General information
Jaw tumors refer to neoplasms in the cat's tissue. This pathology accounts for 13 to 29% of the total number of dental surgical diseases.
Due to its close location to the teeth, brain and eyes, the pathology is characterized by a special clinical course. Tumor formations in this area lead to functional disorders, aesthetic defects and even death.
Depending on the tissue of which the tumor is composed, it can be osteogenic or non-osteogenic. According to the clinical development of pathologies, there are malignant, benign or locally destructive.
Treatment of jaw tumors is a complex and lengthy task that requires high competence and professionalism from the doctor.
Osteoblastoclastoma - microscopic picture
Microscopically, in osteoblastoclastoma, a large number of small, slightly elongated cells with a rounded nucleus (such as osteoblasts) are distinguished, among which massive accumulations of giant multinucleated cells (osteoclasts) are identified. In mononuclear cells, mitoses are observed; in multinucleated cells, they are absent. The formed elements of the tumor are also represented by fibroblasts and xanthoma cells. Areas of hemorrhage undergo a macrophage reaction with the corresponding phagocytic cells. In some areas of the tumor, islands of osteoid tissue are found. The tumor is saturated with decayed red blood cells and is imbibed by the blood pigment - hemosiderin, which gives it a brown color. The presence of the latter and multiple hemorrhages, often in the form of blood cysts, is due to the peculiarity of blood flow in the tumor.
Blood in osteoblastoclastoma circulates outside the vascular bed through intertissue gaps. The absence of endothelium allows it to penetrate the tumor tissue and accumulate there. In this case, the formed elements of the blood are destroyed, forming an accumulation of hemosiderin. Sometimes an abundance of fibrous tissue may be found in the tumor.
Reasons for development
The exact mechanism of tumor development is unknown. It is generally accepted that odontogenic tumors develop under the influence of malformations of jaw tissue.
Provoking factors:
- chronic inflammatory process of tissues of the jaws and adjacent organs;
- the impact of filling composition and other foreign objects on the maxillary sinus;
- damage to the jaw bones and soft tissues due to bruises and other mechanical impacts;
- the effect of nicotine, alcohol and other chemicals on the oral cavity.
Malignant tumors develop due to the spread of metastases from cancerous tumors in other organs.
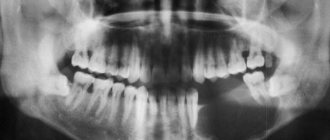
Osteoblastoclastoma - X-ray picture
Radiologically, with a cellular form of a tumor, a shadow from many small and larger cavities or cellular formations, separated from each other by bone partitions of varying thickness, is noted at the site of the lesion. No reaction from the periosteum is observed. The picture is in many ways similar to the X-ray picture of ameloblastoma.
The cystic form on the radiograph resembles an odontogenic jaw cyst and ameloblastoma. The difference between the cystic form of ameloblastoma is that its border with the bone often has fine scalloped outlines in the form of extremely small bays.
In the lytic form of osteoblastoclastoma, the tumor produces a structureless focus of clearing.
Classification and clinical course
Due to the variety of forms and stages, it is difficult to develop a unified classification of jaw tumors. The WHO classification provides for subdivision according to clinical manifestations, histology and anatomical location.
Clinical symptoms, course and prognosis are determined by the type, location and stage of the disease.
- Odontogenic benign
Ameloblastoma is a neoplasm that develops from epithelial cells with inclusions that resemble enamel in structure. Pathology affects people aged 20 to 40 years. As the tumor grows, the patient experiences pain in the jaw and teeth. An external examination reveals a dense structure, fusiform and painless thickening of the jaw bone, causing facial asymmetry. Mobility causes teeth to shift. There is a risk of developing suppuration in case of infection.
Odontomas are pathologies characteristic of children under 15 years of age. The tumor consists of hard tissue, including the pulp and periodontium. It is characterized by its small size and asymptomatic course. When it grows to large dimensions, it deforms the jaw, causing fistulas and pain.
Odontogenic fibroma is a childhood pathology that is formed from the connective tissue of the follicle and is located on both jaws. Characterized by slow, asymptomatic growth. Rarely manifested by aching pain and inflammation in the affected area. Subtype – cementing fibroma.
