General information
Jaw tumors refer to neoplasms in the cat's tissue. This pathology accounts for 13 to 29% of the total number of dental surgical diseases.
Due to its close location to the teeth, brain and eyes, the pathology is characterized by a special clinical course. Tumor formations in this area lead to functional disorders, aesthetic defects and even death.
Depending on the tissue of which the tumor is composed, it can be osteogenic or non-osteogenic. According to the clinical development of pathologies, there are malignant, benign or locally destructive.
Treatment of jaw tumors is a complex and lengthy task that requires high competence and professionalism from the doctor.
Causes
The cause of osteoma is said to be heredity, but its appearance and progression can also be facilitated by certain diseases, including gout, syphilis and rheumatism (the trigger is often trauma, especially repeated trauma). The pathology of calcium metabolism sometimes causes the development of inert tumors, the pathological development of embryonic cells can lead to the development of growths, and when localized in the nasal sinuses - a purulent complication or inflammation, puncture of the maxillary sinus. Ectostoses can form during puberty.
Reasons for development
The exact mechanism of tumor development is unknown. It is generally accepted that odontogenic tumors develop under the influence of malformations of jaw tissue.
Provoking factors:
- chronic inflammatory process of tissues of the jaws and adjacent organs;
- the impact of filling composition and other foreign objects on the maxillary sinus;
- damage to the jaw bones and soft tissues due to bruises and other mechanical impacts;
- the effect of nicotine, alcohol and other chemicals on the oral cavity.
Malignant tumors develop due to the spread of metastases from cancerous tumors in other organs.
Diagnostics
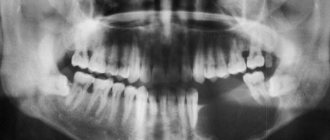
Diagnosis of the tumor is carried out to determine its type and location in order to select tactics for treating osteoma. As part of its implementation, X-ray and CT are used. The most informative is a 3D reconstruction; it shows all the details and outlines, as well as the extent of damage to surrounding tissues. In the process, it is important to differentiate osteoma from chronic Brody’s abscess, organized periosteal callus, osteochondrosis dissecans, osteogenic sarcoma, osteoperiostitis and other diseases.
Before prescribing an x-ray or tomography, the doctor conducts an examination and identifies:
- presence of pain when pressing;
- location;
- growth rate;
- functionality of the tissue that has been affected.
Using X-rays, a specialist detects the number of tumors, their structure, location, and the degree of bone destruction. It should be noted that on an x-ray the exostosis looks smaller than in reality, since its upper cartilaginous layer is not visible. In children it reaches a thickness of several centimeters. The benign nature of the tumor is indicated by correct geometry and structure, a clear contour, a small degree of calcification and growth at a low rate.
Classification and clinical course
Due to the variety of forms and stages, it is difficult to develop a unified classification of jaw tumors. The WHO classification provides for subdivision according to clinical manifestations, histology and anatomical location.
Clinical symptoms, course and prognosis are determined by the type, location and stage of the disease.
- Odontogenic benign
Ameloblastoma is a neoplasm that develops from epithelial cells with inclusions that resemble enamel in structure. Pathology affects people aged 20 to 40 years. As the tumor grows, the patient experiences pain in the jaw and teeth. An external examination reveals a dense structure, fusiform and painless thickening of the jaw bone, causing facial asymmetry. Mobility causes teeth to shift. There is a risk of developing suppuration in case of infection.
Odontomas are pathologies characteristic of children under 15 years of age. The tumor consists of hard tissue, including the pulp and periodontium. It is characterized by its small size and asymptomatic course. When it grows to large dimensions, it deforms the jaw, causing fistulas and pain.
Odontogenic fibroma is a childhood pathology that is formed from the connective tissue of the follicle and is located on both jaws. Characterized by slow, asymptomatic growth. Rarely manifested by aching pain and inflammation in the affected area. Subtype – cementing fibroma.
Cementoma is a formation of connective tissue growing into the cementum of the tooth root. The tumor is localized on the lower jaw in the area of the molars. Asymptomatic.
