to correct gum recession.
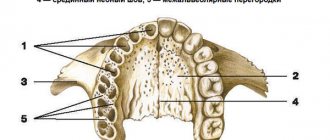
Atrophy and defect of the alveolar process/ridge of the jaw.
There are various reasons for the decrease in the volume of the alveolar process of the upper jaw and the alveolar part of the lower jaw. The main root cause of this pathology is tooth loss of various etiologies. Due to the lack of load on the area of the bone in which the tooth was previously located, its atrophy occurs. Also, in addition to atrophy, there are defects due to jaw injuries and congenital clefts of the alveolar process. The main problem with volume deficiency or alveolar ridge defect is unsatisfactory conditions for further prosthetics.
A modern method of eliminating dentition defects (missing teeth) is prosthetics supported by intraosseous dental implants. The reason for the popularization of this method was to stop bone tissue atrophy in the implantation zone, in contrast to removable prosthetics, in which bone volume continues to slowly decrease. The success of implantation directly depends on the volume of bone tissue, since in order to perform the chewing function, the implant needs good fixation in the bone.
To increase the volume or eliminate a defect in the alveolar crest of the lower jaw or the alveolar process of the upper jaw, transplantation of one’s own bone tissue (bone grafting) from various donor areas (rami and body of the lower jaw, mental region of the lower jaw, iliac crest, etc.) is used. which are chosen individually.
The surgical procedure consists of forming a bed for further transplantation of bone material in the area of atrophy or defect of the alveolar ridge or process, then the material itself is taken from the previously selected donor area (most often bone blocks from the lower jaw are used), after which the resulting bone fragment is modeled and fixed to the area of defect/atrophy. During these operations, all incisions are made in the oral cavity (except for cases in which the donor area is the iliac crest, in which case an additional incision is made in the iliac region 3-5 cm long).
In cases of atrophy of the alveolar process in the area of the chewing teeth of the upper jaw, the mucous membrane of the maxillary sinus can be lifted (sinus lift). The technique of this manipulation consists in creating access in the projection of the maxillary sinus (sinus) above the area of atrophy/defect of the alveolar process, then the mucous membrane of the sinus is carefully peeled off and lifted upward. Biomaterials of natural origin are placed into the resulting cavity, which serve as a matrix for new developing bone tissue. Quite often, dental implantation is performed simultaneously with this manipulation.
It is important to understand that the more time passes without qualified treatment, the greater the atrophy of bone tissue, and therefore the more complicated surgical treatment becomes.
Why is the procedure needed?
The alveolar process is the basis for holding the implant in the jaw bone. Due to the lack of chewing load, the bones gradually thin out and become looser, decreasing in size. This makes it difficult to securely fix the implant.
The longer you put off going to the dentist after losing teeth, the more difficult it is to restore your dentition by installing implants.
Implantation is also difficult to do if the jaws are deformed. It is provoked by neoplasms in the mouth, severe infectious diseases, and injuries of the maxillofacial apparatus.
Therefore, in case of atrophy and deformation of bone structures, bone grafting is prescribed before implantation, in particular, expansion of the alveolar ridge using the splitting method.
Jaw bone atrophy with age
One of the factors influencing the defect is age-related changes. As a rule, in patients over 60 years of age, atrophy is a common process. This is explained by the fact that the lack of minerals and cell nutrition affects metabolism and teeth fall out. The blood supply to bone tissue is disrupted and the required amount of oxygen is not supplied. This causes a change in pressure on the bone.
Types and degrees of jaw bone atrophy
Deformation of the jaw bone develops with different intensity:
- I degree. At the beginning of the disease, it is eliminated by prosthetics. The implant performs its function, the blood supply is not disrupted.
- II degree. The clinical picture is intensifying. The mucous membrane of the jaw begins to shrink. Dental prosthetics are possible, but additional treatment is required before this can be done.
- III degree. The contour of the bone tissue is smoothed both on the inside of the mouth and on the side of the chin.
When selecting a treatment method, this characteristic of the development of pathology should be taken into account. Bone tissue decreases not only in height, but also in width. The bone becomes short and thin.
Classification
After the unit is removed, the hole in place of the tooth narrows by about 30%. Then the process stops and enters the latent stage. Then there is a displacement of the row, the load on the jaw is distributed unevenly, which only worsens the condition. Depending on the course of this process, the anomaly is characterized using various parameters.
Classification according to Schroeder-Kurlyandsky:
- The processes and tubercles are pronounced, the palate is deep. In the first type, the transitional fold is located high. Integrity and structure are preserved.
- With a moderate degree, atrophy of the tubercles and process appears, the depth of the palate is average, as is the vestibule of the oral cavity. The mucous membrane becomes thinner, but is within normal limits.
- The third type is severe atrophy, in which the tubercles and process are absent, the palate becomes flat, the transitional fold and frenulum are attached low. The stage is considered advanced, the sky is flat.
Kepler classification:
- unexpressed stage with preservation of structure, favorable prognosis;
- progressive stage;
- hypoplasia, the distribution of pathology is uneven, atrophy is most strongly expressed in the area of the incisors, weaker in the areas of growth of the molar units.