Cementoma is a formation of connective tissue growing into the cementum of the tooth root. The tumor is localized on the lower jaw in the area of the molars. Asymptomatic.
- Underontogenic benign
There are bone- and cartilage-forming types and osteoblastoclastoma. The list of bone-forming substances includes: osteoma, exostosis, osteophyte, etc.
Osteoma is a dense formation of mature bone tissue. It can be asymptomatic or with pronounced manifestations: pain during chewing, facial asymmetry, mobility of units.
Chondroma is a cartilaginous type of tumor. Localized in HF. It is characterized by slow growth and painlessness.
Osteoblastoclastoma is diagnosed in people under 20 years of age. Patients note a gradual increase in pain in the jaw, asymmetry of facial features, hyperthermia, and the occurrence of fistulas. There is a risk of developing fractures of the lower jaw.
- Malignant neoplasms
They occur 4 times less frequently than benign pathologies. They are odontogenic and non-odontogenic. They are characterized by severe symptoms, an aggressive course and a danger to life.
Osteogenic sarcoma. An aggressive tumor with rapid growth, pronounced pain, radiating to neighboring organs. The symmetry of the face is disrupted, infiltration of soft tissues and metastases to other organs are observed.
Carcinoma. It develops on the HF, growing into the nasal cavity. Purulent rhinitis and nosebleeds develop. When it grows into the orbit, lacrimation, exophaltmus and other complications are noted.
Diagnostics
Late diagnosis of neoplasms is due to the asymptomatic course and low oncological alertness of patients and doctors.
Diagnostic methods used:
- interviewing the patient and collecting anamnesis;
- clinical examination;
- X-ray diagnostics;
- CT;
- scintography;
- infrared thermography;
- biopsy.
If necessary, the doctor prescribes highly specialized examinations.
Treatment algorithm
When jaw tumors are detected, surgical treatment is required. The tumor is excised along with part of the adjacent healthy tissue. This reduces the risk of relapse and malignancy.
In some cases, the use of curettage is allowed. Teeth located in the problem area are subject to extraction.
Malignant tumors of the lower jaw
Before treating malignant tumors of the lower jaw, it is necessary to sanitize the oral cavity. If the patient is to be exposed to radiation, the metal prostheses should be removed, or better yet, isolated with a plastic mouth guard.
The choice of treatment method depends on the type, location, extent of the tumor, age and general condition of the patient.
Cancer of the lower jaw is treated mainly with a combined method, which is also indicated for Ewing sarcomas, reticulosarcoma and hemangioendothelioma. But it should be borne in mind that with Ewing’s sarcoma, even after combined treatment, the prognosis is poor. Treatment of osteogenic and chondrosarcomas, which are radioresistant, is surgical.
In a combined treatment regimen for malignant tumors of the lower jaw, a preoperative course of remote gamma therapy is first carried out. Sessions are daily, the number of radiation fields depends on the size of the lesion and the presence of regional metastases. The total focal dose per course is 40-50 Gy (4000-5000 rad).
The surgical stage is performed 3 weeks after completion of radiation therapy. During this time, radiation reactions occur on the skin and mucous membrane of the oral cavity.
Before surgery, taking into account clinical, radiological and morphological data, you should consider its volume, the method of fixation of the remaining jaw fragment, and the possibility of performing primary bone grafting of the jaw defect. It is also necessary to take into account the presence or absence of regional metastases. We must remember that the primary task of the surgeon is radical removal of the tumor. Therefore, if one-stage plastic surgery is impossible without compromising the radicality of the operation, it should be postponed. Paches A.I. In general, he believes that bone grafting of a defect after resection of the lower jaw for a malignant tumor should be performed no earlier than 2 years after treatment in the absence of relapse and metastases.
Surgeries for malignant tumors of the lower jaw (resections) can be of several types:
- resections with disruption of the continuity of the lower jaw (segmental);
- resections without breaking the continuity of the lower jaw (segmental);
- segmental resection of the lower jaw with disarticulation;
- half resection of the lower jaw with disarticulation;
- resection of the lower jaw (one of the options) with soft tissues.