- Underontogenic benign
There are bone- and cartilage-forming types and osteoblastoclastoma. The list of bone-forming substances includes: osteoma, exostosis, osteophyte, etc.
Osteoma is a dense formation of mature bone tissue. It can be asymptomatic or with pronounced manifestations: pain during chewing, facial asymmetry, mobility of units.
Chondroma is a cartilaginous type of tumor. Localized in HF. It is characterized by slow growth and painlessness.
Osteoblastoclastoma is diagnosed in people under 20 years of age. Patients note a gradual increase in pain in the jaw, asymmetry of facial features, hyperthermia, and the occurrence of fistulas. There is a risk of developing fractures of the lower jaw.
- Malignant neoplasms
They occur 4 times less frequently than benign pathologies. They are odontogenic and non-odontogenic. They are characterized by severe symptoms, an aggressive course and a danger to life.
Osteogenic sarcoma. An aggressive tumor with rapid growth, pronounced pain, radiating to neighboring organs. The symmetry of the face is disrupted, infiltration of soft tissues and metastases to other organs are observed.
Carcinoma. It develops on the HF, growing into the nasal cavity. Purulent rhinitis and nosebleeds develop. When it grows into the orbit, lacrimation, exophaltmus and other complications are noted.
Diagnostics
Late diagnosis of neoplasms is due to the asymptomatic course and low oncological alertness of patients and doctors.
Diagnostic methods used:
- interviewing the patient and collecting anamnesis;
- clinical examination;
- X-ray diagnostics;
- CT;
- scintography;
- infrared thermography;
- biopsy.
If necessary, the doctor prescribes highly specialized examinations.
Treatment algorithm
When jaw tumors are detected, surgical treatment is required. The tumor is excised along with part of the adjacent healthy tissue. This reduces the risk of relapse and malignancy.
In some cases, the use of curettage is allowed. Teeth located in the problem area are subject to extraction.
Localization of tumors: in the body of the lower jaw or upper jaw
The clinical picture depends on the location of the tumor. When localized in the body of the lower jaw, the tumor can cause deformation of the jaw, and when the nerve is compressed, pain of a neuralgic nature. When localized on the coronoid process, as it grows, there is a gradual restriction of mouth opening and malocclusion.
On the upper maxillofacial bone, tumors are most often localized in the maxillary sinus. They usually have a spherical shape and a spongy structure. As it grows, the upper jaw is deformed, the eyeball is displaced and can cause diplopia, neuralgia of the second branch of the trigeminal nerve; if the second pair of cranial nerves is compressed, vision may decrease until it is completely lost.
Tumors can also occur in the nasal cavity and paranasal sinuses. On the radiograph, a shadow of a dense, compared to the surrounding bone, formation with sharply defined boundaries is noted in the bone - compact osteoma. With a spongy tumor, a disruption of the normal bone structure with alternating areas of rarefaction and compaction is determined.
A tumor of the maxillofacial bone can develop inside the bone tissue or manifest itself as superficial (exophytic) growth. This neoplasm can spread to the sinuses of the upper maxillofacial bone, the nasal cavity and the orbit. A tumor of the lower jaw can cause facial asymmetry and limitation of jaw mobility (up to complete). Diagnosis of jaw tumors involves x-ray examination, CT scan, scintigraphy; if necessary, consultation with an ophthalmologist, otolaryngologist, rhinoscopy.
As a tumor of the maxillofacial bone grows, it can cause jaw deformation, restricted mouth opening, and malocclusion. In the upper maxillofacial bone, it can also cause deformation and even lead to visual impairment.
Treatment
If, during an X-ray examination for some other problem, the doctor discovered the presence of this benign formation, this does not necessarily mean that it is necessary to remove the osteoma. Its removal is carried out under general anesthesia through the oral cavity, so there are no visible scars or scars. After removal, a mandatory histological examination is carried out in order to exclude the malignant nature of the formation. Surgical intervention for osteoma is carried out only when a cosmetic defect or functional inconvenience occurs.