Oxman classification:
- hypoplasia of the lower jaw, atrophy is almost not expressed;
- there are dystrophic lesions of all processes;
- pathology is destructive, disproportionate.
Treatment
To restore the appendix, various treatment methods are used, the choice of which depends on the degree of pathology and associated problems. The main methods are:
- process correction;
- change in the position of the infrasocket nerve;
- graft installation;
- Gingivosteoplasty.
Correction is a plastic surgery during which bone tissue is built up and compaction is performed in the area where the implant will subsequently be installed. The following methods are used for correction:
- Internal extension with tissue dissection, fracture and reinstallation of the bone wall. The resulting cavities are filled with biological substitutes, which strengthens the site for subsequent implantation. The bone chips that remain after the manipulation are placed in the area of the transplanted area.
- Overlay on the outer or inner part. First, the tissue is excised, the state of the blood flow and the possibility of closing the implant are checked.
When moving the nerve of the lower jaw, surgery is performed under local anesthesia. The method is recommended when bone destruction develops and the edge is located less than one centimeter from the nerve infrasocket branch.
Transplantation is recommended for severe atrophy, when other treatment methods do not provide a positive result. Depending on the condition, the doctor prescribes a transplant using the following methods:
- alloplastic using resin mixtures based on polymers;
- autoplastic with removal of excess and building up missing areas due to them;
- explantic with the use of intact metal plates, which are placed in the cavity with fastening of rods under the prosthesis (only removable dentures are used).
Cost of treatment
To calculate the cost of treatment, the doctor must conduct a preliminary examination and determine the severity of the pathology. On average, the cost includes the following services:
- gingivosteoplasty – 800-10,000 rubles (depending on complexity);
- correction – from 8400 rubles;
- displacement of the infralunar nerve – 6200 rubles or more;
- transplant installation – 4,000 rubles or more.
Atrophy can seriously worsen the condition, reduce the functionality of the jaws, and cause complications. Therefore, at the first signs of pathology, you should consult a doctor for examination and appropriate treatment.
About the method
Expansion of the alveolar process allows you to increase the volume of bone tissue in width (on average by 2 mm). With it, there is no need to transplant bone blocks, which are fixed on the outside of the cortical plate. Osteomaterial is added inside the process, due to which it grows with blood vessels, and accelerated formation of new bone tissue occurs. There are 2 methods used in dentistry:
- Split-Control.
All the doctor needs to do is cut the appendage, fill the resulting space with bone substitutes and sew up the gum. No patient grafts or biological material are required. It can be carried out as a separate stage before implantation or combined with the installation of implants. - Intercortical osteotomy
with block movement. Used less frequently. The essence of the method is to reconstruct the structure of the jaw tissue. The doctor saws through the alveolar ridge so that a movable fragment is formed, moves it to the area of maximum width of the defect, and fixes it with screws. The resulting space is filled with osteoplastic material. Implants are not installed at once, only 3-4 months after the implantation of the material.
Material and methods
In the period from 2016 to 2022, 18 patients aged from 6 to 60 years with a current diagnosis of a defect of the hard palate and/or alveolar process and oronasal anastomosis were operated on in the Department of Reconstructive, Plastic Maxillofacial Surgery of the Federal State Budgetary Institution "Central Research Institute of IIS and Maxillofacial Surgery", Surgical treatment was performed to cover the defect and oronasal anastomosis with a FAMM flap.
Most patients have a history of multiple operations for the underlying disease in the scope of primary uranoplasty, reuranoplasty, the number of previously undergone surgical interventions on the palate in this group of patients ranges from 1 to 8-10, and yet in all cases there was a recurrent residual defect coupled with cicatricial -changed surrounding tissues due to repeated surgical interventions, inflammatory and necrotic processes. The size of the defect from 3 to 40 mm, the need to separate two anatomical zones - the oral and nasal cavity / maxillary sinus, as well as the presence of a persistent inflammatory process in the nasal cavity / maxillary sinus dictated the need to bring in a sufficient amount of well-supplied tissue from another anatomical area.
The psychological and emotional state of these patients makes it a priority to choose a traumatic surgical intervention, without serious donor damage, an optimal surgical intervention in terms of time, with a minimization of the rehabilitation period associated with lower risks in case of failure.
At the first stage of treatment of such patients, the primary task is the reliable and effective elimination of the oronasal anastomosis with a soft tissue flap; in the future, patients are planned to undergo bone reconstruction followed by dentofacial rehabilitation.
In all 18 cases, to plan a flap in the projection of the facial artery, as an instrumental method of research, patients underwent duplex ultrasound scanning of facial vessels with determination of qualitative and quantitative characteristics of the facial arteries, which in 100% of cases helped to determine the localization of the facial artery in a typical place, as well as to register a satisfactory blood flow speed and vessel diameter.
In cases of extensive bilateral defects, CT angiography of the vessels of the face and neck was performed to visualize the bone edges and determine the true size of the defect, which is the most reliable method of preoperative diagnosis and precision flap planning.