When choosing the type of surgical intervention, you should remember the possibility of a malignant tumor growing into surrounding organs and tissues: the floor of the mouth, tongue, palatine arches and tonsils, lower lip, skin of the chin, submandibular salivary glands, parotid salivary glands. In this case, the scope of the operation must be expanded to include a block of tissue removed, organs affected by the tumor. In addition, primary malignant tumors of the mandible can spread along the neurovascular bundle in the mandibular canal. Experience shows that even with superficial damage to the alveolar process or the lower edge of the mandible (if regional metastasis spreads to the bone), it is not worth performing resection while maintaining the continuity of the organ, because this is fraught with relapse.
If the neurovascular bundle is involved in the tumor process, resection with disarticulation is indicated.
If the tumor is localized in the chin area, resection is performed from angle to angle of the jaw.
If the tumor is localized in the body area, resection is performed from the middle of the chin to the mandibular foramen.
If the angle of the mandible is affected, half resection with disarticulation is indicated.
According to Kabakov B.D. et al., 1978, resection of the lower jaw while maintaining continuity is very controversial and can be indicated for secondary cancer, when the mucous membrane is affected and there are only initial bone lesions. It must be remembered that the desire to simultaneously preserve the function and appearance of patients with any location of a malignant tumor is fraught with its relapse.
Resection of the lower jaw is performed under endotracheal anesthesia. Resection of the jaw without disarticulation is technically easier.
Technique of half resection of the lower jaw
The patient lies on the operating table with his head turned in the direction opposite to the affected one. An incision is made in the skin and subcutaneous tissue from the middle of the chin to the mastoid process 1.5-2.0 cm below the level of the lower edge of the lower jaw. For a better view, you can additionally make a midline incision in the lower lip. Then the mucous membrane of the vestibule of the oral cavity is dissected to the branch, 2 cm away from the tumor infiltrate. The buccal flap is separated within the incision with a scalpel and scissors. An incision is made in the mucous membrane along the alveolar process from the lingual side from the frenulum of the tongue (at the point of attachment to the lower jaw) to the angle. The soft tissues are carefully separated so as not to damage the tumor. The central incisor on the affected side is removed. At the level of the socket of this tooth, a Jig-li saw is carried out and, protecting the soft tissues with Farabeuf hooks, the lower jaw is sawed in the frontal region. The assistant uses a hook to move the jaw down.
The next stage of the operation is the separation of soft tissues in the area of the jaw branch. To do this, the masticatory and internal pterygoid muscles are cut off from the jaw, and the neurovascular bundle is crossed between two ligatures above the mandibular foramen. An osteotomy of the branch is performed using a Gigli saw. When performing an osteotomy of the lower jaw, the doctor should be guided by the radiograph and retreat from the boundaries of the lesion visible in the image by 3-4 cm.
The removed tumor should be sent for histological examination. The wound is carefully examined, washed with antiseptics and, after hemostasis, sutured in several rows with catgut and lesa.
At this stage, it is important to take into account reliable separation of the wound from the oral cavity, otherwise the wound may become infected with the contents of the oral cavity, which leads to failure of the sutures and the formation of a large defect. To prevent the cutting of sutures in the mouth, immediately after osteotomy of the lower jaw, its stump must be smoothed with a milling cutter, and during suturing, carefully covered with soft tissues.
Resection of the lower jaw with disarticulation
All stages of the operation are performed as described above. After lowering the lower jaw and cutting off the neurovascular bundle, the tendon of the temporal muscle and the external pterygoid muscle in the area of the condylar process are cut off from the coronoid process. After this, they begin careful dislocation movements, avoiding fracture of the jaw and damage to the tumor, since this leads to contamination of the wound with tumor cells. Suturing the wound begins with the oral mucosa.
If surgery on the regional lymphatic system is indicated, then lymphadenectomy is first performed, and at the final stage the lower jaw is included in the block of tissue removed. This guarantees the ablastic nature of the intervention.
It is very important in the postoperative period to keep the jaw fragments in the correct position. For this purpose, Tigerstedt and Weber splints with one or two inclined planes are used, less often - Vankevich or Stepanov splints, and the Rudko apparatus.