The operation is performed when osteoma disrupts any functions, makes prosthetics difficult, deforms, etc. The tumor is usually removed using intraoral access. After the formation of the mucoperiosteal flap, a series of pinholes are created around the circumference of the formation and the tumor is removed with a chisel. Next, grinding is carried out to eliminate irregularities. After hemostasis, the wound is sutured tightly. Tumor-like formations that develop in the jaw bones and are most often encountered in the practice of a dental surgeon include odontogenic cysts and exostoses.
The Center for Oral and Maxillofacial Surgery and Implantology has its own comfortable hospital with operating rooms equipped with the most modern medical, dental and anesthesiological equipment and comfortable wards. The Center's surgeons and anesthesiologists have extensive experience in performing such operations and guarantee complete patient satisfaction with the results of treatment.
Symptoms
The moment of appearance of osteoma and the moment of appearance of the first symptoms diverge in time, i.e. the tumor may not show clinical symptoms for a long time.
When it reaches a significant size, the following signs appear:
- The appearance of a compaction in the jaw area, often smooth to the touch, less often lumpy;
- Pain due to compression of the nerves by the tumor (headaches and other diseases associated with the nervous system occur);
- Facial asymmetry and swelling, unnatural shape of the jaw itself;
- Malocclusion (improper closing of the jaws);
- Limited (partial or complete) movement of the lower jaw. The larger the tumor, the more difficult it is for the patient to move the jaw. The patient notes the inability to open his mouth wide;
- Painfulness of an advanced stage tumor when palpated;
- Breathing problems through the nose;
- Impaired eye mobility on the side where the tumor is located.
Causes
The exact causes of osteoma remain unclear to this day, and existing theories of the origin of osteomas from the periosteum of mature bone or remnants of embryonic cartilage do not provide an exhaustive answer to all questions. Some authors associate the occurrence of osteomas with frequent injuries to bone tissue and previous inflammatory processes.
Presumably, factors contributing to the development of osteomas are: genetic predisposition, inflammation/previous infections and diseases ( rheumatism , syphilis , gout ), hypothermia.
The reasons for the development of osteoid osteoma have also not been studied. Some authors consider this type of tumor as chronic non-purulent focal necrotizing osteomyelitis , while other authors classify it as a tumor.
Types of osteoma
Osteomas are dense formations of the bone structure, most often located inside the skull, where they reach sizes of 1-4 cm. They are less common on the surface of other bones; if they appear, they become larger. A type of osteoma is osteoid osteoma. Like osteoma, osteoid osteoma is a benign bone tumor. It differs in location because it most often concerns the long bones and bones of the pelvis or scapula. It also happens to occur inside the vertebrae. Osteoid osteoma does not exceed a few centimeters in diameter and most often occurs in young men. A very characteristic feature of this neoplasm is the occurrence of pain after exercise, during night rest and pain relief under the influence of salicylates.
Another type of osteoma is osteoblastoma, a rare primary bone cancer. Most often this is a benign tumor, but in the literature there are cases where osteochondritis showed an aggressive course, reminiscent of bone sarcomas (malignant tumors).
This type of cancer is located in the long bones and bony parts of the spine. As with osteoid osteoma, patients with osteoblastoma do experience bone pain that does not go away with medication. The tumor grows larger than other types of osteomas and is most common in young people.
Factors
There is a consensus among experts on the question “what are the reasons for the formation of such a tumor?” does not exist. It is argued that there is a connection between osteoma of the jaw and a number of factors. These include:
- Trauma to the maxillofacial bones, chronic or one-time (bruise, damage to the integrity of the oral mucosa, untreated teeth (which caused them to quickly collapse), tartar (hard dental deposits), dentures and dental implant crowns that change the bite (poorly fitted) ), poor surface treatment of dental fillings that do not allow the jaws to fully close).
- Inflammation in the area of the nose and jaw (actinomycosis, sinusitis, periodontitis, osteomyelitis, periostitis, sinusitis and other pathologies), chronic or acute.
- Aggressive environmental effects (smoking, chemical, ionizing and radioactive exposure).
- Foreign particles in the sinuses above the upper jaw (often fragments of teeth or particles of materials used to fill teeth).
Experts do not classify osteoma itself as an odontogenic disease. But there are factors that provoke the appearance of a tumor.
Rehabilitation and prognosis
The recovery period after surgical intervention in the lower/upper jaw - excision of osteoma - is usually favorable. If the lesion is small, no dental correction is required, since the bite is not disturbed. It is enough for a person to eat right and lead a healthy lifestyle. The prognosis is favorable.
If the osteoma has reached a large size and the intervention area is significant, the dentist will subsequently recommend dental implantation so that you can chew food. Rehabilitation periods are lengthened. Nevertheless, the prognosis remains favorable - such tumors rarely degenerate into cancer. It is enough to follow all the doctor’s recommendations, give up bad habits and undergo regular jaw checkups.
What is osteoma?
Osteoma is a benign bone tumor, most often localized in the flat bones of the craniofacial side, but also occurs in the ribs, pelvis and long bones. Sometimes osteomas develop inside the bones that make up the paranasal sinuses, protruding into them, which leads to obstruction of the sinuses. Osteoma usually occurs between the ages of 40 and 50, and is twice as common in men. On average, bone cubes reach several centimeters in diameter. Most often, they form a solid, clearly defined mass of bone consistency that does not cause any unpleasant symptoms.
Osteomas are characteristic of a genetic disorder called Gardner syndrome.
Patients with this syndrome suffer from multiple colon polyps, often accompanied by osteomas (usually in the jaw area). To date, the causes of osteomas have not been identified, but the influence of inheritance of mutant genes is often mentioned.
Symptoms of osteoma
The symptoms of osteomas depend on their location and size. Very often they are asymptomatic. During physical examination, changes are felt that are located closer to the skin - these are solid formations with the consistency of bones, well separated from the surrounding tissues. When the paranasal sinuses are affected, symptoms occur that resemble inflammation in the nature of pain and distraction. If the tumor grows in size or develops near the orbit, unilateral proptosis may develop. The presence of a tumor extending into the sinus air space can also obstruct sinus passage and lead to recurrent sinus inflammation.
Tumors can occur near cranial or spinal nerves. In such situations, numerous neurological symptoms occur, the nature of which depends on the pressure on a particular nerve.
Treatment tactics
Despite the benign nature of most osteomas in the lower jaw, once a pathological focus is identified, it should be removed immediately. Pharmacy products or traditional medicine recipes are not able to cope with the progression of the tumor or slow down its growth and development. Oncologist surgeons treat such diseases.
Indications for emergency medical intervention:
- severe pain syndrome;
- suspicion of the appearance of cancer cells in the lesion;
- rapid tumor growth;
- severe jaw movement disorders.
Surgical excision occurs after cutting the tissue and gaining access to the tumor. The doctor performs all manipulations after the patient has fallen asleep from general anesthesia. In addition to the osteoma itself, some healthy tissue must be excised to prevent relapse of the disease.
Since this results in the formation of a kind of defect—a void in the bone—it is necessary to perform plastic surgery—to fill the defect with the patient’s own cells or with an artificial implant. Typically, surgeons perform both actions in one operation.
Treatment
Removal of osteoma is indicated if it compresses neighboring organs, is visible visually, that is, acts as a cosmetic defect (especially on the face and head), changes the shape of bones, reduces mobility, leads to scoliosis, and causes pain. Most often, tumors are removed from the sinuses, ear canal, jaws, knee and hip joints.
If the tumor does not manifest itself in any way and does not cause discomfort, the doctor observes it and evaluates its growth rate. A small osteoma that has stopped growing does not need to be removed or treated.
The operation to remove the tumor is performed by maxillofacial surgeons or neurosurgeons. During the operation, the doctor cuts the tissue, removes the growth and part of the bone/tissue around it to avoid relapse.