When resection of the frontal fragment of the lower jaw with tissues of the floor of the mouth, the operation often begins with the application of a tracheostomy. When part of the tongue is included in the block of tissue to be removed, tube feeding is indicated
Rehabilitation of patients
Restoring the anatomical integrity of the lower jaw, and thereby function and appearance, is a complex and controversial issue. Plastic surgery of a bone defect is a complex operation, which in a cancer patient weakened by previous treatment may end in failure, since the regenerative abilities of the tissues are sharply reduced. With malignant tumors, even after radical treatment, relapses are possible.
Some surgeons resort to primary bone grafting only after resection of small tumors that do not extend beyond the bone, because otherwise it is impossible to create a good receptive bed for the graft.
To hold jaw fragments in the correct position, implants are recommended to use various designs that approximate the shape of the missing area of the jaw. In this case, materials indifferent to body tissues are used: plastic, stainless steel, tantalum, Vitaly. It should be taken into account that these devices do not always provide rigid fixation of jaw fragments and can cut through soft tissue. Then they need to be removed and replaced with a tire.
Secondary plastic surgery of the defect after resection of the lower jaw, according to the recommendation of A.I. Paches, should be performed no earlier than 2 years later in the absence of relapse and metastases. It is carried out using both a preserved graft (which is preferable, since it eliminates the operation of taking an autograft from a weakened patient) and an autograft.
When planning reconstructive operations in this group of patients, the doctor must carefully consider the method of fixation of the lower jaw.
Prognosis for a malignant tumor of the lower jaw
The results of treatment of malignant tumors of the lower jaw are unsatisfactory. A 5-year cure after combined and isolated surgical treatment is observed only in 20-30% of patients. The results obtained after removal of sarcomas are even worse, and a 5-year cure occurs in less than 20% of patients.
Relapses of malignant tumors of the lower jaw usually occur in the first 1 to 2 years after treatment. Tumors of this location are insensitive to chemotherapy. The main reason for the high mortality rate of patients with this tumor location is late diagnosis and untimely initiation of treatment.
If patients are cured, their ability to work, as a rule, decreases, but some patients get the opportunity to return to their previous profession. Such patients themselves raise the question of plastic surgery within a few months after discharge from the hospital.
Treatment
Neoplasms of the jaws, regardless of type, are treated by complete removal. In the case of a malignant tumor, chemotherapy and radiation are prescribed in parallel with surgery.
When a tumor is diagnosed early, its removal is accompanied by minor losses of healthy tissue, while in later stages a massive resection of the jaw may be required, up to its complete removal followed by prosthetics. In addition, a complication of tumors is often tooth loss or loss of functionality of the entire dentition.
Timely detection of pathology reduces the risk of complications and has a favorable outcome even in the case of a malignant neoplasm, therefore regular preventive examinations are the main way to prevent the development of oncological processes.
Osteoblastoclastoma - differential diagnosis
Osteoblastoclastoma (cystic and cellular forms) must be differentiated from ameloblastoma and radicular cyst, the lytic form - from osteogenic sarcoma (in contrast to osteolytic sarcoma, thinning and swelling of the cortical layer of the jaw are noted in osteoblastoclastoma) and fibrous osteodysplasia (characterized by slow growth and preservation of the continuity of the cortical layer on the radiograph). layer of the jaw), fibromyxoma, central fibromas of the jaws.
Clinical and radiological examination without histological comparison is sometimes insufficient to establish an accurate diagnosis of osteoblastoclastoma. The frequency of discrepancy between the clinical diagnosis and pathohistological diagnosis is 30%; the most common discrepancies arise when differentiating osteoblastoclastoma from ameloblastoma - 16%
Symptoms of osteoblastoclastoma of the jaw
This tumor can develop asymptomatically for a long time, especially if it is centrally localized. The growth of the tumor leads to the appearance of symptoms such as:
- violation of facial symmetry;
- the appearance of pain in the affected area;
- the appearance of signs of inflammation of the soft tissues adjacent to the tumor;
- with prolonged development - the formation of ulcers and fistulas with purulent discharge in the oral cavity, and in some cases on the skin of the face.
Typically, the asymptomatic development of osteoblastoclastoma lasts from three to ten years. The patient does not have any complaints, and the tumor is discovered by chance - for example, during a general examination. Rapid and aggressive growth of this neoplasm occurs very rarely.