The doctor will suggest removing the osteoma in the following ways:
- complete excision – used for tumors in the sphenoid sinus;
- curettage - an incision in the skin, removal of a tumor, cleansing the lesion by curettage;
- endoscopic removal - suitable for small tumors with a difficult approach, used using computed tomography to monitor the progress of the operation and a radiofrequency probe, takes about 2 hours.
Tumor recurrence occurs in 10% of cases due to incomplete removal. To exclude this possibility, you need to choose a good clinic and specialist.
Diagnosis and differentiation
When a person discovers a lump in the lower or upper jaw, he must see a specialist. This is a pathology where it is impossible to diagnose or treat it on your own. Patients often come to specialists at an advanced stage, when osteoma has affected large areas of the jaw. It happens that the tumor is found by an ENT doctor during a standard appointment.
To diagnose osteoma of the upper and lower jaw, there are the following methods:
- Collection and analysis of information about the disease (history) based on a conversation with the patient;
- Visual inspection and palpation. The doctor determines the size of the osteoma itself, location, appearance;
- X-ray of the jaw. In the picture, osteoma is a spherical or oval compaction with a noticeable border. If images of the tumor and tooth root are combined, then osteoma is confused with odontoma. The compact peripheral appearance of osteoma is easily diagnosed (it is mainly located on the outer side of the lower jaw). A tumor located on cancellous bone tissue has a heterogeneous color in the image, because it has a heterogeneous structure, having different densities in different areas;
- Computed tomogram of the maxillofacial apparatus;
- Scintigraphy (used if x-ray examination does not help determine an accurate diagnosis);
- Biopsy of tumor tissue. Used to determine the degree of danger of osteoma;
- Biopsy of the inflamed lymph node under the jaw (near the place where the tumor is located);
- Consultation and examination with an ENT doctor and an ophthalmologist (more often with osteoma of the upper jaw, when the tumor reaches the bones of the orbit and nasal sinuses);
- Phonoscopy and rhinoscopy (more often necessary for maxillary osteoma);
- Puncture of the sinuses (if necessary);
- Maxillary sinusotomy (if necessary).
The main task of the doctor at the examination stage is to determine an accurate diagnosis, that is, to differentiate osteoma of the jaw from other neoplasms and pathologies:
- Hyperostosis (excessive accumulation of bone substance in unchanged bone tissue, inflammation of the periosteum);
- Odontoma (a benign tumor consisting of pathologically growing dental tissue; purulent fistulas sometimes appear);
- Osteoid osteoma (differing in cell composition, but being a benign tumor);
- Fibrous osteodysplasia (a defect in the growth and development of bone tissue; on an x-ray it looks like a spongy osteoma; it develops in childhood, adolescence, when the body (including bones) is still growing);
- Chondroma (similar to spongy osteoma; consists of mature cartilaginous cells; is rarely formed in the jaw bones, more often localized in the tubular bones of the arms; can transform into chondrosarcoma, malignant in nature);
- Intraosseous sclerosis (does not have a clear boundary between healthy cells and diseased cells; bone tissue becomes excessively dense and interferes with normal blood flow);
- Salivary stone (the main difference is severe pain when the salivary duct is blocked by a stone; the pathology is typical for people with chronic diseases (diabetes mellitus, urolithiasis, gout), lack of vitamin A and excess vitamin D);
- Osteoid-osteoma (a distinctive feature is pain from the moment the tumor appears, intensifying at night; a small tumor that does not deform the bone);
- Exastosis (in the X-ray image it does not differ from osteoma, it has clearly visible boundaries).
Treatment of osteoma and prognosis
If the tumors are small and do not cause symptoms, it is enough to observe the development of the tumor. In other cases, treatment consists of surgical removal of the tumor. During the procedure, it may turn out that in order to completely get rid of osteoma, it is necessary to remove fragments of healthy bone. These cavities are then filled with special materials, most often titanium plates. In some cases of osteomas from the cranial region, it is possible to perform the procedure through a less invasive transnasal approach using the endoscopic method. Osteomas are benign formations, so the prognosis is good. These tumors do not metastasize to distant tissues, and their harmful effects mainly depend on their location.